Stereotactic-Guided Magnetic Seed Localisation Versus Radioguided Occult Lesion Localisation: A Comparison of Total Resection Volumes
ORIGINAL ARTICLE
Hong Kong J Radiol 2024 Sep;27(3):e164-70 | Epub 10 September 2024
Stereotactic-Guided Magnetic Seed Localisation Versus Radioguided Occult Lesion Localisation: A Comparison of Total
Resection Volumes
RYS Mak1, AHC Wong1, CKM Mo1, KH Chin1, WWC Wong1, PL Chau2, YH Ling2, LWY Ma3, JSY Lee3, JYW Chan3, CY Choi3, AYT Lai1
1 Department of Radiology, Pamela Youde Nethersole Eastern Hospital, Hong Kong SAR, China
2 Department of Surgery, Ruttonjee Hospital, Hong Kong SAR, China
3 Department of Surgery, Pamela Youde Nethersole Eastern Hospital, Hong Kong SAR, China
Correspondence: Dr RYS Mak, Department of Radiology, Pamela Youde Nethersole Eastern Hospital, Hong Kong SAR, China. Email: mys877@ha.org.hk
Submitted: 4 April 2023; Accepted: 5 October 2023.
Contributors: RYSM and AYTL designed the study. RYSM, AHCW, CKMM, PLC, YHL, LWYM, JSYL, JYWC and AYTL acquired the data.
RYSM, KHC, WWCW, YHL, LWYM and AYTL analysed the data. RYSM, AHCW and PLC drafted the manuscript. CKMM, KHC, WWCW,
PLC, YHL, LWYM, JSYL, JYWC, CYC and AYTL critically revised the manuscript for important intellectual content. All authors had full
access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of Interest: All authors have disclosed no conflicts of interest.
Funding/Support: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data Availability: All data generated or analysed during the present study are available from the corresponding author on reasonable request.
Ethics Approval: This research was approved by the Hong Kong East Cluster Research Ethics Committee of Hospital Authority, Hong Kong (Ref No.: HKECREC-2022-059). The requirement for patient consent was waived by the Committee due to the retrospective nature of the research.
Declaration: This paper was presented orally in the 30th Annual Scientific Meeting of Hong Kong College of Radiologists (12-13 November 2022; virtual meeting).
Abstract
Introduction
Cosmetic outcome after breast conservation surgery has a major impact on patients’ quality of life.
Previous research demonstrated the use of non-radioactive magnetic markers (Magseed) to be safe and effective.
There have been few studies comparing magnetic seeds and radioguided occult lesion localisation (ROLL). This
study compares the total resection volume in lumpectomies of mammographically detected non-palpable lesions
using magnetic seeds with the volume resulting from ROLL guidance.
Methods
This was a retrospective cohort study comparing lumpectomy cases guided by one or the other technique.
Total resection volume was calculated based on pathology reports. Margin clearance and reoperation rates were
analysed.
Results
Each cohort included 11 patients with similar baseline characteristics and comparable histopathology from
the vacuum-assisted biopsy specimens. The technical success rates of magnetic seed deployment and ROLL injection
were both 100%. The total resection volume in the magnetic seed cohort was significantly lower than that in the
ROLL cohort. If the cases with involved or close margins were excluded from analysis of total resection volume, the
magnetic seeds group still achieved a significantly lower total resection volume. No significant difference was found
in the final histopathological diagnosis, margin clearance, or reoperation rates between the two groups.
Conclusion
Magnetic seed localisation is a safe and effective technique that can reduce total resection volume
compared with ROLL, without compromising margin clearance and reoperation rates.
