The Value of Arterial Sheath Placement Prior to Caesarean Section for Major Placenta Praevia
ORIGINAL ARTICLE
Hong Kong J Radiol 2023 Dec;26(4):255-9 | Epub 18 Dec 2023
The Value of Arterial Sheath Placement Prior to Caesarean Section for Major Placenta Praevia
W Shu1, AHC Wong2, LW Chan1
1 Obstetrics and Gynaecology Clinic, Gleneagles Hospital Hong Kong, Hong Kong SAR, China
2 Department of Radiology, Pamela Youde Nethersole Eastern Hospital, Hong Kong SAR, China
Correspondence: Dr W Shu, Obstetrics and Gynaecology Clinic, Gleneagles Hospital Hong Kong, Hong Kong SAR, China. Email: wendy.shu@gleneagles.hk
Submitted: 30 Apr 2022; Accepted: 25 Aug 2022.
Contributors: All authors designed the study, acquired and analysed the data, drafted the manuscript, and critically revised the manuscript for important intellectual content. All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of Interest: All authors have disclosed no conflicts of interest.
Funding/Support: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data Availability: All data generated or analysed during the present study are available from the corresponding author on reasonable request.
Ethics Approval: The research was approved by the Hong Kong East Cluster Research Ethics Committee of Hospital Authority, Hong Kong (Ref No.: HKECREC-2020-136).
Acknowledgement: The authors thank Mr Steve LT Lee, senior radiographer of Pamela Youde Nethersole Eastern Hospital, for retrieving data of cases who had femoral sheath inserted at the radiology department of the institution, and Mr Robert Porsch for advising on statistical analysis.
Abstract
Introduction
This study aims to assess the value of non-urgent femoral sheath placement in women with major placenta praevia by analysing its utilisation rate and associated outcome measures.
Methods
We performed a 10-year retrospective cohort analysis of cases of women who underwent elective Caesarean section for major placenta praevia in a single obstetric unit. We compared outcomes between those with preoperative femoral sheath placement to those not receiving a sheath.
Results
One hundred and forty-five women with major placenta praevia were enrolled. Femoral sheaths were placed in 70 cases, and 7.1% experienced successful uterine artery embolisation. The complication rate of femoral sheath placement was low (1.4%). The odds of receiving additional uterotonics were higher in the femoral sheath placement group (odds ratio = 5.44; p = 0.013). Femoral sheath placement was not associated with reduced blood loss, need for blood transfusion, operation duration, or the use of additional procedures to abate bleeding. The rate of intensive care unit admissions was comparable in both groups.
Conclusion
The placement of femoral arterial sheath prior to elective Caesarean section in cases of major placenta praevia may not be beneficial. It is time-consuming and does not improve maternal morbidity.
Key Words: Arterial; Caesarean section; Maternal mortality; Placenta praevia
中文摘要
剖腹產前放置動脈鞘對於嚴重前置胎盤的價值
舒敏欣、黃可澄、陳連偉
簡介
本研究透過分析使用率和相關結果指標,評估非緊急股動脈鞘放置對於嚴重前置胎盤孕產婦的價值。
方法
我們對一間產科因嚴重前置胎盤而接受擇期剖腹產的女性病例進行了10年回顧性隊列分析,並比較術前放置與未放置股動脈鞘患者的結果。
結果
共145名患有嚴重前置胎盤的女性納入研究,70例放置股動脈鞘,7.1%子宮動脈栓塞成功。股動脈鞘置入術的併發症發生率較低(1.4%)。股動脈鞘置入組接受額外子宮收縮劑子宮收縮的機率較高(優勢比 = 5.44;p = 0.013)。股動脈鞘放置與失血量減少、輸血需求、手術時間或使用其他方案來減少出血無關。兩組的加護病房入院率相若。
結論
對於嚴重前置胎盤的病例,在擇期剖腹產前放置股動脈鞘可能沒有好處。它耗時並且不會改善孕產婦發病率。
INTRODUCTION
The global prevalence of placenta praevia (PP) is
approximately 5 per 1,000 pregnancies, with the highest
prevalence reported in Asian women (12.2 per 1,000
pregnancies).[1] Delivery by Caesarean section in these
cases are 12 times more likely to result in massive
haemorrhage than Caesarean sections performed for
other reasons.[2]
Preoperative measures in minimising haemorrhagic
morbidities for these women can be achieved by closely
liaising with blood bank specialists, haematologists,
and interventional radiologists.[3] It has been suggested
that interventional radiology with uterine artery
embolisation (UAE), performed intraoperatively or
postoperatively, has reduced the need for hysterectomy
when pharmacological measures have failed.[4] [5]
In 2017, Luo et al[6] advocated prophylactic intraoperative
aortic balloon insertion with major PP, irrespective of
the presence or absence of abnormal invasive placenta.
