Computed Tomography and Magnetic Resonance Imaging Features of Pedal Ectrodactyly with Lateral Hindfoot Syndrome: A Case Report
CASE REPORT
Hong Kong J Radiol 2024 Sep;27(3):e176-82 | Epub 2 September 2024
Computed Tomography and Magnetic Resonance Imaging
Features of Pedal Ectrodactyly with Lateral Hindfoot Syndrome: A Case Report
JK Fung1, JHM Cheng1, JKC Chan2, BWT Cheng1, CY Chu1, KH Chin1
1 Department of Radiology, Pamela Youde Nethersole Eastern Hospital, Hong Kong SAR, China
2 Department of Orthopaedics and Traumatology, Pamela Youde Nethersole Eastern Hospital, Hong Kong SAR, China
Correspondence: Dr JK Fung, Department of Radiology, Pamela Youde Nethersole Eastern Hospital, Hong Kong SAR, China. Email: jamesfung@gmail.com
Submitted: 11 June 2023; Accepted: 5 October 2023.
Contributors: JKF and JHMC designed the study. JKF, JHMC, JKCC, BWTC and CYC acquired and analysed the data. JKF, JHMC, JKCC
and BWTC drafted the manuscript. JKF, JHMC, JKCC, CYC and KHC critically revised the manuscript for important intellectual content. All
authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and
integrity.
Conflicts of Interest: All authors have disclosed no conflicts of interest.
Funding/Support: This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data Availability: All data generated or analysed during the present study are available from the corresponding author on reasonable request.
Ethics Approval: This study was approved by the Hong Kong East Cluster Research Ethics Committee of Hospital Authority, Hong Kong (Ref No.:
CIRB-2023-069-1). Informed patient consent for the study and publication was obtained.
INTRODUCTION
Ectrodactyly, also known as split hand and foot
deformity, is a rare congenital skeletal deformity
characterised by deficiency or absence of the central
digital rays. The central cleft simulates the appearance of
a lobster claw.[1] It can present as an isolated deformity or
part of a syndrome—usually with autosomal dominance
inheritance—such as the ectrodactyly-ectodermal
dysplasia-clefting syndrome or limb-mammary
syndrome.[2] [3]
We present a case with non-syndromic pedal ectrodactyly.
The patient presented with chronic pain over the lateral
ankle. To the best of our knowledge, this is the first report
of imaging findings, highlighting consequent soft tissue
findings in an adult with split foot deformity.
CASE PRESENTATION
A 31-year-old female with known left foot deformity
since birth presented with a 2-year history of increasing pain over the lateral ankle. The pain was worse on
movement and weight-bearing. There was no preceding
injury. She was born full term by normal spontaneous
delivery. She enjoyed good past health and had no other
known congenital anomalies. Physical examination
revealed clefting deformity and abnormal configuration
of the left foot. The lateral ankle joint was tender with
mild local swelling.
