Radiological and Positron Emission Tomography–Computed Tomography Features of Xanthogranulomatous Mastitis: An Extremely Rare Malignancy Mimicker in the Male Breast
CASE REPORT
Hong Kong J Radiol 2023 Jun;26(2):e10-3 | Epub 8 May 2023
Radiological and Positron Emission Tomography–Computed Tomography Features of Xanthogranulomatous Mastitis: An
Extremely Rare Malignancy Mimicker in the Male Breast
T Wong1, S Yang2, WY Fung1, RLS Chan1, CM Chau1, AWT Yung1, JKF Ma1
1 Department of Radiology, Princess Margaret Hospital, Hong Kong SAR, China
2 Department of Radiology, Tuen Mun Hospital, Hong Kong SAR, China
Correspondence: Dr T Wong, Department of Radiology, Princess Margaret Hospital, Hong Kong SAR, China. Email: gloria_wong@live.com
Submitted: 21 Dec 2021; Accepted: 26 Jan 2022.
Contributors: All authors designed the study. TW, SY, WYF, RLSC and CMC acquired and analysed the data. TW and SY drafted the
manuscript. All authors critically revised the manuscript for important intellectual content. All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of Interest: All authors have disclosed no conflicts of interest.
Funding/Support: This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data Availability: All data generated or analysed during the present study are available from the corresponding author on reasonable request.
Ethics Approval: This study was approved by the Kowloon West Cluster Research Ethics Committee of Hospital Authority, Hong Kong (Ref No.: 152-12). The patient was treated in accordance with the tenets of the Declaration of Helsinki and provided written informed consent for the investigations and the publication of this case report.
CASE REPORT
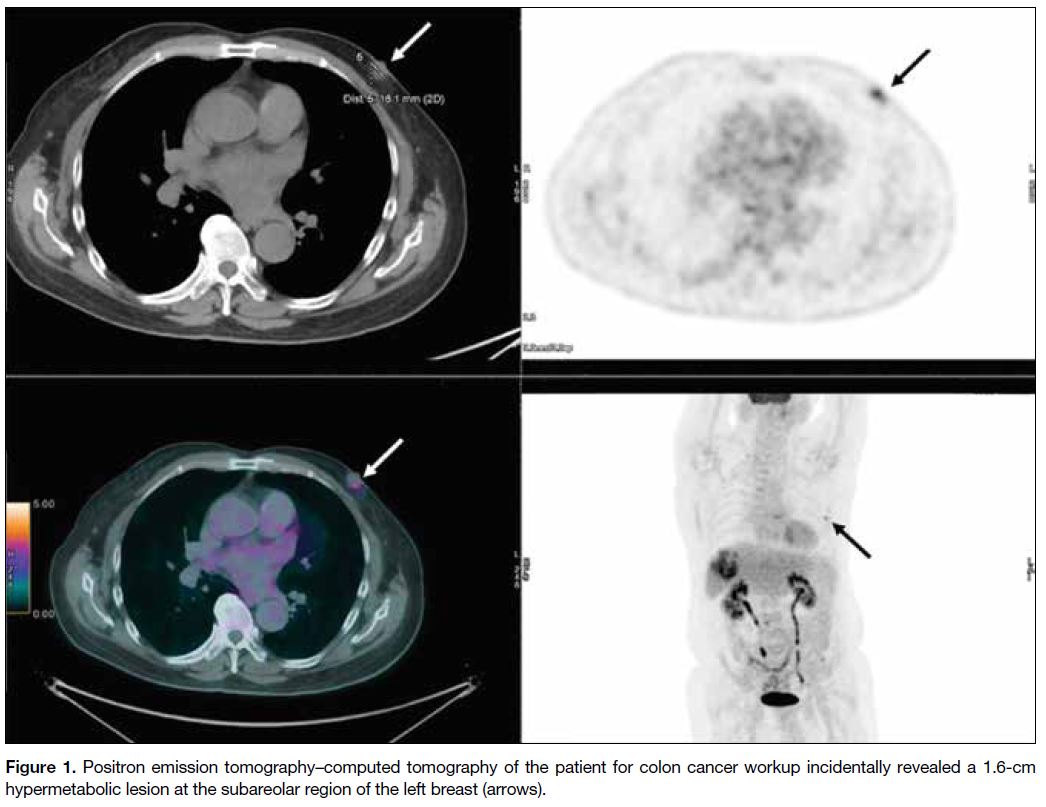
A 71-year-old male presented with an incidental finding
of a 1.6-cm hypermetabolic oval nodule in the subareolar
region of the left breast with maximum standardised
uptake value of 3.5 on positron emission tomography–computed tomography (PET-CT) [Figure 1]. He had
stage IV colon cancer with multiple liver metastases. No
abnormal lymph node was seen in the left axilla. Physical
examination revealed a 1.5-cm firm mobile mass at
the left breast subareolar region that was considered
clinically suspicious.