However, a recent randomised controlled trial showed
that prophylactic internal iliac artery balloon occlusion
did not reduce postpartum haemorrhage (PPH) or have
any effect on maternal or neonatal morbidity in this
group of women.[7]
Prophylactic placement of femoral arterial catheters
(or sheaths) for PP is becoming more widespread.[8] In
our centre, femoral arterial sheath placement before Caesarean section for major PP is a common practice.
We explored the value of femoral sheath placement in
the management of PP.
METHODS
This was a 10-year retrospective observational analysis of all women with major PP delivered electively at
our centre from January 2010 to December 2020.
Anonymous data were collected from the Clinical Data
Analysis and Reporting System, a computer-based
administration database that records all the diagnostic
and procedural coding of admitted patients, and cases
were identified based on their diagnostic coding (10th
edition of the International Classification of Diseases[9]).
Missing data were retrieved manually from hard copies
of the patients’ records.
Major PP is defined by placenta covering the internal
os either partially (grade III) or completely (grade IV).[10]
The main bulk of the PP can be anterior, non-anterior, or
complete (completely covering the internal os). The type
of PP was determined by the most recent transvaginal
ultrasound before delivery.
Elective Caesarean section was scheduled between 37
and 38 weeks of gestation by an obstetrician, who would
arrange for femoral sheath placement by notifying a
dedicated radiographer. A 5-Fr sheath (Lonyi Medicath,
Shenzhen, China) [Figure] was inserted into the right
common femoral artery before the elective Caesarean section in the radiology department. Techniques used to
insert the sheath were by palpation, under fluoroscopy, or
by ultrasonic guidance. Complications were categorised
into bleeding, infection, and thrombosis. Femoral sheath
placement was not performed when the delivery was
urgent or in an emergency setting when the attending
radiologist was otherwise occupied.
Figure. A 5-Fr femoral sheath set used in our institution.
Cases with major PP were divided into two groups,
namely those with femoral sheath placement and those
without. The primary outcome was the eventual need
for UAE. Technically successful UAE was defined
by successful embolisation of both uterine arteries.
Secondary outcomes included estimated intraoperative
blood loss; need for blood transfusion (units of packed
red cells); operation duration; additional procedures to
control bleeding, including compression sutures and
Bakri balloon insertion; and additional uterotonics
administered (medication other than the usual
prophylactic oxytocin/ergometrine), including rectal
misoprostol 800 to 1,000 mg, intramuscular carboprost
250 mcg, and infusion of concentrated oxytocin. PPH
was defined by blood loss > 1,000 mL and the cause was
categorised as active bleeding, concomitant placenta
accreta, or uterine atony.
Simple differences between the two groups were analysed
via Fisher’s exact and correlation test for categorical
and continuous variables, respectively. Continuous data
were expressed as median (interquartile range) and were
analysed with the Mann-Whitney U test. Multiple linear
regression was performed to investigate the effects of
femoral sheaths on estimated blood loss, need for blood
transfusion, operation duration, and use of uterotonics/additional procedures after adjusting for possible
confounders (i.e., age, gestation, parity, emergency
Caesarean section, and antepartum haemorrhage).
Poisson regression analysis was performed on units
of blood transfused, while multiple linear regression
analyses were performed to investigate the effects of
femoral sheath on estimated blood loss and operation
duration. Logistic regression analysis was performed
on additional use of uterotonics, additional procedures,
intensive care unit admissions, and hysterectomy.
Analyses were carried out using R version 3.6.3. A p
value < 0.05 was considered statistically significant.