Key Words: Breast; Carcinoma; Psychosocial functioning
中文摘要
立體定位磁粒子定位與無線電導引隱匿性病灶定位:總切除體積的比較
麥恩善、黃可澄、巫冠文、錢凱、黃慧中、周珮鈴、凌若熙、馬慧欣、李雪盈、陳盈穎、蔡自怡、黎爾德
引言
乳房保留手術後的美容效果對患者的生活品質有重大影響。先前的研究證明使用非放射性磁性標記(Magseed)是安全有效的。比較磁性粒子和無線電引導隱匿性病灶定位(ROLL)的研究很少。本研究比較了使用磁粒子對乳房X光檢查檢測到的不可觸及病變進行腫塊切除術的總切除體積與ROLL引導結果的體積。
方法
這是一項回顧性隊列研究,比較由這兩種技術指導的腫瘤切除術病例。我們根據病理報告計算總切除體積,並分析切緣清除率和再手術率。
結果
每個隊列包括11名具有相似基線特徵和真空輔助活檢標本組織病理學相似的患者。磁粒子部署和ROLL注射的技術成功率均為100%。磁粒子組的總切除體積顯著低於ROLL組。如果將涉及或接近切緣的病例排除在總切除體積分析之外,磁粒子組的總切除體積仍顯著較低。兩組之間的最終組織病理學診斷、切緣清除或再手術率沒有顯著差異。
結論
磁粒子定位是一種安全有效的技術,與ROLL相比,可以減少總切除體積,且不影響切緣清除率和再手術率。
INTRODUCTION
The use of non-radioactive magnetic seed markers
(Magseed; Endomagnetics, Cambridge, United
Kingdom) is a relatively new technique for localisation
of non-palpable breast lesions requiring surgical
resection, including early breast cancers and high-risk
lesions, which are being increasingly detected due to
advancements in breast imaging techniques and more
widespread breast cancer screening. Several studies
have already demonstrated magnetic seeds to be a safe,
effective method that is non-inferior to wire-guided
localisation.[1] [2] [3] A recent retrospective cohort study
showed that localisation with magnetic seeds resulted in
reduced resection volumes without an increased margin
positivity rate compared with wire-guided localisation.
Minimising resection volumes is important for optimal
cosmetic outcome.[4]
In contrast, there have been fewer studies comparing
magnetic seeds and radioguided occult lesion localisation
(ROLL). Initial experience in a regional hospital in Hong
Kong showed comparable operation times, surgical
specimen sizes, margin clearances and reoperation rates
compared with ROLL, with magnetic seeds having the
added advantage of being non-radioactive and allowing decoupling of radiological and surgical schedules.[5] Due
to similar experience, magnetic seed localisation has
become the preferred technique since its adoption in our
unit.
It is known that the cosmetic outcome after breast
conservation surgery (BCS) can affect the psychosocial
functioning of patients.[6] Women with pronounced breast
asymmetry are more likely to feel stigmatised, experience
depressive symptoms, and have a worse quality of life.[6]
The major determining factor for cosmetic outcome is
resection volume.[7] Ideally, the resection volume should
be as small as possible without jeopardising the margin
status. This is in turn related to surgical accuracy that relies
heavily on the localisation technique for non-palpable
breast lesions.[7] We aim to compare the total resection
volume along with other outcome measures, including
margin status and reoperation rate, in lumpectomies of
mammographically detected non-palpable lesions under
magnetic seed and ROLL guidance performed in two
regional hospitals in Hong Kong.
METHODS
This retrospective cohort study first identified all
lumpectomy cases aiming at vacuum-assisted biopsy (VAB) markers guided by stereotactic-guided magnetic
seed localisation. To control for the targeted amount of
tissue to be excised, only the lumpectomy cases aiming
at radiopaque VAB markers that were placed after VAB
were included. These were malignant or high-risk lesions
identified from the VAB specimens, which required
further surgical excision. These excisions were guided by
magnetic seed placement. The cases were then matched
with a control group of older consecutive lumpectomy
cases aiming at VAB markers stereotactically guided by
ROLL, beginning immediately before the adoption of
magnetic seeds for such cases, until the same number was
reached. Theoretically, as the lesions were non-palpable
and sonographically occult, and the VAB markers were
the common mammographically localised targets, the
expected total resection volume would be comparable
between the two cohorts. It was not feasible to draw both
cohorts from the same time period as ROLL was rarely
utilised after the introduction of magnetic seeds.
Electronic medical records were reviewed. Baseline
characteristics including age, laterality of lesion, initial
mammographic abnormality, pathology of the VAB
specimen, and the time interval between localisation
and operation were recorded. The preoperative
mammographically detected post-VAB residual lesion
sizes including the VAB marker (3 mm) were measured.
