Rupture of Renal Pelvis Secondary to Obstructing Calculus in Menkes Disease: A Case Report
CASE REPORT
Hong Kong J Radiol 2023 Sep;26(3):194-7 | Epub 4 Sep 2023
Rupture of Renal Pelvis Secondary to Obstructing Calculus in Menkes Disease: A Case Report
TM Chiu, KKF Fung, EYL Kan
Department of Radiology, Hong Kong Children’s Hospital, Hong Kong SAR, China
Correspondence: Dr TM Chiu, Department of Radiology, Hong Kong Children’s Hospital, Hong Kong SAR, China. Email: ctm537@ha.org.hk
Submitted: 20 Nov 2021; Accepted: 7 Apr 2022.
Contributors: All authors designed the study, acquired and analysed the data. TMC drafted the manuscript. KKFF and EYLK critically revised the manuscript for important intellectual content. All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of Interest: As an editor of the journal, KKFF was not involved in the peer review process. Other authors have disclosed no conflicts of interest.
Funding/Support: This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data Availability: All data generated or analysed during the present study are available from the corresponding author on reasonable request.
Ethics Approval: The study was approved by the Hong Kong Children’s Hospital Research Ethics Committee (Ref No.: HKCH-REC-2021-017). The patient was treated in accordance with the Declaration of Helsinki. Consent for publication was obtained from the patient’s parent.
BACKGROUND
Menkes disease is a rare X-linked hereditary multisystem
disorder due to a defect in copper metabolism caused
by a mutation in the ATP7A gene.[1] Patients can present
with neurodegenerative manifestations and multiple
connective tissue abnormalities.[1] We report the case of
a 4-year-old boy, known to have Menkes disease, who
presented with an obstructive ureteric stone complicated
by rupture of the renal pelvis.
CASE REPORT
Our patient was diagnosed with Menkes disease at 6
months of age. Since then, he has developed recurrent
urinary tract infections, attributed to the presence of
multiple urinary bladder diverticula. He has received
copper histidine injections since around 8 months of age
and clean intermittent catheterisation since 19 months of
age.
The patient presented with an episode of abdominal
distension and septicaemia at the age of 4. There was
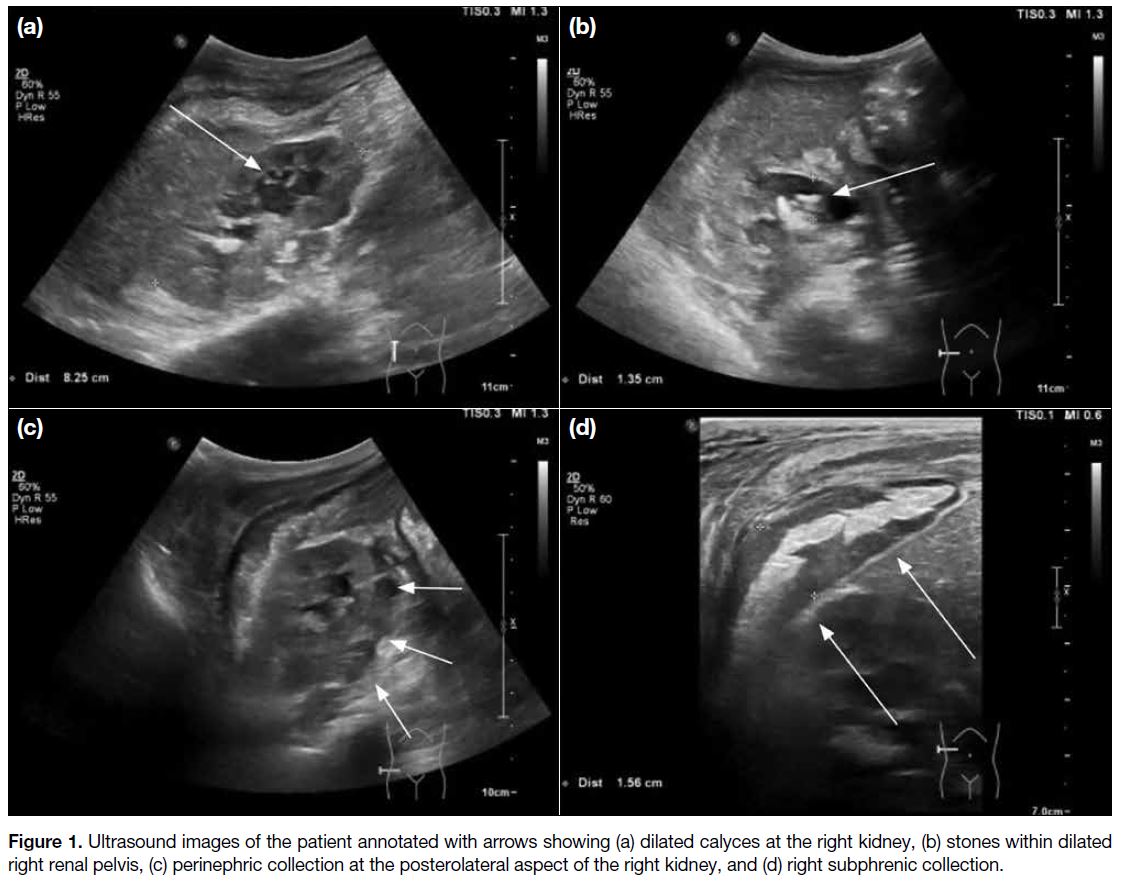
no history of recent surgery or trauma. Ultrasound of the abdomen and pelvis revealed right-sided
hydronephrosis and fluid collections around the right
perinephric and right subphrenic regions (Figure 1).