Figure 1. Positron emission tomography–computed tomography of the patient for colon cancer workup incidentally revealed a 1.6-cm
hypermetabolic lesion at the subareolar region of the left breast (arrows).
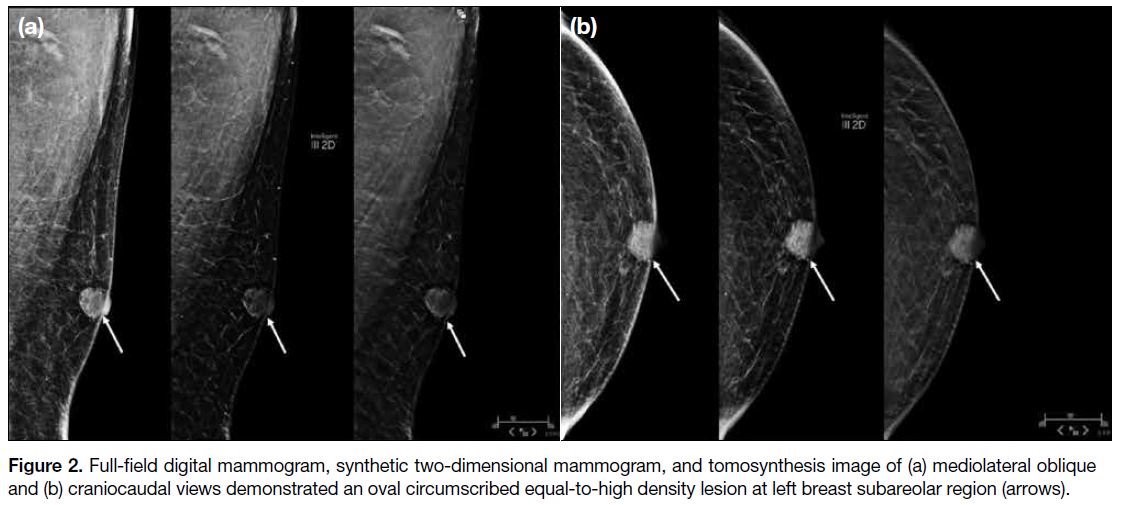
Mammography and tomosynthesis images revealed an
oval circumscribed lesion of equal-to-high density at the
subareolar region of the left breast with no nipple or skin
retraction (Figure 2). There was no associated suspicious
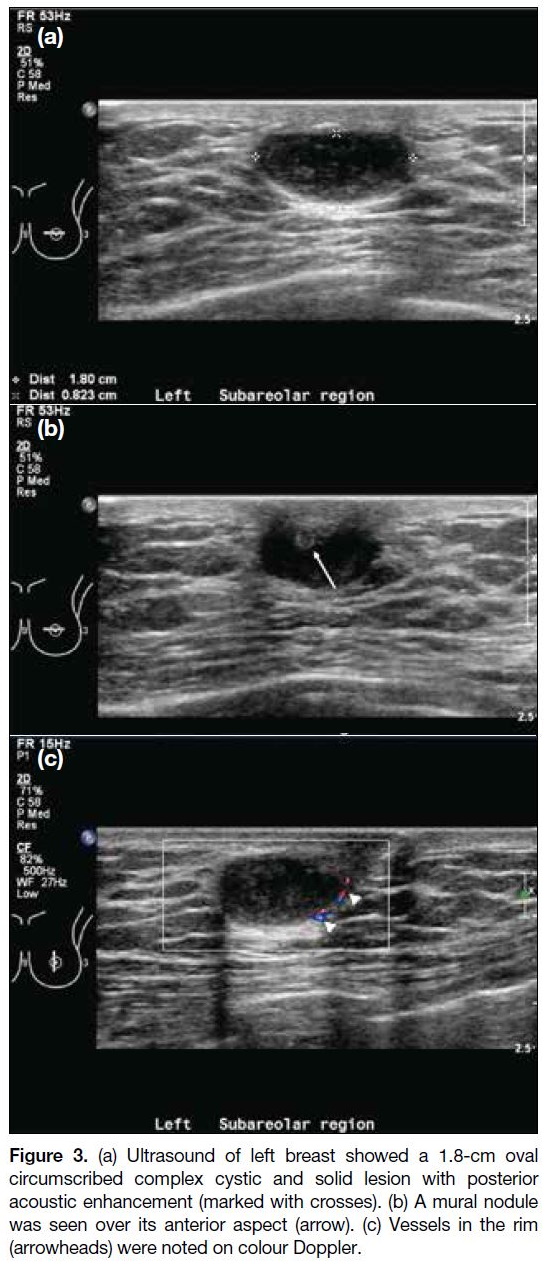
calcification or architectural distortion. On ultrasound,
a 1.8 cm × 0.8 cm × 1.6 cm oval circumscribed
complex cystic and solid lesion with posterior acoustic
enhancement was seen at the subareolar region of the left breast (Figure 3a). A 0.3-cm echogenic mural nodule
was seen at the anterior aspect of the lesion (Figure 3b).