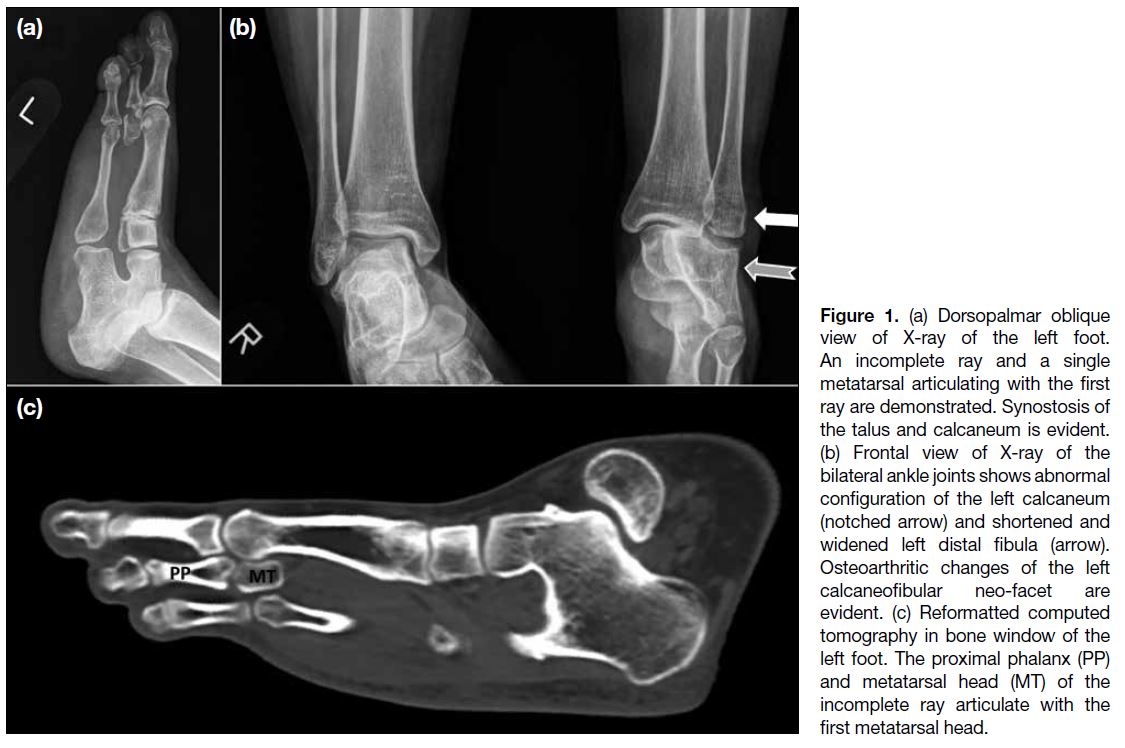
Radiographs and reconstructed three-dimensional
computed tomography of the left foot and ankle revealed
the presence of two complete rays and a singular tarsal
bone articulating with the first ray. An incomplete ray
was seen in between, comprised of two phalanges and a
metatarsal head. The base of the proximal phalanx and
the metatarsal head formed anomalous articulation with
the first metatarsal head (Figure 1).
Figure 1. (a) Dorsopalmar oblique
view of X-ray of the left foot.
An incomplete ray and a single
metatarsal articulating with the first
ray are demonstrated. Synostosis of
the talus and calcaneum is evident.
(b) Frontal view of X-ray of the
bilateral ankle joints shows abnormal
configuration of the left calcaneum
(notched arrow) and shortened and
widened left distal fibula (arrow).
Osteoarthritic changes of the left
calcaneofibular neo-facet are
evident. (c) Reformatted computed
tomography in bone window of the
left foot. The proximal phalanx (PP)
and metatarsal head (MT) of the
incomplete ray articulate with the
first metatarsal head.
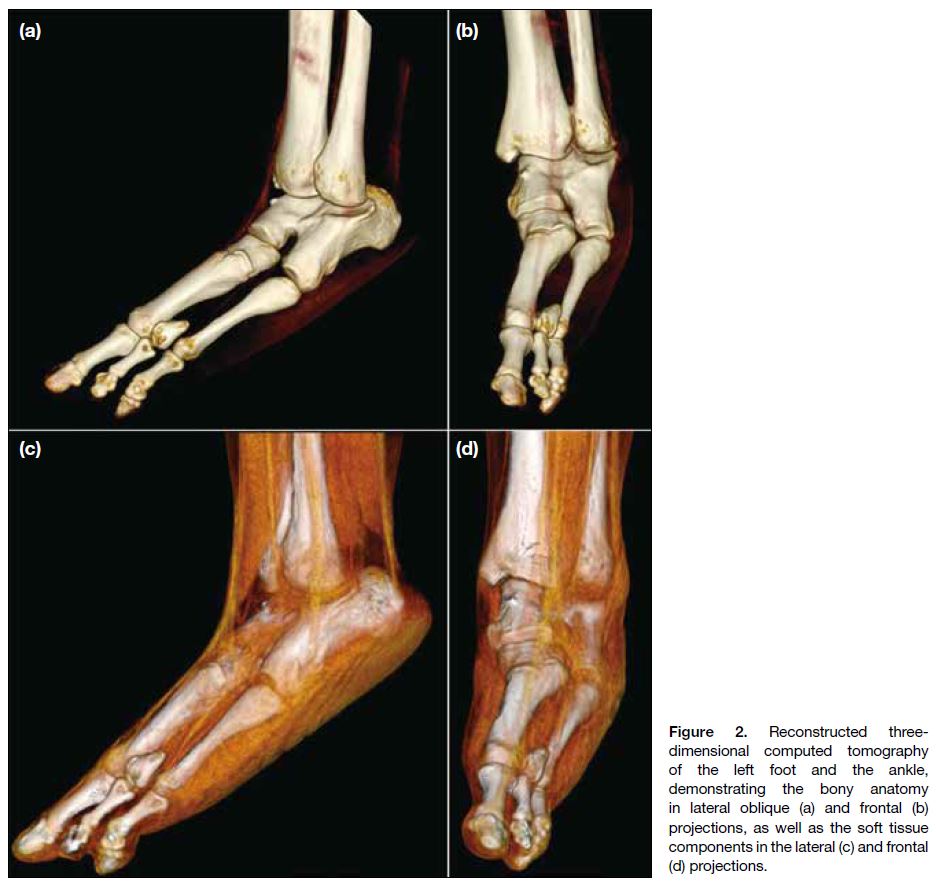