The total span of the preoperative mammographically
detected post-VAB residual lesion (with inclusion of
the VAB marker) and the localisation agent (magnetic
seed or iodinated contrast injected during ROLL) was
likewise measured.
Surgical specimen volume was calculated using the
ellipse volume formula Volume = 4/3 × π × A × B × C,
where A, B, and C are the lengths of all three semi-axes
as documented in the pathology reports. If additional
margins were excised intraoperatively, their volumes
were likewise calculated. In cases where intraoperative
additional margins measurements were not fully
documented, they were assumed to be of negligible
volume. Specimens of other breast lesions, contralateral
breast surgery, and sentinel lymph node biopsy were
considered irrelevant in the calculation of specimen
volume in this study. The total resection volume was
yielded by the sum of all relevant specimens.
The technical success rate of localisation for magnetic
seeds and ROLL were recorded. The technical success
of magnetic seed localisation was defined as deployment
of the seeds without significant migration (>1 cm), and subsequent excision of the seeds and the VAB marker.
In the ROLL cohort, additional iodinated contrast (0.1-0.25 mL) was injected at the original site of isotope
injection, followed by post-procedural mammographic
spot images and planar scintigraphy to ensure accurate
localisation and absence of ductograms. Technically
successful ROLL was defined as iodinated contrast
seen at the site of the VAB marker and its subsequent
complete excision of the VAB marker.
Other relevant outcome measures, including operation
duration, pathology of the lumpectomy specimen,
margin status, successful surgical removal of all VAB
markers and magnetic seeds, and reoperation within 6
months, were also analysed.
Statistical Analysis
Statistical analysis was performed using SPSS (Windows
version 28.0; IBM Corp, Armonk [NY], United States).
Graphical representations were made using commercial
software GraphPad Prism (Windows version 9.3.1;
GraphPad Software Inc, San Diego [CA], United States).
Frequencies and percentages were calculated for
categorical data and compared using Fischer’s exact
test. Continuous data were reported as medians with
interquartile range and compared using the Mann-Whitney U test.
RESULTS
A total of 11 consecutive lumpectomy cases with
stereotactic guidance targeting VAB markers and
localised with magnetic seeds were identified between
1 April 2021 and 28 February 2022, after excluding a
case in which multiple lesions localised with magnetic
seeds were excised in one specimen. A control group
of 11 consecutive lumpectomy cases with stereotactic
guidance targeting VAB markers managed with ROLL
between 2 May 2019 and 31 March 2021 was identified.
All lumpectomies were performed by at least one
specialist surgeon. There were seven specialist surgeons
in the magnetic seed cohort, two of whom performed the
lumpectomies in the ROLL cohort.
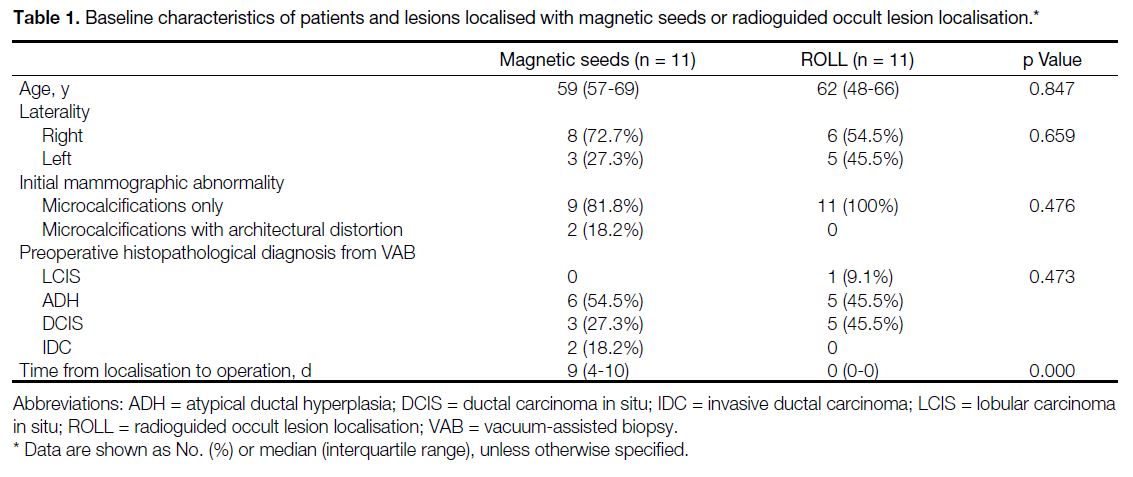
Baseline characteristics of the patients and lesions in both groups are shown in Table 1. Both groups of patients had
similar age ranges. All the lesions initially manifested
as microcalcifications, with or without architectural
distortion. The histopathology from the VAB specimens
in both cohorts were comparable, with most lesions
being either atypical ductal hyperplasia (ADH) or ductal carcinoma in situ (DCIS), and a minority of lobular
carcinoma in situ or invasive ductal carcinoma. None of
the patients included in the study received neoadjuvant
treatment prior to lumpectomy.