RESULTS
One hundred and forty-five cases of major PP were
enrolled. All patients were ethnically Chinese. Seventy-one
(49%) were nulliparous. Seventy cases underwent
Caesarean section with femoral sheath placement and 75
cases underwent Caesarean section without. The patient
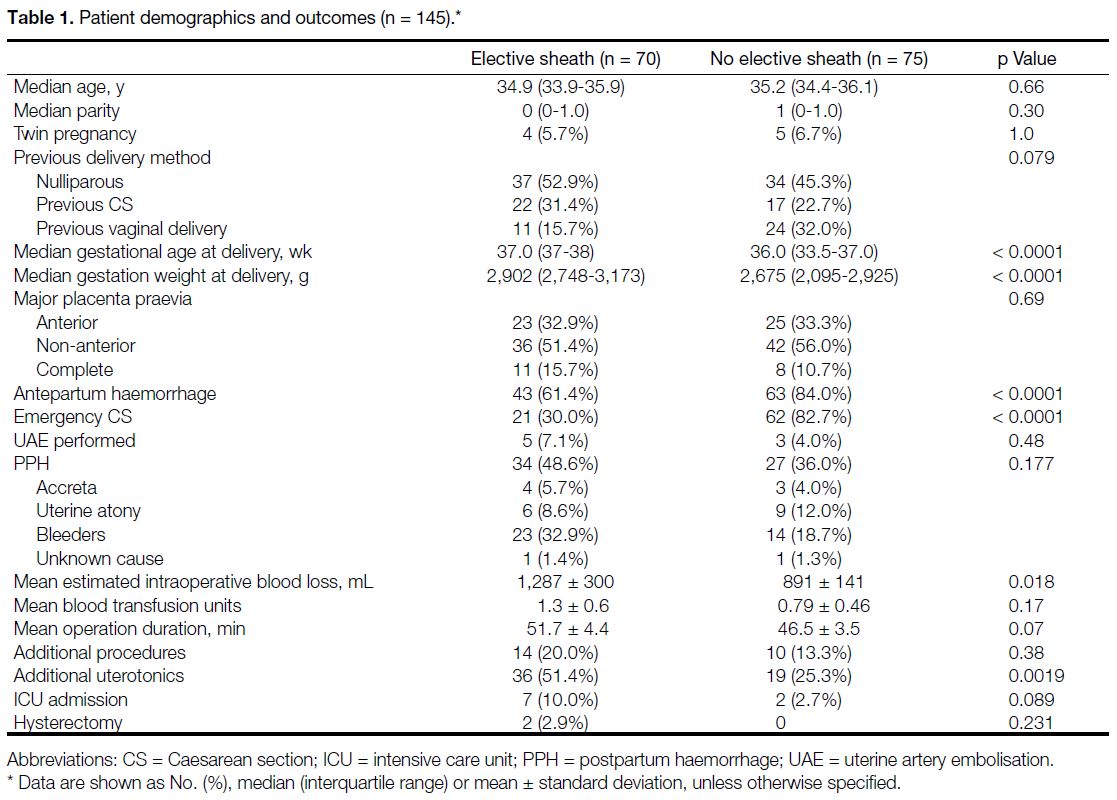
demographics and outcomes for the two groups are
summarised in Table 1. The demographic and obstetric
characteristics were similar in both groups, with the
exception of the median gestational age at delivery,
which was significantly lower in the cases not receiving
femoral sheaths (36 vs. 37.1 weeks; p < 0.0001). The
frequency of antepartum haemorrhage (84% vs. 61.4%)
and need for emergency Caesarean section (82.7% vs.
30%) were higher in the group not receiving femoral
sheaths %; (both p < 0.0001).
Table 1. Patient demographics and outcomes (n = 145)
The eventual need for UAE was 4.0% for those not
receiving femoral sheaths; it was 7.1% for the cases with
femoral sheaths (p = 0.48). All UAEs were performed
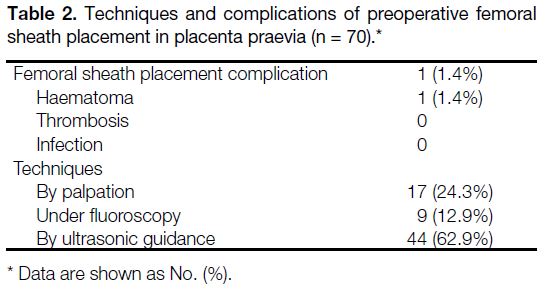
successfully in both groups. The majority (62.9%) of the
femoral sheaths were inserted by ultrasonic guidance
(Table 2). A single complication, a localised 6-cm
haematoma, occurred in one case.
Table 2. Techniques and complications of preoperative femoral sheath placement in placenta praevia (n = 70).
