The Significance of Computed Tomography–Detected Breast Lesions
ORIGINAL ARTICLE CME
Hong Kong J Radiol 2024 Sep;27(3):e140-6 | Epub 4 September 2024
The Significance of Computed Tomography–Detected Breast Lesions
LY Lam, KM Chu, HHC Tsang, WC Wai, JLF Chiu
Department of Radiology and Imaging, Queen Elizabeth Hospital, Hong Kong SAR, China
Correspondence: Dr LY Lam, Department of Radiology and Imaging, Queen Elizabeth Hospital, Hong Kong SAR, China. Email: lly858@ha.org.hk
Submitted: 14 March 2023; Accepted: 5 October 2023.
Contributors: LYL, HHCT and WCW designed the study and acquired the data. All authors analysed the data. LYL drafted the manuscript. KMC, HHCT, WCW and JLFC critically revised the manuscript for important intellectual content. All authors had full access to the data,
contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of Interest: All authors have disclosed no conflicts of interest.
Funding/Support: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data Availability: All data generated or analysed during the present study are available from the corresponding author on reasonable request.
Ethics Approval: This research was approved by the Kowloon Central Cluster and Kowloon East Cluster Research Ethics Committee of Hospital Authority, Hong Kong (Ref No.: KC/KE-22-0059/ER-4). The requirement for patient consent was waived by the Committee due to the retrospective nature of the research.
Abstract
Introduction
With ever-increasing computed tomography (CT) utilisation, more breast lesions are incidentally
detected. We sought to investigate the yield of undiagnosed cancers from incidental CT-detected breast lesions.
Imaging features were compared with the pathological diagnoses.
Methods
A retrospective analysis of CT examinations in a regional hospital in Hong Kong between January 2018
and December 2020 was performed. Patients without a history of breast diseases whose CT reports contained the
keyword ‘breast’ and who were referred for a formal breast examination were included. Two radiologists reviewed the
CT reports and lesion characteristics were recorded. The diagnostic accuracy of different CT features was evaluated.
Results
A total of 219 breast lesions were included. Forty-eight lesions (21.9%) were malignant. Patients with
malignant diagnoses were older in age than those with benign diagnoses (mean age: 67.58 vs. 56.60 years; p = 0.05). Spiculation, irregularity, rim and heterogeneous enhancement, as well as the presence of abnormal lymph nodes were useful in predicting malignancy. Lesion size and presence of calcifications were not useful for predicting
the pathological diagnosis.
Conclusion
More than 20% of breast lesions detected incidentally in CT examinations were malignant. The presence
of spiculation and irregularity were positive predictive factors. A careful review of the breasts on CT studies including
the chest should always be part of routine practice.
Key Words: Breast; Breast neoplasms; Diagnostic imaging; Incidental findings; Lymph nodes
中文摘要
電腦斷層掃描檢測到乳腺病變的重要性
林樂宜、朱嘉敏、曾凱晴、衛頴莊、趙朗峰
引言
隨着電腦斷層掃描使用愈趨普及,越來越多的乳腺病變被偶然發現。我們調查電腦斷層掃描偶然檢測到的乳腺病變中未確診癌症的發生率,並比較影像學特徵與病理診斷。
方法
我們就2018年1月至2020年12月期間香港某地區醫院的電腦斷層掃描檢查進行回顧性分析。本研究納入沒有乳腺疾病史而電腦斷層掃描報告中包含「乳腺」關鍵字並轉診進行正式乳腺檢查的患者。兩名放射科醫生審查了電腦斷層掃描報告。本研究記錄了患者的病變特徵,並評估不同電腦斷層掃描特徵的診斷準確性。
結果
本研究共納入219個乳腺病灶,48個病變(21.9%)為惡性。診斷為惡性病變的患者年齡比診斷為良性病變的患者年齡大(平均年齡:67.58歲與56.60歲;p = 0.05)。毛邊、不規則、邊緣和不均勻強化以及異常淋巴結的存在有助預測惡性腫瘤。病灶大小和鈣化的存在無助預測病理診斷。
結論
電腦斷層掃描檢查偶然發現的乳腺病變中20%以上為惡性。存在毛邊和不規則是陽性預測因素。透過電腦斷層掃描檢查仔細檢查胸部乳腺應成為常規。
INTRODUCTION
Breast cancer is one of the commonest cancers in Hong
Kong, comprising 28.4% of female cancers in 2020.[1]
In Hong Kong, mammography and sonography are the
preferred initial modalities in the evaluation of breast
lesions.[2] In some other countries, mammography is the
mainstay for breast cancer screening.[3] In an era with
increasing utilisation of computed tomography (CT),
more breast lesions are detected incidentally when CT
scanning is performed for other indications such as
pulmonary or cardiac conditions.[4] [5] [6] Although dedicated
mammography and sonography are still required for
a better evaluation of the lesions, it is still important
for radiologists to detect imaged breast lesions and to
characterise them when such lesions are encountered on
a CT scan. With an increased detection of undiagnosed
breast cancer, a prompt referral of suspicious lesions for
further investigation can help improve patient outcome.