Table 1. Baseline characteristics of patients and lesions localised with magnetic seeds or radioguided occult lesion localisation.
The cases localised by magnetic seeds underwent
lumpectomy with or without sentinel lymph node
biopsy, with the magnetic seeds placed at a median of
9 days (interquartile range, 4-10) before surgery. All
cases guided by ROLL underwent lumpectomy within
the same day (Table 1).
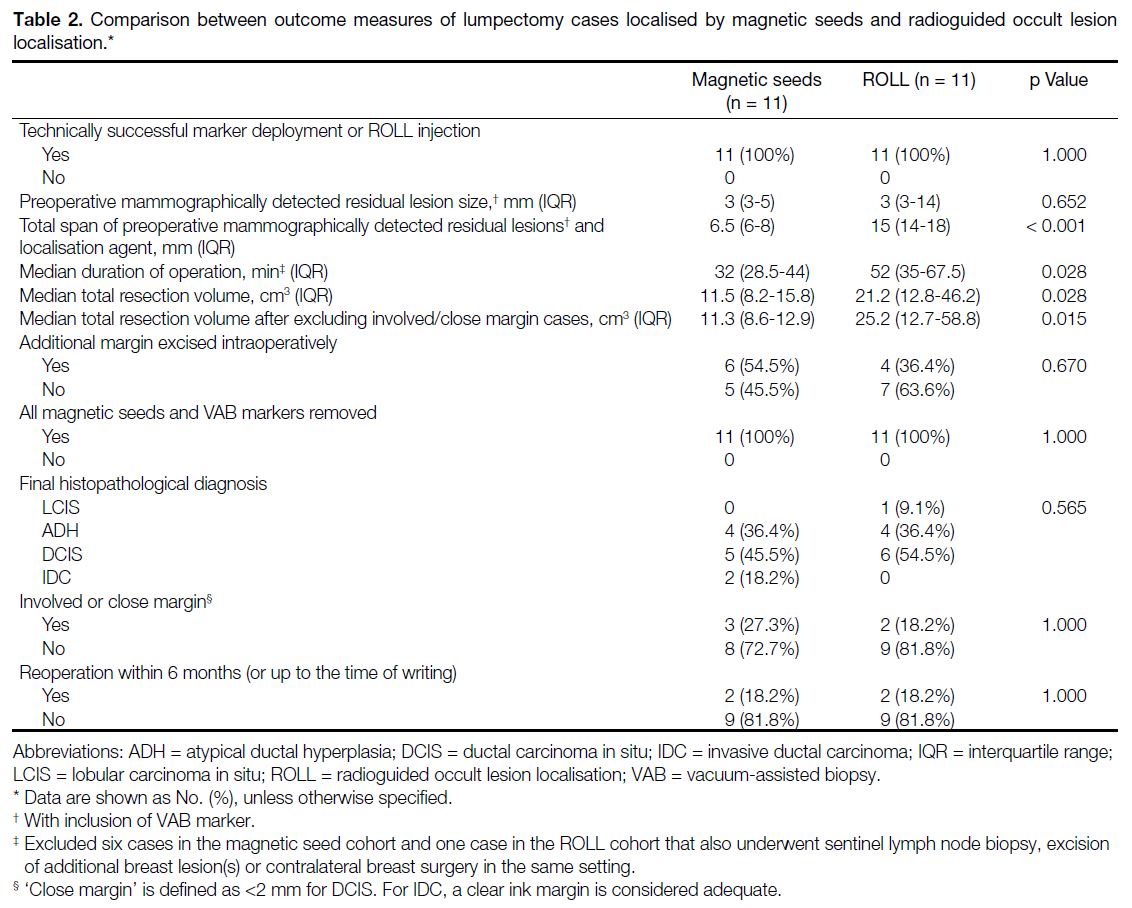
The outcomes of the lumpectomy cases localised
with magnetic seeds and ROLL are shown in Table 2. The technical success rates of marker deployment
and ROLL injection were 100%. The preoperative
mammographically detected post-VAB residual lesion
size with inclusion of the VAB marker in both groups
did not differ significantly (3 mm vs. 3 mm; p = 0.652).