The left hindfoot was formed by a single bony
structure with anterior bifid appearance, simulating non-segmentation of the talus and calcaneus (hereby
termed the talocalcaneal complex) [Figures 1 and 2]. A
calcaneofibular neo-facet was demonstrated. The distal
fibula was shortened while the lateral malleolus appeared
widened (Figures 1 and 2).
Figure 2. Reconstructed three-dimensional
computed tomography
of the left foot and the ankle,
demonstrating the bony anatomy
in lateral oblique (a) and frontal (b)
projections, as well as the soft tissue
components in the lateral (c) and frontal
(d) projections.
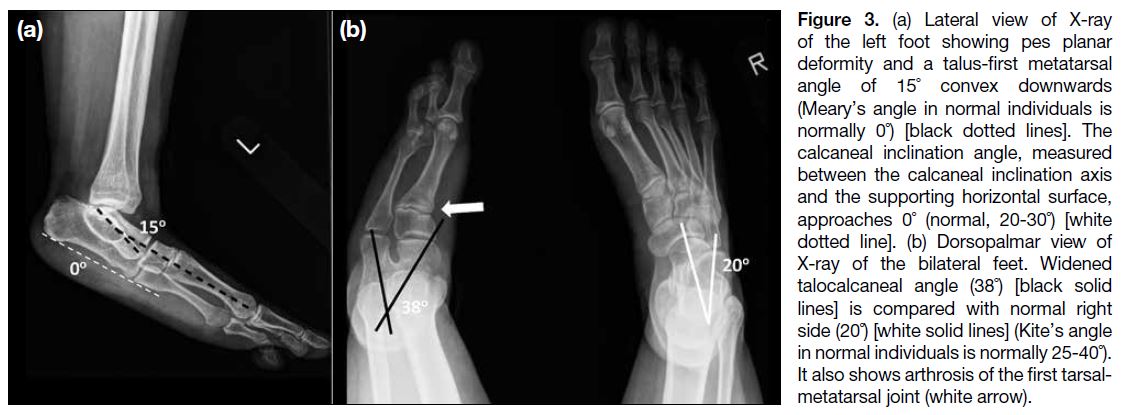
Pes planar deformity was evident with loss of both medial
and lateral longitudinal arches. The talus-first metatarsal
angle (Meary’s angle) measured 15° while the calcaneal
inclination angle approached 0°, signifying loss of the
medial and lateral arches, respectively (Figure 3a). There
was widening of the talocalcaneal angle, suggestive of
hindfoot valgus deformity (Figure 3b). Osteophytes and
subchondral sclerosis were seen around the first tarsalmetatarsal
joint, suggestive of midfoot arthrosis (Figure 3b).