We aimed to investigate the yield of breast cancers from
incidentally detected breast lesions on CT in Hong Kong.
Their imaging features were correlated and compared
with the final pathological diagnoses.
METHODS
A retrospective analysis of the CT examinations scanned
in Queen Elizabeth Hospital from 1 January 2018 through
31 December 2020 was performed. Patients whose CT
reports contained the keyword ‘breast’ and were referred for a formal breast examination were included. The CT
reports were derived from the Radiological Information
System and Picture Archiving and Communication
System, which is a system managed by Hospital
Authority. Patients who had a history of breast diseases
or breast surgeries were excluded from the study.
The CT scanners used in this study included SOMATOM
Force Ultra-Fast Dual Source CT Scanner (Siemens
Healthcare, Erlangen, Germany), Aquilion CXL
128 Slice CT Scanner (Toshiba, Tochigi, Japan), and
Aquilion Prime CT Scanner (Canon Medical Systems,
Tochigi, Japan), with a section thickness of 5 mm. The
types of contrast used for enhanced procedures were
iohexol (Omnipaque 350; GE HealthCare, Milwaukee
[WI], US) and iodixanol (Visipaque 320; GE HealthCare,
Milwaukee [WI], US), with a standard adult dose of 90
mL, administered via a pump injector. In examinations of
the abdomen requiring injected contrast material imaged
in different phases, the contrast was administered for the
arterial phase at 3.5 mL/s or in the portal venous phase at
2.5 mL/s with a standard 70-second delay.
The CT images were reviewed by and commented on
by two experienced radiologists (with 6 and 8 years’
experience in breast imaging, respectively) who were
blinded to the diagnostic outcome. As there is no formal
lexicon for breast lesions detected in a CT scan, the descriptors used in this study were adapted from the
Breast Imaging and Reporting Data System terminology
for magnetic resonance imaging lexicons (5th edition).[7] [8]
The axillary lymph nodes were considered abnormal if:
(1) their longest-to-shortest axis ratio was <2; (2) they
lacked a fatty hilum; (3) there was cortical thickening of
>3 mm; or (4) their cortices were eccentric.[9]
Continuous variables were presented as mean ± standard
deviation, and categorical variables were presented
as frequencies. The Mann-Whitney U test was used to
evaluate the distribution of continuous data. Fisher’s
exact test was performed to assess the correlation of
the CT features with final pathological diagnosis. The
specificity and sensitivity for malignancy were calculated
for the significant CT features. A p value of < 0.05 was
considered to be statistically significant.