After localisation, the total span of the preoperative
mammographically detected post-VAB residual lesion
(with inclusion of the VAB marker) and the localisation
agent (magnetic seed or iodinated contrast injected
during ROLL) was significantly lower in the magnetic
seed cohort compared with the ROLL cohort (6.5 mm
vs. 15 mm; p < 0.001) [Table 2].
Table 2. Comparison between outcome measures of lumpectomy cases localised by magnetic seeds and radioguided occult lesion localisation.
The median operative time was lower in the magnetic
seed cohort compared with the ROLL cohort (32 min
vs. 52 min; p = 0.028), after exclusion of the cases that
also underwent sentinel lymph node biopsy, excision of
additional breast lesion(s) or contralateral breast surgery in the same setting. However, there were six such
excluded cases in the magnetic seed cohort and one in the
ROLL cohort, rendering the sample size small (Table 2).
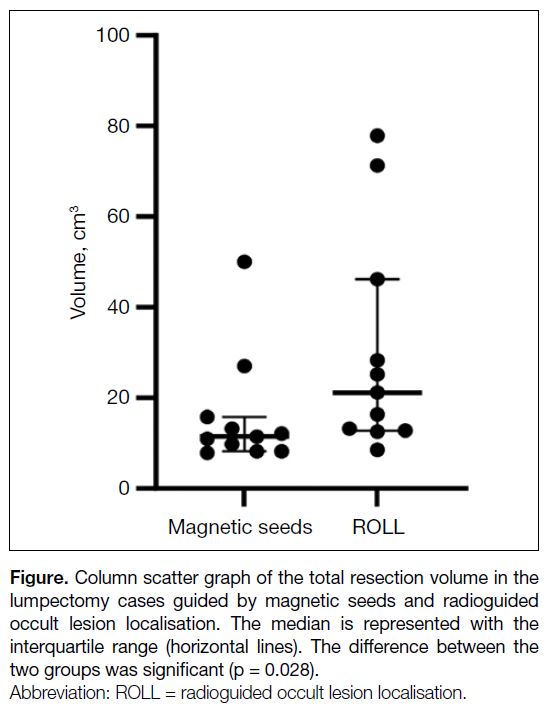
The total resection volume of the relevant specimens in
the cases localised by magnetic seeds was significantly
lower than in the group using ROLL (11.5 cm3 vs.
21.2 cm3; p = 0.028) [Table 2 and Figure]. If the cases
with involved or close margins (three in the magnetic
seed cohort and two in the ROLL cohort) were excluded
from analysis, the magnetic seeds group still achieved
a lower total resection volume (11.3 cm3 vs. 25.2 cm3; p = 0.015). There was a higher proportion of cases
with additional margins resected intraoperatively in the
magnetic seeds group (54.5% vs. 36.4%), but it did not
reach statistical significance (p = 0.670) [Table 2]. In two
cases of the ROLL cohort and one case in the magnetic
seed cohort, the measurements of the additional margins
taken were not fully documented and they were assumed
to be of negligible volume.
Figure. Column scatter graph of the total resection volume in the
lumpectomy cases guided by magnetic seeds and radioguided
occult lesion localisation. The median is represented with the
interquartile range (horizontal lines). The difference between the
two groups was significant (p = 0.028).