Figure 3. (a) Lateral view of X-ray
of the left foot showing pes planar
deformity and a talus-first metatarsal
angle of 15˚ convex downwards
(Meary’s angle in normal individuals is
normally 0˚) [black dotted lines]. The
calcaneal inclination angle, measured
between the calcaneal inclination axis
and the supporting horizontal surface,
approaches 0˚ (normal, 20-30˚) [white
dotted line]. (b) Dorsopalmar view of
X-ray of the bilateral feet. Widened
talocalcaneal angle (38˚) [black solid
lines] is compared with normal right
side (20˚) [white solid lines] (Kite’s angle
in normal individuals is normally 25-40˚).
It also shows arthrosis of the first tarsal-metatarsal
joint (white arrow).
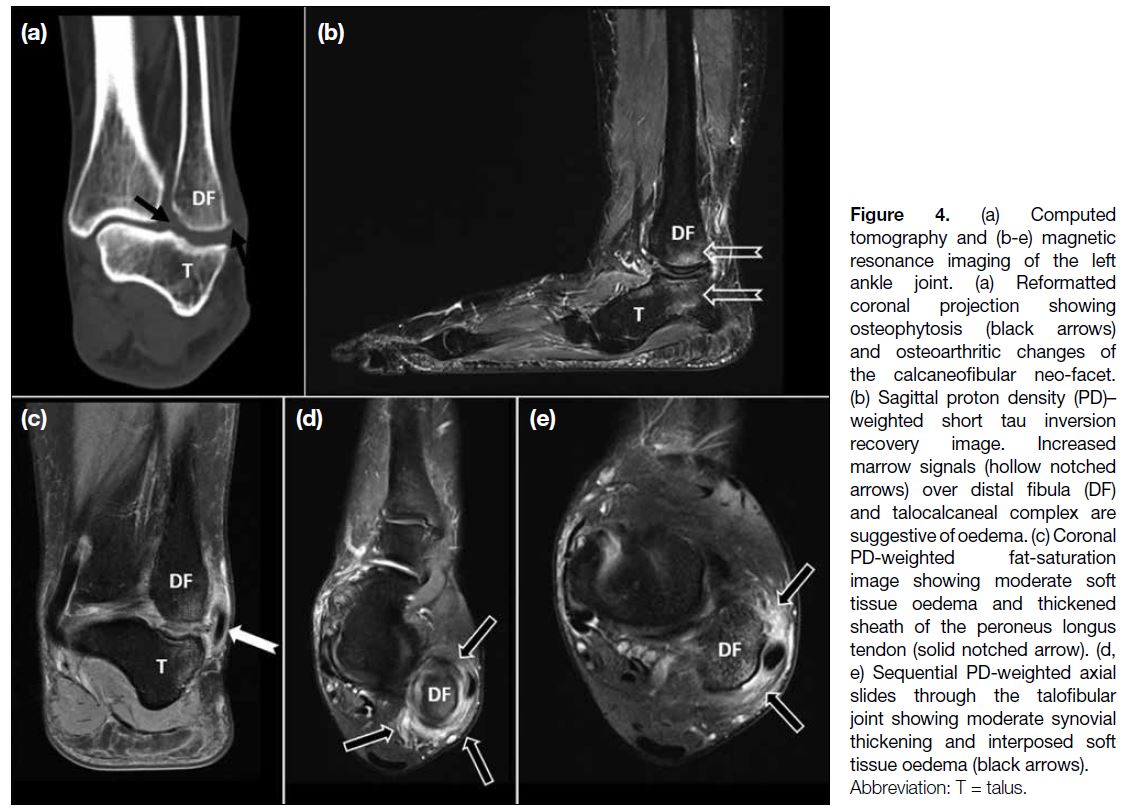
Computed tomography of the left ankle joint
revealed bony remodelling with flat neo-facets at the
calcaneofibular articulation. Secondary osteoarthritic
changes and osteophytes were observed (Figure 4a).
Magnetic resonance imaging showed associated marrow
oedema, moderate synovial thickening, and interposed
soft tissue oedema. Mild thickening of the adjacent peroneus brevis and longus tendon sheaths was observed
(Figures 4b to 4e). Overall features were suggestive of
lateral hindfoot impingement syndrome.