Vessels in the rim were noted on colour Doppler (Figure 3c). No abnormal axillary lymphadenopathy was found.
The lesion was classified as BI-RADS (Breast Imaging
Reporting and Data System) category 4B.
Figure 2. Full-field digital mammogram, synthetic two-dimensional mammogram, and tomosynthesis image of (a) mediolateral oblique
and (b) craniocaudal views demonstrated an oval circumscribed equal-to-high density lesion at left breast subareolar region (arrows).
Figure 3. (a) Ultrasound of left breast showed a 1.8-cm oval
circumscribed complex cystic and solid lesion with posterior
acoustic enhancement (marked with crosses). (b) A mural nodule
was seen over its anterior aspect (arrow). (c) Vessels in the rim
(arrowheads) were noted on colour Doppler.
Core biopsy revealed xanthogranulomatous mastitis
(XGM) without malignancy. The patient opted for
conservative management. He remained asymptomatic
for the breast lesion upon follow-up 6 months later, with
only a vague lump in the subareolar region of the left
breast palpable during physical examination. Ultrasound
revealed interval shrinkage of the lesion to 1.3 cm ×
0.7 cm × 1.1 cm. It remained oval and circumscribed,
with mixed cystic and solid components (Figure 4).
Figure 4. Follow-up ultrasound of left breast 6 months later showed
interval shrinkage of the lesion to 1.3 cm in size. (a) It remained oval
and circumscribed with cystic and solid components (marked with
crosses). (b) The echogenic mural nodule (arrow) was seen.
DISCUSSION
XGM is a rare chronic benign inflammatory condition
of the breast, with fewer than 30 cases reported and none in men since it was first described in 2005.[1] [2] To
the best of our knowledge, this is the first reported case
in a male XGM patient with PET-CT and digital breast
tomosynthesis performed.
The aetiology of XGM remains debatable. Koo and Jung[3]
postulated it to be a result of obstruction and rupture of
dilated ducts with foamy histiocyte aggregates. XGM
has been reported in patients with concurrent breast
cancer,[3] fat necrosis,[3] lactational changes,[3] and implant
rupture,[4] [5] [6] suggesting that prior insult, hypersecretory
status or implant leak might be triggering factors.[3] [5] It has
also been reported in breast cancer regression following
neoadjuvant chemotherapy and in Erdheim–Chester disease with breast involvement.[7] [8]
XGM is commonly identified as a BI-RADS category
4 or 5 lesion on breast imaging, as noted in the present
case.[1] [3] [9] [10] Nonetheless the common imaging features
of XGM have not been well reported[10] and were only
described in a few cases. XGM lesions have been
depicted as solid hypoechoic lesions on ultrasound,[1] [4] [9] [10] with most described as irregular.[1] [9] [10] On mammography,
XGM has been revealed as a poorly defined dense area[9]
or as a spiculated mass with increasing number and size
of the associated clustered calcifications.[10] Previous
reports of magnetic resonance imaging described a
patient with a poorly defined heterogeneous area in the
breast that showed early and heterogeneous enhancement
with upward curve,[9] and another patient with prior
breast reconstruction presenting with areas of contrast
enhancement in the breast reconstruction and latissimus
dorsi scar, mimicking breast cancer recurrence.[5]
In our patient, XGM presented initially as a
hypermetabolic lesion on PET-CT. It was an oval
circumscribed lesion of equal-to-high density on
full-field digital mammography and digital breast
tomosynthesis and was complex mixed cystic and solid
with an echogenic mural nodule and vessels in the rim
on ultrasound. Such radiological features have not been
reported before. Nonetheless XGM has previously been
reported to have a cystic precursor stage, presumed to
represent the markedly dilated duct preceding its rupture.[1]
It is evident that XGM can have a variable radiological
presentation.