There was no incidence of magnetic seed migration in
the entire cohort. All magnetic seeds and VAB markers
were successfully removed from all patients (Table 2).
The final histopathological diagnoses of the lesions,
which were taken as the higher of the grades between
the VAB and lumpectomy specimens, were comparable
in both groups with no significant difference (p = 0.565)
[Table 2]. Two cases in the magnetic seed group and one
in the ROLL group were upgraded from ADH to DCIS
after surgical excision.
The margin clearance rates (72.7% vs. 81.8%) and
reoperation rates (18.2% vs. 18.2%) were similar in both
groups with no statistically significant difference (both
p = 1.000) [Table 2]. In all cases localised by magnetic
seeds, there was no margin involvement. Two cases
with DCIS did have close margins (<1 mm and 0.5 mm)
and underwent re-excision of margin and mastectomy,
respectively. No evidence of malignancy was detected
in the subsequent specimens obtained in either case,
except a small focus of ADH found in the patient who
had mastectomy. One patient who had DCIS with a close
margin (1.8 mm) opted against reoperation, proceeded
to adjuvant radiotherapy and has remained in remission
up to the time of this writing (9 months after her
operation). No significant postoperative complications
were recorded in the magnetic seed cohort. In the group
localised with ROLL, one case of DCIS had focally
involved margins and underwent re-excision. Residual DCIS was found in the re-excision specimen. There was
one case of DCIS with a close margin (<1 mm) upon
which a radiotherapy boost instead of re-excision was
decided after multidisciplinary team discussion. One
patient underwent wound exploration and clot evacuation
due to postoperative hematoma.
DISCUSSION
This study showed that a statistically significant
smaller total resection volume could be achieved with
magnetic seed localisation compared with ROLL, while
maintaining a similar margin clearance and reoperation
rate (Table 2). Although additional margins were
excised intraoperatively in a non-significantly higher
proportion of cases in the magnetic seed group, it did
not lead to an overall increased total resection volume,
which is the main determinant for cosmetic outcome.[7]
Previous studies on cosmetic outcomes after BCS found that exceeding a resection volume of 50 to 85 cm3 was
associated with a higher rate of cosmetic failure.[7] [8] [9] [10] [11] In
our study, there was only one case in the magnetic seed
cohort in which the total resection volume reached this
range (50.1 cm3). Two cases from the ROLL cohort
(77.8 cm3 and 71.3 cm3) fell within this range. None in the entire cohort exceeded 85 cm3.
The magnetic seeds were placed at a median of 9 days
before surgery. In contrast, all cases guided by ROLL
underwent same-day operation due to the constraint of
the nature of radioisotopes. Successful removal of the
magnetic seeds from the patient was achieved in all cases
(Table 1). The median operative time was lower in the
magnetic seed cohort (Table 2). No complications were
observed in the group localised with magnetic seeds,
while there was one case of postoperative hematoma
requiring surgical wound exploration in the group guided
by ROLL.
A possible reason for the improvement in resection
volume using magnetic seeds could be its ability to more precisely localise lesions, thus enhancing surgical
accuracy. With ROLL, the radioisotope, and hence the
area with highest radioactivity detected by the gamma
probe, infiltrates and disperses to adjacent tissues upon
injection, as supported by our data, resulting in the
surgeons resecting additional margins if residual activity
is detected in the surgical bed.[12] Intraductal injections
can also occur in ROLL, causing the radioisotopes
to be even more widely dispersed, in which case a
salvage localisation procedure would be necessary.[7] [13] [14]
Moreover, in the post-excision specimen radiograph,
it is easier to visualise the centre of the target if it is
guided by magnetic seeds than by ROLL.[15] One case
from the ROLL cohort in the study took up to four
specimen excisions before the VAB marker was seen
included within one of the specimens. It is possible that
the diffuse distribution of the radioisotopes could have
contributed to the need for repeated excisions in this
case. In comparison, a magnetic seed can pinpoint the
exact location of a lesion. The main factor that could
undermine its accuracy would be migration. Previous
studies showed that magnetic seed migration appears to
occur more frequently when performed under stereotactic
guidance owing to the ‘accordion’ effect, which the
release of breast compression causes the magnetic seed
to migrate along the direction of compression.[16] [17] This
effect could be mitigated by using less compression
before deploying the marker and by slowly releasing the
breast from compression after placement.[17] The reported
migration rates of magnetic seeds in previous studies
were low[17] [18] [19]; none of the magnetic seeds migrated in
this study.