RESULTS
Demographics and Study Cohort
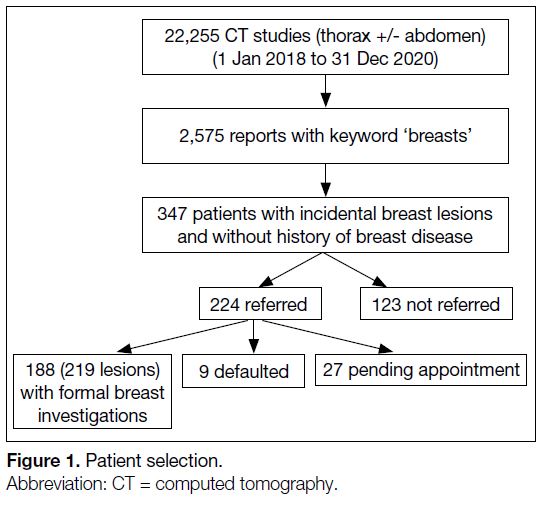
A total of 22,255 CT studies of the thorax with or
without abdominal regions were performed during the
study period. Among these CT examinations, 2,575 of
the reports contained the keyword ‘breast’. A total of
347 patients without history of prior breast disease or
surgery were noted to have one or more incidental breast
lesions in the CT studies; 345 were women and two were
male. A total of 224 patients were referred for further
formal breast assessment and investigation, among
which 188 had subsequent formal breast investigations,
nine had defaulted appointments, and 27 were still
pending appointments at the time of the study. Among
these 188 patients (186 female and 2 male), 164 patients
had a solitary lesion, while 17 patients had two lesions
and seven patients had three lesions, for a total of 219
incidentally detected breast lesions (Figure 1).
Figure 1. Patient selection
Referral Rates
The overall referral rate for formal breast investigations during the study period was 64.6%. It was lowest in
2018 (61.0%) and highest in 2019, which was 70.8%.
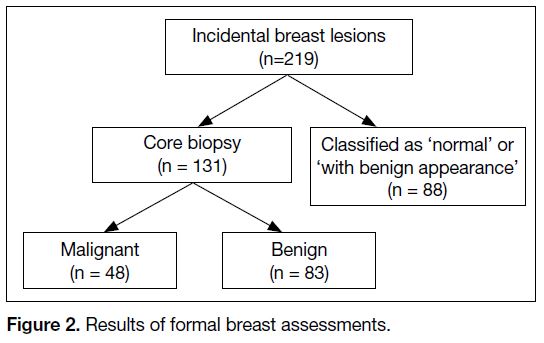
Formal Breast Assessment Findings
Among the 219 breast lesions undergoing formal breast
assessment, 88 were classified as ‘normal’ or ‘with benign
appearance’ by clinical examination, mammography,
and ultrasonography. The remaining 100 patients have
undergone ultrasound-guided biopsy in our institute. In
these patients, 83 lesions were found to be benign and 48
lesions were malignant (Figure 2), most of which were
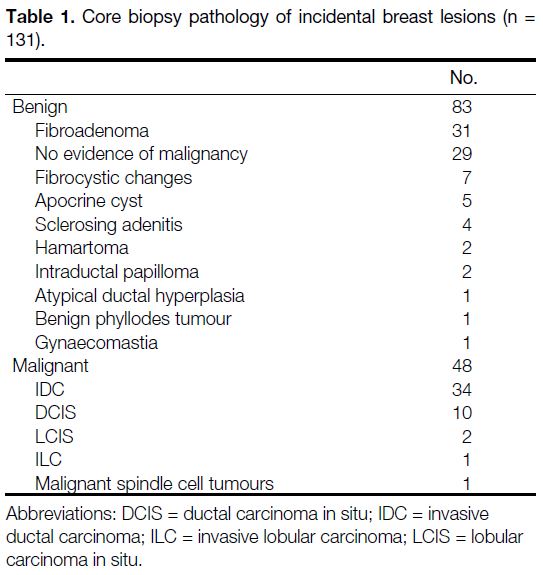
invasive ductal carcinoma (Table 1).
Figure 2. Results of formal breast assessments
The malignancy rate was 21.9% (48 out of 219 lesions).
Patients with malignant lesions were likely to be older
in age compared with those with benign findings (mean
age: 67.58 vs. 56.60 years, p = 0.05).
Table 1. Core biopsy pathology of incidental breast lesions (n = 131).