A complex cystic breast lesion can have a wide range
of differential diagnoses, but there is a substantial risk
that it is a malignant lesion, such as ductal carcinoma
in situ or invasive ductal carcinoma and invasive
lobular carcinoma.[11] Other common diagnoses include
fibrocystic changes, fibroadenoma, intraductal or
intracystic papilloma with or without atypia, atypical
ductal hyperplasia, and lobular neoplasia.[11] It is therefore
radiologically difficult to differentiate this benign entity
from a malignant condition. It has been suggested that
the mass-forming nature of XGM with the presence of
inflammation accounts for its suspicious appearance,[9]
therefore biopsy is often required to confirm the
diagnosis.[1] [10] [11]
XGM is often asymptomatic with a self-limiting course.[1]
It was an incidental finding in our case, with subsequent shrinkage. Nonetheless there is insufficient evidence to
guide optimum management and radiological follow-up.[1] Surgical excision is not common practice but may
be required for large or infiltrative lesions since drainage,
steroids, and antibiotics are unhelpful.[1]
In conclusion, XGM is exceedingly rare, and our patient
is the first reported case in a male. Its radiological
appearance can mimic malignancy and it may
demonstrate hypermetabolism on PET-CT. Histological
evaluation is essential to confirm the diagnosis of this
benign entity.
REFERENCES
1. Kapoor H, Zhang Y, Qasem SA, Owen W, Szabunio MM. Xanthogranulomatous
mastitis preceded by cysts on ultrasound: two cases
with review of literature. Clin Imaging. 2021;78:64-8. Crossref
2. Shin SJ, Scamman W, Gopalan A, Rosen PP. Mammary presentation of adult-type “juvenile” xanthogranuloma. Am J Surg
Pathol. 2005;29:827-31. Crossref
3. Koo JS, Jung W. Xanthogranulomatous mastitis: clinicopathology and pathological implications. Pathol Int. 2009;59:234-40. Crossref
4. Dinets A, Unukovych D, Khrapach V, Zakhartseva O, Sulik V, Kaminskyi E, et al. An unusual case of a ruptured Poly Implant Prothèse breast implant associated with xanthoma. Case Reports Plast Surg Hand Surg. 2016;3:11-5. Crossref
5. Hussain T, Elahi B, Long E, Mahapatra T, McManus PL, Kneeshaw PJ. Xanthogranulomatous inflammation involving
latissimus dorsi donor site and implant breast reconstruction: case
report and literature review. World J Surg Oncol. 2012;10:166. Crossref
6. Hernanz F, Baeza S, Serna E, Gómez-Fleitas M. Xanthogranulomatous capsulitis mimicking a polypoid neoplasm
disease: an unusual presentation of ruptured Poly Implant Prothèse
(PIP) breast implant. Eur J Plas Surg. 2013;36:797-800. Crossref
7. Aktepe F, Kapucuoğlu N, Pak I. The effects of chemotherapy on breast cancer tissue in locally advanced breast cancer. Histopathology. 1996;29:63-7. Crossref
8. Barnes PJ, Foyle A, Haché KA, Langley RG, Burrell S, Juskevicius R. Erdheim–Chester disease of the breast: a case report and review of the literature. Breast J. 2005;11:462-7. Crossref
9. de Oliveira I Junior, Viana CR, Sabino SM, Kerr LM, Vieira RA. Xanthogranulomatous mastitis mimicking locally advanced breast cancer. Breast J. 2017;23:227-9. Crossref
10. Hwang SH, Son EJ, Oh KK, Kim EK, Jung J, Jung WH. Bilateral xanthogranuloma of the breast: radiologic findings and pathologic correlation. J Ultrasound Med. 2007;26:535-7. Crossref
11. Doshi DJ, March DE, Crisi GM, Coughlin BF. Complex cystic breast masses: diagnostic approach and imaging-pathologic correlation. Radiographics. 2007;27 Suppl 1:S53-64. Crossref