Figure 4. (a) Computed
tomography and (b-e) magnetic
resonance imaging of the left
ankle joint. (a) Reformatted
coronal projection showing
osteophytosis (black arrows)
and osteoarthritic changes of
the calcaneofibular neo-facet.
(b) Sagittal proton density (PD)–weighted short tau inversion
recovery image. Increased
marrow signals (hollow notched
arrows) over distal fibula (DF)
and talocalcaneal complex are
suggestive of oedema. (c) Coronal
PD-weighted fat-saturation
image showing moderate soft
tissue oedema and thickened
sheath of the peroneus longus
tendon (solid notched arrow). (d,
e) Sequential PD-weighted axial
slides through the talofibular
joint showing moderate synovial
thickening and interposed soft
tissue oedema (black arrows).
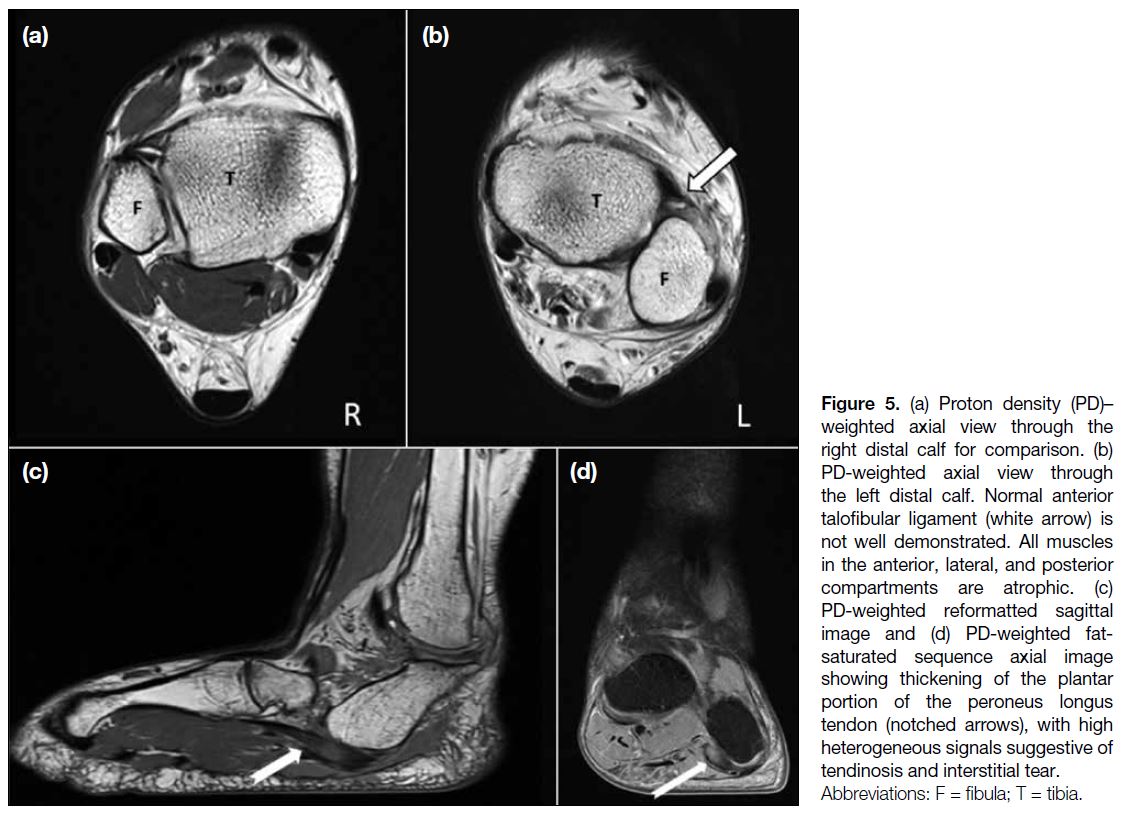
Normal anterior talofibular ligament and calcaneofibular
ligament were not well delineated, possibly due to
either congenital absence or secondary to chronic
impingement-related tearing (Figure 5a and 5b). The
posterior talofibular ligament and anterior inferior
tibiofibular ligament were small in calibre. Moderate
thickening and high heterogeneous short tau inversion
recovery signals of the peroneus longus tendon was seen,
suggestive of tendinosis and interstitial tear (Figure 5c and 5d). It was possibly a sequala of the altered hindfoot
biomechanics.