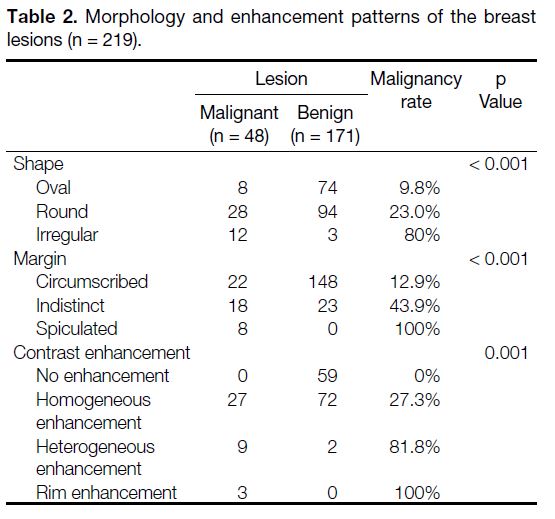
Lesion Characteristics
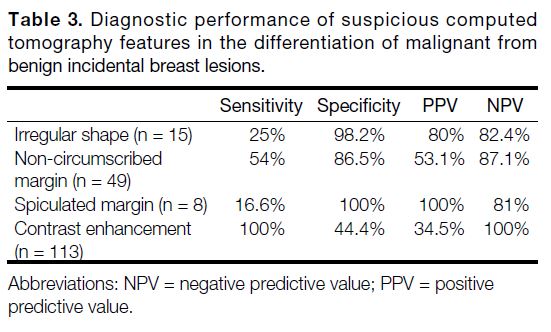
CT measurement showed that the malignant lesions
(mean size: 1.56 cm) were larger than the benign lesions
(mean size: 1.23 cm) but not statistically significant
(p = 0.08). Among the morphological characteristics
of the breast lesions (Table 2), more lesions with an
irregular shape or non-circumscribed margin were
diagnosed as malignant (p ≤ 0.001). The malignancy
rate (i.e., positive predictive value [PPV]) of all irregular
lesions was 80%. The sensitivity and specificity of an
irregular shape were 25% and 98.2%, respectively,
while the malignancy rate of all non-circumscribed
lesions was 53.1%. The calculated sensitivity and
specificity of a non-circumscribed margin were 54%
and 86.5%, respectively. Among the two descriptors for
non-circumscribed margins, a spiculated margin had a
malignancy rate of 100% with sensitivity and specificity
of 16.6% and 100%, respectively, and is more indicative
of malignancy (p < 0.05) [Table 3 and Figure 3].
Table 2. Morphology and enhancement patterns of the breast lesions (n = 219)
Table 3. Diagnostic performance of suspicious computed
tomography features in the differentiation of malignant from
benign incidental breast lesions