The overall incidence of PPH was 40.6%, mostly due
to bleeding from the placental bed. The mean estimated
intraoperative blood loss appears significantly greater
in the cases receiving sheaths electively than in those
undergoing emergent UAE (1,287 mL vs. 891 mL;
p = 0.018) [Table 1]. However, the mean operation
duration, blood transfusion rate, and use of additional
procedures were comparable in both groups after
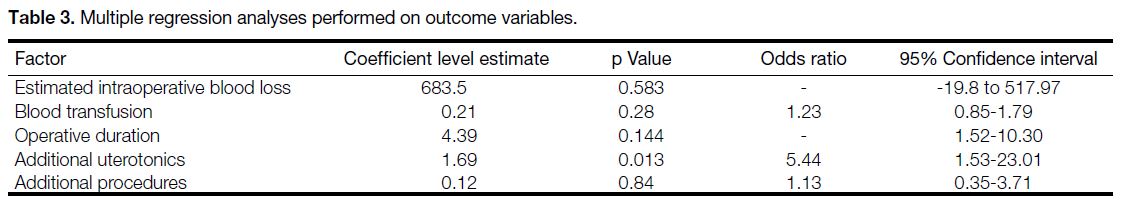
adjusting for confounders (Table 3). Logistic regression
analysis shows that the odds ratio for receiving additional
uterotonics was higher in those receiving elective femoral
sheaths (5.44, 95% confidence interval = 1.53-23.01;
p = 0.013).
Table 3. Multiple regression analyses performed on outcome variables.
DISCUSSION
The current definition of PP is limited to placentas that cover the internal os.[10] Nonetheless, minor (grade I and
II) and major (grade III and IV) PP are still in use to
date.[10] The prevalence of PP in this study was 13.1 per
1,000 deliveries, higher than the rate of 5.2 per 1,000
pregnancies previously reported in 2013.[1] This can be
contributed by raised awareness and screening of PP
increasingly becoming a part of standard obstetric care.
Iyasu et al[11] found that Asian women are twice more likely to develop PP compared to other ethnicities, hinting a
genetic predisposition. All patients in this study are of
Chinese ethnicity, which may have also contributed to
the higher prevalence.
Unlike invasive coronary angiography in interventional
cardiology,[12] to the best of our knowledge, femoral
sheath placement in PP has not been previously studied.
Femoral access can be technically difficult when
circulation is compromised. Also, there is considerable
variation in the anatomy of the femoral artery,[13] and
its pulse may be nonpalpable in pregnant women with
physiological oedema. Therefore, it was postulated that
elective femoral arterial access prior to the procedure
could facilitate UAE and reduce vascular complications
when UAE is eventually needed. In this study, most
of the femoral sheaths were inserted under ultrasonic
guidance. Ultrasonic guidance is the preferred method
by radiologists, with a success rate of 98.5% and reduced
number of re-attempts.[14] Fluoroscopy, although safe, is
the least preferred method because of concerns with
radiation.[15]
The majority of the femoral sheaths were not used and
were removed 24 hours postoperatively. Haematoma
formation occurred in one case (1.4%) with preoperative
femoral sheath insertion. Significant local haematoma
can occur in 2% to 3% of the femoral sheath procedures,
but these figures were derived from non-obstetric
studies.[13] [14] Thrombosis, potentiated by the inherent
thrombogenic effect of pregnancy, was not observed in
this study.
Other studies have shown that increased birth weight
and greater gestational age were associated with more
bleeding in major PP.[16] [17] The cases receiving the sheath
electively delivered at a greater gestational age, which
was associated with more blood loss. Increased blood
loss should not be attributed to the femoral sheath alone,
as shown by multivariate analysis, which found that the
femoral sheath is not associated with poorer outcome.
The need for additional uterotonics was found in the
cases receiving the sheath electively, however.
A large proportion of emergency Caesarean sections
were performed without elective femoral sheath
placement, because transport to the radiology department
can be time-consuming and the radiologist may not
be available. When UAE was needed in this group of
women, the femoral access was uncomplicated, further
arguing against the need for routine placement.
Limitations
Potential limitations of this study are due to its
retrospective nature. Intraoperative blood loss was
estimated since calibrated drapes and weighing of gauzes
were not introduced yet at the time of this study. Long-term
complications such as femoral artery aneurysm or
arteriovenous fistula were not documented. In addition,
explicit criteria were not applied when deciding which
patients should receive a femoral sheath prior to delivery.
This study also did not examine the role of femoral sheath
in the placenta accreta spectrum, a rarer but significant
cause of intractable intraoperative blood loss.
CONCLUSION
This 10-year retrospective analysis, focusing on the
use of elective femoral sheath placement in cases of
PP undergoing Caesarean section, did not confirm its
theoretical advantage of facilitating subsequent UAE
due to low usage. Furthermore, it may expose patients
to unnecessary risks and discomfort. Future research
should prioritise investigating the prophylactic use of
femoral sheath in cases where UAE is more likely to be
employed, such as placenta accreta spectrum.