Figure 5. (a) Proton density (PD)–weighted axial view through the
right distal calf for comparison. (b)
PD-weighted axial view through
the left distal calf. Normal anterior
talofibular ligament (white arrow) is
not well demonstrated. All muscles
in the anterior, lateral, and posterior
compartments are atrophic. (c)
PD-weighted reformatted sagittal
image and (d) PD-weighted fat-saturated
sequence axial image
showing thickening of the plantar
portion of the peroneus longus
tendon (notched arrows), with high
heterogeneous signals suggestive of
tendinosis and interstitial tear.
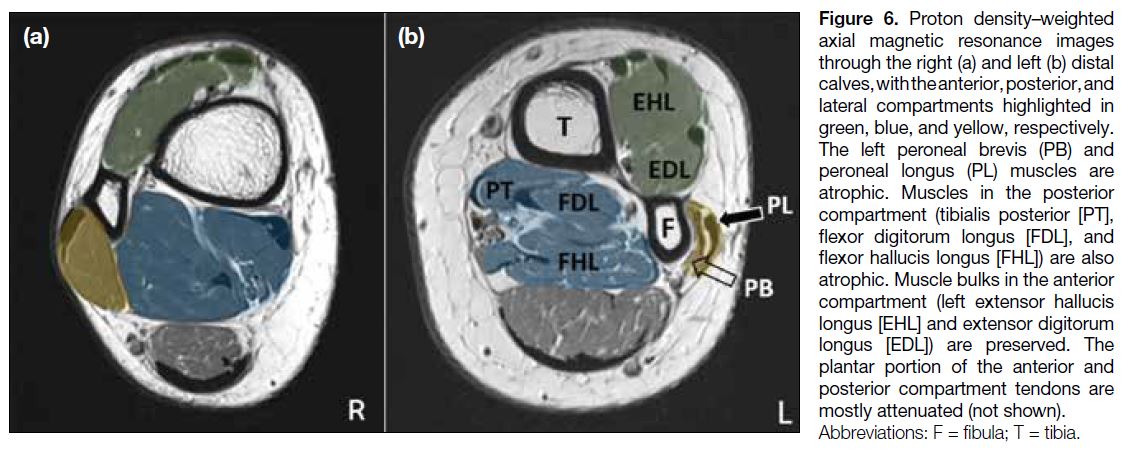
The left peroneus longus and brevis muscles were
atrophic compared with the right side. Normal infra-malleolar
portion of the peroneus brevis tendon was not
demonstrated (Figure 6). Other calf muscles had smaller
bulk than the right side, most evident at the lateral and
posterior compartments (Figure 5b). The plantar portions
of the tendons in the anterior and posterior compartment
were attenuated.
Figure 6. Proton density–weighted
axial magnetic resonance images
through the right (a) and left (b) distal
calves, with the anterior, posterior, and
lateral compartments highlighted in
green, blue, and yellow, respectively.
The left peroneal brevis (PB) and
peroneal longus (PL) muscles are
atrophic. Muscles in the posterior
compartment (tibialis posterior [PT],
flexor digitorum longus [FDL], and
flexor hallucis longus [FHL]) are also
atrophic. Muscle bulks in the anterior
compartment (left extensor hallucis
longus [EHL] and extensor digitorum
longus [EDL]) are preserved. The
plantar portion of the anterior and
posterior compartment tendons are
mostly attenuated (not shown).
DISCUSSION
Ectrodactyly derives from the Greek words ‘ektromo’ and
‘daktylos’, meaning abortion and fingers, respectively. It
is nonetheless not limited to the digits or upper limbs.