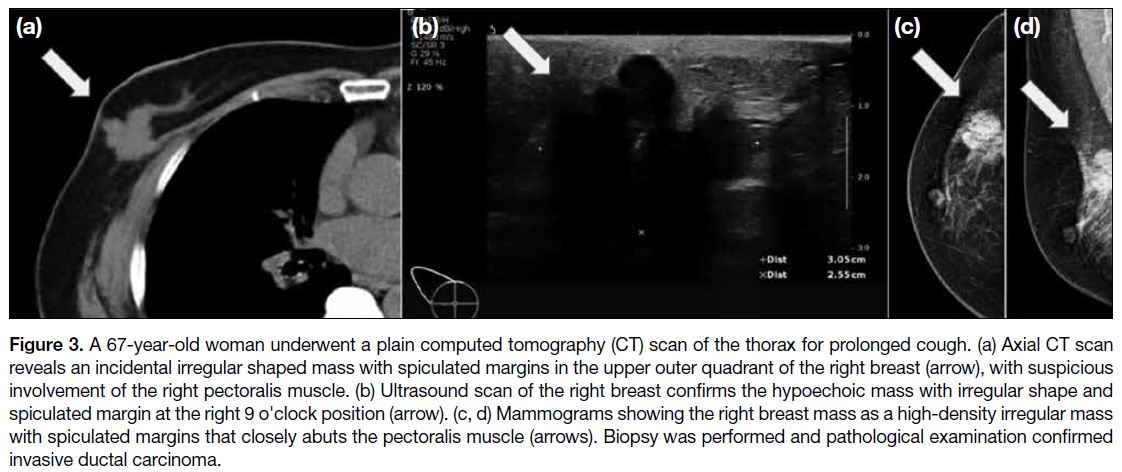
Figure 3. A 67-year-old woman underwent a plain computed tomography (CT) scan of the thorax for prolonged cough. (a) Axial CT scan
reveals an incidental irregular shaped mass with spiculated margins in the upper outer quadrant of the right breast (arrow), with suspicious
involvement of the right pectoralis muscle. (b) Ultrasound scan of the right breast confirms the hypoechoic mass with irregular shape and
spiculated margin at the right 9 o'clock position (arrow). (c, d) Mammograms showing the right breast mass as a high-density irregular mass
with spiculated margins that closely abuts the pectoralis muscle (arrows). Biopsy was performed and pathological examination confirmed
invasive ductal carcinoma
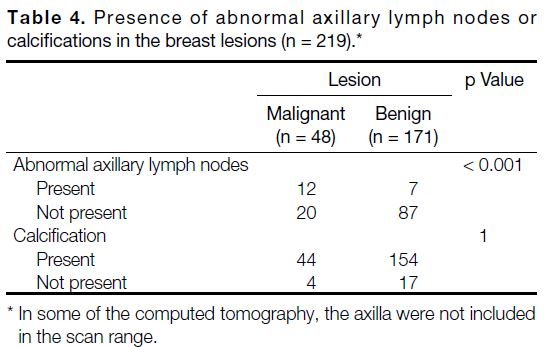
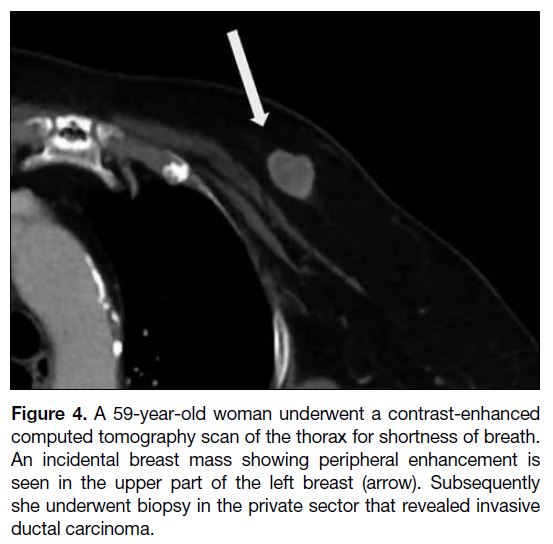
Four biopsy-proven malignant lesions contained
calcification. However, the association between
calcification and malignancy of the lesions was not
statistically significant (p > 0.05) [Table 4 and Figure 4].
Table 4. Presence of abnormal axillary lymph nodes or calcifications in the breast lesions (n = 219)
Figure 4. A 59-year-old woman underwent a contrast-enhanced
computed tomography scan of the thorax for shortness of breath.