REFERENCES
1. Cresswell JA, Ronsmans C, Calvert C, Filippi V. Prevalence of placenta praevia by world region: a systematic review and meta-analysis. Trop Med Int Health. 2013;18:712-24. Crossref
2. Royal College of Obstetricians and Gynaecologists. Blood Transfusions in Obstetrics. Green-top Guideline No. 47. London: RCOG; 2015.
3. Royal College of Obstetricians and Gynaecologists. Placenta Praevia and Placenta Accreta: Diagnosis and Management. Green-top Guideline No.27a. London: RCOG; 2018.
4. Vedantham S, Goodwin SC, McLucas B, Mohr G. Uterine artery embolization: an underused method of controlling pelvic hemorrhage. Am J Obstet Gynecol. 1997;176:938-48. Crossref
5. Mei J, Wang Y, Zou B, Hou Y, Ma T, Chen M, et al. Systematic
review of uterus-preserving treatment modalities for abnormally
invasive placenta. J Obstet Gynaecol. 2015;35:777-82. Crossref
6. Luo F, Xie L, Xie P, Liu S, Zhu Y. Intraoperative aortic balloon occlusion in patients with placenta previa and/or placenta accreta: a retrospective study. Taiwan J Obstet Gynaecol. 2017;56:147-52. Crossref
7. Yu SC, Cheng YK, Tse WT, Sahota DS, Chung MY, Wong SS, et al. Perioperative prophylactic internal iliac artery balloon occlusion in the prevention of postpartum hemorrhage in placenta previa: a randomized controlled trial. Am J Obstet Gynecol.
2020;223:117.e1-13. Crossref
8. Shevell T, Malone FD. Management of obstetric hemorrhage. Semin Perinatol. 2003;27:86-104. Crossref
9. National Center for Health Statistics, Centers for Disease Control
and Prevention. ICD-10-CM International Classification of
Diseases, Tenth Revision, Clinical Modification (ICD-10-CM).
Available from: https://www.cdc.gov/nchs/icd/icd-10-cm.htm. Accessed 21 Nov 2023.
10. Jauniaux E, Alfirevic Z, Bhide AG, Belfort MA, Burton GJ, Collins SL, et al. Placenta praevia and placenta accreta: diagnosis and management: green-top guideline No. 27a. BJOG.
2019;126:e1-48. Crossref
11. Iyasu S, Saftlas AK, Rowley DL, Koonin LM, Lawson HW, Atrash HK. The epidemiology of placenta previa in the United States, 1979 through 1987. Am J Obstet Gynaecol. 1993;168:1424-9. Crossref
12. Castle EV, Rathod KS, Guttmann OP, Jenkins AM, McCarthy CD,
Knight CJ, et al. Routine use of fluoroscopic guidance and up-front
femoral angiography results in reduced femoral complications
in patients undergoing coronary angiographic procedures: an
observational study using an interrupted time-series analysis. Heart
Vessels. 2019;34:419-26. Crossref
13. Abu-Fadel MS, Sparling JM, Zacharias SJ, Aston CE, Saucedo JF,
Schechter E, et al. Fluoroscopy vs. traditional guided femoral
arterial access and the use of closure devices: a randomized controlled trial. Catheter Cardiovasc Interv. 2009;74:533-9. Crossref
14. Kurisu K, Osanai T, Kazumata K, Nakayama N, Abumiya T, Shichinohe H, et al. Ultrasound-guided femoral artery access for minimally invasive neuro-intervention and risk factors for access site hematoma. Neurol Med Chir (Tokyo). 2016;56:745-52. Crossref
15. Stahl CM, Meisinger QC, Andre MP, Kinney TB, Newton IG. Radiation risk to the fluoroscopy operator and staff. AJR Am J Roentgenol. 2016;207:737-44. Crossref
16. Shinohara S, Okuda Y, Hirata S. Association between birth weight
and massive haemorrhage in pregnancy with a low-lying placenta:
a 9-year single-centre retrospective cohort study in Japan. J Obstet
Gynaecol. 2019;39:22-6. Crossref
17. Boyle RK, Waters BA, O’Rourke PK. Blood transfusion for caesarean delivery complicated by placenta praevia. Aust N Z J Obstet Gynaecol. 2009;49:627-30. Crossref