Overall, the observations in this study echo those of
previous works.[1] [2] [3] [5] It shows that magnetic seeds are a
safe and effective localisation technique, and further
suggests that they can reduce total resection volume
compared with ROLL, without negatively impacting
the margin clearance and reoperation rates. They could
potentially benefit patients with early-stage breast
cancer, for which BCS with adjuvant radiotherapy is the
standard treatment. This is a large group of patients with
good survival rates, who face substantial psychological
stress.[6] [20] Although BCS preserves the breast, it results
in different degrees of breast asymmetry, which runs
the risk of affecting the psychosocial functioning of
these surviving cancer patients.[6] Improving the cosmetic
outcome without compromising the oncological margin
status may contribute to their psychosocial well-being
and quality of life.[7]
One major drawback of magnetic seeds is their high
cost in comparison with ROLL and other localisation
techniques, which may be a barrier to its adoption in
some centres. The logistical advantage of magnetic seeds
due to the decoupling of localisation and surgery may
be able to reduce delays in surgery and increase overall
efficiency.[7] Future cost-effectiveness analysis is required
and should take into consideration the overall efficiency,
which include surgical outcomes including cosmetic
results and patient satisfaction.
Limitations
This study has several limitations. First, the sample size was small, including patients only from two regional
hospitals, during the initial stage of magnetic seed
adoption. Second, surgeons might have resected a larger
amount of tissue in selected cases to ensure a clear
margin, particularly if previous VAB pathology results
already confirmed malignancy. This was assumed to be
balanced out by the relatively comparable distribution
of high risk versus malignant pathology of the VAB
specimens in both cohorts. Contrary to the concern for
selection bias, in the magnetic seed cohort of the current
study, there were two more invasive cancer cases than
in the ROLL cohort, which would presumably require
a wider margin. Third, the specimen weights were not
available in some cases, thus specimen volumes were
retrospectively calculated using the ellipse volume
formula, assuming that the surgical specimens were
ellipsoids. In practice, however, they are often irregularly
shaped. In a few cases, the measurements of some of the
additional margins excised were not fully documented,
which may affect the accuracy of the results.
CONCLUSION
This study demonstrated that localisation of non-palpable breast lesions with magnetic seeds can achieve a smaller
total resection volume compared with ROLL, without
affecting the margin clearance or reoperation rate.
Multicentre studies with larger sample size are required
to substantiate this finding and compare other surgical
outcomes of magnetic seeds and ROLL.
REFERENCES
1. Gera R, Tayeh S, Al-Reefy S, Mokbel K. Evolving role of
Magseed in wireless localization of breast lesions: systematic
review and pooled analysis of 1,559 procedures. Anticancer Res.
2020;40:1809-15. Crossref
2. Miller ME, Patil N, Li P, Freyvogel M, Greenwalt I, Rock L, et al.
Hospital system adoption of magnetic seeds for wireless breast
and lymph node localization. Ann Surg Oncol. 2021;28:3223-9. Crossref
3. Thekkinkattil D, Kaushik M, Hoosein MM, Al-Attar M, Pilgrim S, Gvaramadze A, et al. A prospective, single-arm, multicentre clinical
evaluation of a new localisation technique using non-radioactive
Magseeds for surgery of clinically occult breast lesions. Clin Radiol.
2019;74:974.e7-11. Crossref
4. Redfern RE, Shermis RB. Initial experience using Magseed for
breast lesion localization compared with wire-guided localization:
analysis of volume and margin clearance rates. Ann Surg Oncol.
2022;29:3776-83. Crossref
5. Tsui HL, Fung EP, Kwok KM, Wong LK, Lo LW, Mak WS.
Magnetic marker wireless localisation versus radioguided
localisation of nonpalpable breast lesions. Hong Kong J Radiol.