An incidental breast mass showing peripheral enhancement is
seen in the upper part of the left breast (arrow). Subsequently
she underwent biopsy in the private sector that revealed invasive
ductal carcinoma
Contrast Enhancement
A total of 172 lesions were evaluated in contrast-enhanced CT scans, with 113 of them showing contrast
enhancement (Table 2). All of the malignant lesions
showed enhancement. The sensitivity and specificity
of contrast enhancement were 100% and 44.4%,
respectively, for a negative predictive value of 100% for
lack of enhancement (Table 3). Furthermore, all lesions
that showed rim enhancement were malignant, giving a
malignancy rate of 100% (p < 0.05) with specificity of
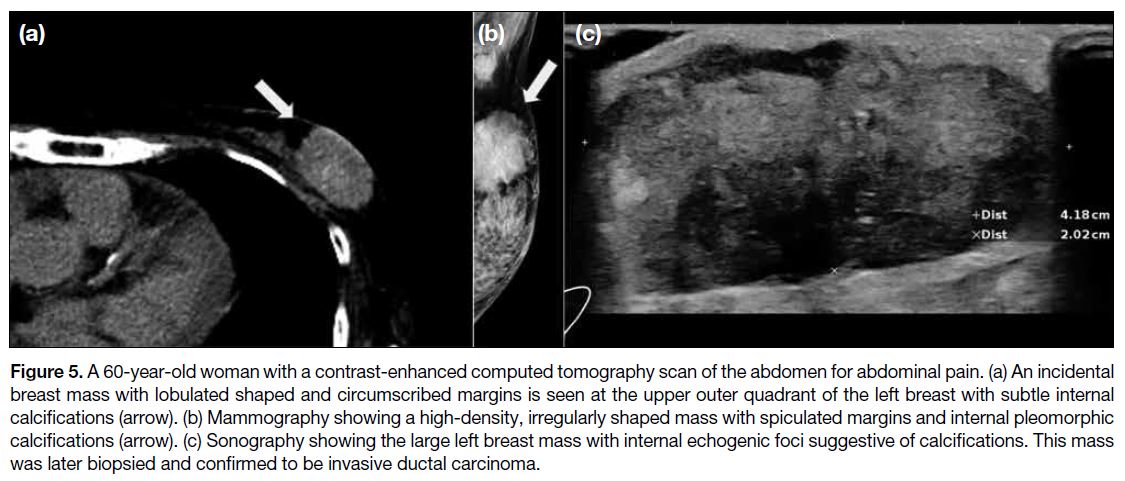
100% (Table 2 and Figure 5).
Figure 5. A 60-year-old woman with a contrast-enhanced computed tomography scan of the abdomen for abdominal pain. (a) An incidental
breast mass with lobulated shaped and circumscribed margins is seen at the upper outer quadrant of the left breast with subtle internal
calcifications (arrow). (b) Mammography showing a high-density, irregularly shaped mass with spiculated margins and internal pleomorphic
calcifications (arrow). (c) Sonography showing the large left breast mass with internal echogenic foci suggestive of calcifications. This mass
was later biopsied and confirmed to be invasive ductal carcinoma.
Presence of Axillary Lymph Nodes
The axillary regions were included in the CT scan
range in 126 patients. A total of 19 patients were found
to have abnormal axillary lymph nodes, of which 12
of them have biopsy-proven malignant breast lesions.
The association between presence of abnormal-looking
axillary lymph nodes and breast malignancy was found
to be statistically significant (p < 0.001) [Table 4].
DISCUSSION
Our study shows an increase in referral rate for dedicated
breast imaging from 2018 to 2020, with increased
reporting of CT-detected breast lesions. Despite a similar
number of total CT scans done in our institute annually,
this may be due to an increased awareness of CT-detected
breast lesions leading to referral to the breast imaging
units for characterisation.
In our study, 21.9% of the incidental CT-detected breast lesions were proven to be malignant after biopsy in the
breast unit, i.e., out of the 22,255 CT studies performed
in 2018 to 2020, 43 patients (five of them with more than
one incidental breast tumour) were ultimately diagnosed
with unsuspected breast cancer. Hence, the extrapolated
breast cancer detection rate by CT scans is 1.9 cases per
1000 population based on our findings. A retrospective
review by a local public hospital performed in the 5-year
period from 1998 to 2002 showed that the breast cancer
detection rate by mammogram is 5 cases per 1000
population,[2] in agreement with the concept that CT scan
alone is not a better screening test than mammography.
Of the incidentally detected breast cancers in our study,
most cases were invasive ductal carcinoma (70.8%)
[Table 1], similar to the incidence of invasive ductal
carcinoma in the general population of 75%.[10] [11] Ductal
carcinoma in situ accounted for 20.8% of the incidentally
detected breast cancers in our study (Table 1). Although
CT lacks the resolution for microcalcifications, these
cases were detected as breast masses.[12]
The most suspicious features for malignancy were found
to be an irregular shape (malignancy rate of 80%) and
spiculated margin (malignancy rate of 100%) [Table 2]. These results were in keeping with other studies
across different modalities including mammography
and sonography. Liberman et al[13] reported a PPV for
malignancy of 73% for irregular shape and 81% for
spiculated margins for mammographic studies. Inoue
et al[14] reported a PPV for malignancy of 99% for irregular
shape and 100% for spiculated margins for CT using
dynamic dedicated breast CT. Stavros et al[15] reported a
PPV for malignancy of 91.8% for spiculated lesions on
sonography.