Reportedly it represents a spectrum of limbic deformity,
from aphalangia, adactylia and acheiria, to hemimelia
or amelia. Most cases of sporadic ectrodactyly are
unilateral.[4] The pathogenesis involves failure of initiation
of apical ectodermal ridge, or subsequent signalling
pathways, that contributes to truncation of all skeletal
elements over the distal developing limb bud.[3]
Although ectrodactyly commonly presents as an isolated
finding, it may form part of a syndrome. Ectrodactyly-ectodermal
dysplasia-clefting syndrome is the most
reported. It is an autosomal dominant condition,
affecting structures derived from the ectoderm such
as hair, skin, nails, and teeth, with such presentations
as skin hypopigmentation, sparse hair, and dental
defects. Genitourinary and lacrimal duct anomalies are also common. Limb-mammary syndrome is also well
studied. It is characterised by mammary gland and nipple
hypoplasia.[5] Other less common syndromes associated
with ectrodactyly include Karsch–Neugebauer-syndrome (congenital nystagmus), Patterson-Stevenson-
Fontaine syndrome (mandibulofacial dysostosis), and
Adams-Oliver syndrome (scalp defect).[5] [6] Despite the
characteristic features, marked phenotypic variability
is reported, possibly related to variable expression and
incomplete penetrance.
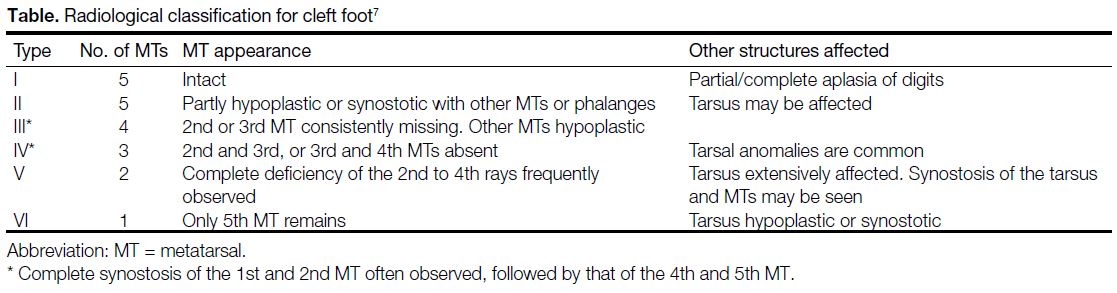
Blauth and Borisch[7] proposed a radiological classification
for cleft foot that describes a spectrum of metatarsal
defects ranging from types I to VI. The characteristics and
possible associated features are shown in the Table.[7] With
an incomplete metatarsus and two absent rays, our patient
fell between type IV and V. In line with the findings, our
patient demonstrates possible synostosis of the talus and
calcaneum. From the case series, the authors suggested
that cleft formation begins at the second or third ray, then proceeds in a distal to proximal fashion.[7] The fifth ray is
usually the last affected (Table). Synostosis is commonly
seen at the margin of the cleft. Associated features such
as syndactyly, polydactyly and cross-bone deformities
may be observed, yet appear widely variable.
Table. Radiological classification for cleft foot[7]
The presence of an incomplete ray caught our attention.
According to the known pattern of deformation, the
distal portion of the ray should be first affected. For
the incomplete ray, provided the absence of a proximal
metatarsal, the development of the distal metatarsal and phalanges are not to be expected. In split-hand
deformities, syndactyly of the remaining digits is
reportedly common. There are also rare cases of
triphalangeal thumbs.[5] In the case series by Blauth and
Borisch,[7] a few cases displaying central polydactylous
element were also reported. Two of the cases showed
duplicated phalanges of the second digit.[7] We remain
open to the possibility that the incomplete metatarsal
head in our patient might arise from the first ray as a
polydactylous deformity.
The Bluman-Myerson classification stages adult acquired
flatfoot deformity (AAFD) based on severity and rigidity
of the flatfoot deformity.[8] The bony deformities in our
patient caused severe and irreversible hindfoot valgus
and rigid flatfoot deformity, classified as stage III AAFD.