2021;24:247-56. Crossref
6. Waljee JF, Hu ES, Ubel PA, Smith DM, Newman LA,
Alderman AK. Effect of esthetic outcome after breast-conserving
surgery on psychosocial functioning and quality of life. J Clin
Oncol. 2008;26:3331-7. Crossref
7. Krekel N, Zonderhuis B, Muller S, Bril H, van Slooten HJ,
de Lange de Klerk E, et al. Excessive resections in breastconserving
surgery: a retrospective multicentre study. Breast J.
2011;17:602-9. Crossref
8. Cochrane RA, Valasiadou P, Wilson AR, Al-Ghazal SK,
Macmillan RD. Cosmesis and satisfaction after breast-conserving
surgery correlates with the percentage of breast volume excised.
Br J Surg. 2003;90:1505-9. Crossref
9. Olivotto IA, Rose MA, Osteen RT, Love S, Cady B, Silver B, et al.
Late cosmetic outcome after conservative surgery and radiotherapy:
analysis of causes of cosmetic failure. Int J Radiat Oncol Biol Phys.
1989;17:747-53. Crossref
10. Taylor ME, Perez CA, Halverson KJ, Kuske RR, Philpott GW,
Garcia DM, et al. Factors influencing cosmetic results after
conservation therapy for breast cancer. Int J Radiat Oncol Biol
Phys. 1995;31:753-64. Crossref
11. Vrieling C, Collette L, Fouquet A, Hoogenraad WJ, Horiot JH,
Jager JJ, et al. The influence of patient, tumor and treatment factors
on the cosmetic results after breast-conserving therapy in the
EORTC ‘boost vs. no boost’ trial. EORTC Radiotherapy and Breast
Cancer Cooperative Groups. Radiother Oncol. 2000;55:219-32. Crossref
12. Postma EL, Verkooijen HM, van Esser S, Hobbelink MG, van der
Schelling GP, Koelemij R, et al. Efficacy of ‘radioguided occult
lesion localisation’ (ROLL) versus ‘wire-guided localisation’
(WGL) in breast conserving surgery for non-palpable breast cancer:
a randomised controlled multicentre trial. Breast Cancer Res Treat.
2012;136:469-78. Crossref
13. Luini A, Zurrida S, Paganelli G, Galimberti V, Sacchini V,
Monti S, et al. Comparison of radioguided excision with wire
localization of occult breast lesions. Br J Surg. 1999;86:522-5. Crossref
14. Rampaul RS, MacMillan RD, Evans AJ. Intraductal injection of the
breast: a potential pitfall of radioisotope occult lesion localization.
Br J Radiol. 2003;76:425-6. Crossref
15. Zacharioudakis K, Down S, Bholah Z, Lee S, Khan T, Maxwell AJ,
et al. Is the future magnetic? Magseed localisation for non palpable
breast cancer. A multi-centre non randomised control study. Eur J
Surg Oncol. 2019;45:2016-21. Crossref
16. Esserman LE, Cura MA, DaCosta D. Recognizing pitfalls in early
and late migration of clip markers after imaging-guided directional
vacuum-assisted biopsy. Radiographics. 2004;24:147-56. Crossref
17. Lamb LR, Bahl M, Specht MC, D’Alessandro HA, Lehman CD.
Evaluation of a nonradioactive magnetic marker wireless
localization program. AJR Am J Roentgenol. 2018;211:940-5. Crossref
18. Singh P, Scoggins ME, Sahin AA, Hwang RF, Kuerer HM,
Caudle AS, et al. Effectiveness and safety of Magseed-localization
for excision of breast lesions: a prospective, phase IV trial. Ann
Surg Open. 2020;1:e008. Crossref
19. Harvey JR, Lim Y, Murphy J, Howe M, Morris J, Goyal A, et al.
Safety and feasibility of breast lesion localization using magnetic
seeds (Magseed): a multi-centre, open-label cohort study. Breast
Cancer Res Treat. 2018;169:531-6. Crossref
20. Institute of Medicine (US) and National Research Council (US)
National Cancer Policy Board. Hewitt M, Herdman R, Holland
J, editors. Meeting Psychosocial Needs of Women with Breast
Cancer. Washington (DC): National Academies Press (US); 2004.