On the other hand, we found that oval shape (malignancy
rate of 9.8%) and circumscribed margins (malignancy
rate of 12.9%) are more indicative of benignity (Table 2). These results are also similar in the study by Moyle et al.[16]
The presence of CT-detected calcifications in breast
lesions does not show a statistically significant
association with the final pathology diagnosis (Table 4). In this study, only four biopsy-proven malignant
lesions contained calcification, while the other visible
calcifications were associated with benign entities.
This is likely due to the fact that CT has limited spatial
resolution. Microcalcifications <0.5 mm that are more
likely associated with malignancy cannot be detected on non-dedicated CT.[17] Lindfors et al[18] found that CT
was worse than mammography for visualisation of microcalcifications.
In our study, all of the biopsy-proven breast
malignancies showed contrast enhancement with
different enhancement patterns. Among these patterns,
rim enhancement and heterogeneous enhancement were
more indicative of malignancy (malignancy rate of
100% and 81.8%, respectively) [Table 2]. These results
are similar to the findings by Moyle et al[16] and Agrawal
et al[19] but are opposite from the study by Inoue et al,[14]
who made use of dedicated breast CT for their study.
The discrepancy can be due to the difference in timing
of image acquisition in the CT studies in our study. Also,
malignant breast tumours show rapid contrast uptake
and washout, which is well known as a type 3 curve.[20]
However, one limitation of our study is that the timing
of the contrast administration was not fixed for all the
CT studies, therefore such contrast enhancement pattern
cannot be demonstrated.
In our study, the association between the presence of
abnormal-looking axillary lymph nodes and breast
malignancy was found to be statistically significant
(Table 4). Therefore, evaluation of axillary lymph nodes
is essential as part of the triple assessment and before
sentinel lymph node biopsy. Although axillary ultrasound
is more convenient, it is found that the combination of
axillary ultrasound, breast CT, and magnetic resonance
imaging of the breast yields a better accuracy rate than
the use of a single imaging modality.[21]
CONCLUSION
The breasts are an area for review by CT radiologists, as
more breast lesions are being detected incidentally in CT
examinations. This study has shown that nearly one in
four incidental breast lesions leads to a diagnosis of breast
cancer, particularly in older adults, lesions demonstrating
spiculation, irregularity or rim enhancement, and in
the presence of abnormal axillary lymph nodes. The
detection of these incidental lesions can facilitate a
timely referral for a formal breast examination, prompt
patient management, and better disease outcome.
REFERENCES
1. Centre for Health Protection, Department of Health, Hong Kong
SAR Government. Breast cancer. January 2024. Available
from: https://www.chp.gov.hk/en/healthtopics/content/25/53.html#:~:text=It%20accounted%20for%2028.4%25%20of,of%20breast%20cancer%20in%20males.&text=In%202020%2C%204956%20new%20cases,per%20100%20000%20female%20population. Accessed 2 Mar 2023.
2. Lui CY, Lam HS, Chan LK, Tam KF, Chan CM, Leung TY, et al.
Opportunistic breast cancer screening in Hong Kong; a revisit of the
Kwong Wah Hospital experience. Hong Kong Med J. 2007;13:106-13.
3. Zeng B, Yu K, Gao L, Zeng X, Zhou Q. Breast cancer screening
using synthesized two-dimensional mammography: a systematic
review and meta-analysis. Breast. 2021;59:270-8. Crossref
4. Molteni T, Patrique PO, Niasme E, Haefliger L, Vo QD. Incidental
breast lesion on chest CT scan: a review. Obstet Gynecol Int J.