The altered bony configuration leads to lateral hindfoot
(or subfibular) impingement with associated soft tissue
fibrosis, midfoot arthrosis, peroneal tendinopathy, and
calcaneofibular ligament entrapment.[9] Stage III AAFD is
also not uncommonly present in patients with congenital
tarsal coalition due to arch flattening and associated
rigid hindfoot valgus.[10] The principles of treating stage
III AAFD include correcting hindfoot valgus, realigning
the midfoot from abduction deformity, and relieving the
lateral compartment. In normal individuals, arthrodesis of
the talonavicular and subtalar joints is usually performed,
where most deformities are found. The calcaneocuboid
joint may also be fused, after balancing against the
risks of ankle valgus, failure of the deltoid ligament and
worsened foot rigidity.[11] In our case, the aim of surgical
treatment will be to relieve lateral compartment pressure
and the associated pain. A bony procedure is needed
as the primary pathology is bone anomaly. Treatment
options are limited by a deformed talocalcaneal complex,
the absence of few mid- and hind-foot bony structures
and hence such joints as the subtalar and calcaneocuboid joints. Medialising calcaneal (talocalcaneal complex, in
our case) osteotomy is the most feasible option. In view
of the osteoarthritis of the calcaneofibular neo-facet, this
procedure may not completely relieve the pain. Ankle
fusion would be the last resort to treat the arthritic pain
since severe functional disability would result.
CONCLUSION
Common features of ectrodactyly, including absent
metatarsals and tarsal synostosis, are present in this case.
The presence of an incomplete distal ray around the
cleft is nonetheless discordant with current knowledge;
we propose that it may arise from the first ray as a
polydactylous deformity. Pes planus deformity and
associated lateral hindfoot impingement syndrome were
well demonstrated across different imaging modalities
and consistent with the clinical presentation. Future
case series directed at associated soft tissue injuries may
be helpful in planning rehabilitation programmes and
surgical interventions.
REFERENCES
1. Jindal G, Parmar VR, Gupta VK. Ectrodactyly/split hand feet malformation. Indian J Hum Genet. 2009;15:140-2. Crossref
2. Pinette M, Garcia L, Wax JR, Cartin A, Blackstone J. Familial ectrodactyly. J Ultrasound Med. 2006;25:1465-7. Crossref
3. Duijf PH, van Bokhoven H, Brunner HG. Pathogenesis of split-hand/split-foot malformation. Hum Mol Genet. 2003;12 Spec No 1: R51-60. Crossref
4. Krakow D. The dysostoses. In: Rimoin D, Pyeritz R, Korf B, editors. Emery and Rimoin’s Principles and Practice of Medical Genetics. 6th ed. Amsterdam: Elsevier; 2013. p 1-22. Crossref
5. van Bokhoven H, Hamel BC, Bamshad M, Sangiorgi E, Gurrieri F, Duijf PH, et al. p63 gene mutations in EEC syndrome,
limb-mammary syndrome, and isolated split hand-split foot
malformation suggest a genotype-phenotype correlation. Am J
Med Genet. 2001;69:481-92 Crossref
6. Hernandez-Andrade E, Yeo L, Goncaives LF, Luewan S, Garcia M,
Romero R. Fetal musculoskeletal system. In: Norton ME, Scoutt
LM, Feldstein VA, editors. Callen’s Ultrasonography in Obstetrics and Gynaecology, 6th ed. Amsterdam: Elsevier; 2017. p 272-345.
7. Blauth W, Borisch NC. Cleft feet. Proposals for a new classification
based on roentgenographic morphology. Clin Orthop Relat Res.
1990;(258):41-8. Crossref
8. Bluman EM, Title CI, Myerson MS. Posterior tibial tendon rupture:
a refined classification system. Foot Ankle Clin. 2007;12:233-49. Crossref
9. Donovan A, Rosenberg ZS. Extraarticular lateral hindfoot impingement with posterior tibial tendon tear: MRI correlation. AJR Am J Roentgenol. 2009;193:672-8. Crossref
10. Flores DV, Mejía Gómez C, Fernández Hernando M, Davis MA, Pathria MN. Adult acquired flatfoot deformity: anatomy,
biomechanics, staging, and imaging findings. Radiographics.
2019;39:1437-60. Crossref
11. Vulcano E, Deland JT, Ellis SJ. Approach and treatment of the adult acquired flatfoot deformity. Curr Rev Musculoskelet Med.
2013;6:294-303. Crossref