2022;13:15-7. Crossref
5. Son JH, Jung HK, Song JW, Baek HJ, Doo KW, Kim W, et al.
Incidentally detected breast lesions on chest CT with US
correlation: a pictorial essay. Diagn Interv Radiol. 2016;22:514-8. Crossref
6. Monzawa S, Washio T, Yasuoka R, Mitsuo M, Kadotani Y,
Hanioka K. Incidental detection of clinically unexpected breast
lesions by computed tomography. Acta Radiol. 2013;54:374-9. Crossref
7. Spak DA, Plaxco JS, Santiago L, Dryden MJ, Dogan BE. BI-RADS ® fifth edition: a summary of changes. Diagn Interv Imaging. 2017;98:179-90. Crossref
8. Magny SJ, Shikhman R, Keppke AL. Breast Imaging Reporting
and Data System. 2022 Aug 29. In: StatPearls [Internet]. Available
from: https://www.ncbi.nlm.nih.gov/books/NBK459169/.
Accessed 30 Dec 2022.
9. Lee HJ, Nguyen AT, Song MW, Lee JE, Park SB, Jeong WG,
et al. Prediction of residual axillary nodal metastasis following
neoadjuvant chemotherapy for breast cancer: radiomics analysis
based on chest computed tomography. Korean J Radiol.
2023;24:498-511. Crossref
10. Mannu GS, Wang Z, Broggio J, Charman J, Cheung S, Kearins O,
et al. Invasive breast cancer and breast cancer mortality after
ductal carcinoma in situ in women attending for breast screening
in England, 1988-2014: population based observational cohort
study. BMJ. 2020;369:m1570. Crossref
11. American Cancer Society. Breast Cancer Facts & Figures 2019-2020. 2019. Available from: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/breast-cancer-facts-and-figures/breast-cancer-facts-and-figures-2019-2020.pdf. Accessed 3 Jan 2022.
12. Vaidya Y, Vaidya P, Vaidya T. Ductal carcinoma in situ of the breast. Indian J Surg. 2015;77:141-6. Crossref
13. Liberman L, Abramson AF, Squires FB, Glassman JR, Morris EA,
Dershaw DD. The breast imaging reporting and data system:
positive predictive value of mammographic features and final
assessment categories. AJR Am J Roentgenol. 1998;171:35-40. Crossref
14. Inoue M, Sano T, Watai R, Ashikaga R, Ueda K, Watatani M, et al.
Dynamic multidetector CT of breast tumors: diagnostic features and
comparison with conventional techniques. AJR Am J Roentgenol.
2003;181:679-86. Crossref
15. Stavros AT, Thickman D, Rapp CL, Dennis MA, Parker SH,
Sisney GA. Solid breast nodules: use of sonography to distinguish
between benign and malignant lesions. Radiology. 1995;196:123-34. Crossref
16. Moyle P, Sonoda L, Britton P, Sinnatamby R. Incidental breast
lesions detected on CT: what is their significance? Br J Radiol.
2010;83:233-40. Crossref
17. Gazi PM, Yang K, Burkett GW Jr, Aminololama-Shakeri S,
Seibert JA, Boone JM. Evolution of spatial resolution in breast CT
at UC Davis. Med Phys. 2015;42:1973-81. Crossref
18. Lindfors KK, Boone JM, Nelson TR, Yang K, Kwan AL, Miller DF. Dedicated breast CT: initial clinical experience.
Radiology. 2008;246:725-33. Crossref
19. Agrawal G, Su MY, Nalcioglu O, Feig SA, Chen JH. Significance
of breast lesion descriptors in the ACR BI-RADS MRI lexicon.
Cancer. 2009;115:1363-80. Crossref
20. Yang SN, Li FJ, Chen JM, Zhang G, Liao YH, Huang TC.
Kinetic curve type assessment for classification of breast lesions
using dynamic contrast-enhanced MR imaging. PLoS One.
2016;11:e0152827. Crossref
21. Aktaş A, Gürleyik MG, Aydın Aksu S, Aker F, Güngör S.
Diagnostic value of axillary ultrasound, MRI, and 18F-FDG-PET/CT in determining axillary lymph node status in breast cancer
patients. Eur J Breast Health. 2021;18:37-47. Crossref