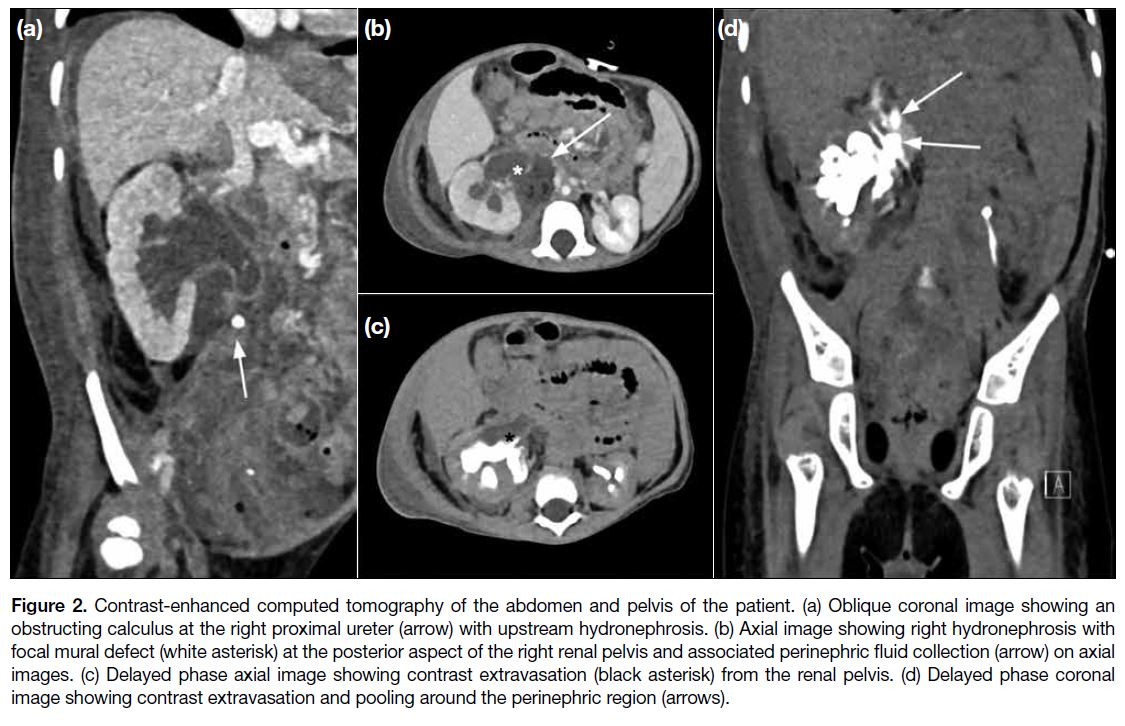
Further contrast-enhanced computed tomography (CT)
scan of the abdomen and pelvis showed an obstructing
stone at the right proximal ureter with gross upstream
hydroureteronephrosis. Delayed phase images were
subsequently obtained at 60 minutes post injection and
confirmed the presence of a mural defect at the posterior
aspect of the right renal pelvis with contrast extravasation
from the corresponding area and contrast pooling around
the right perinephric region (Figure 2). A ruptured right
renal pelvis was diagnosed.
Figure 1. Ultrasound images of the patient annotated with arrows showing (a) dilated calyces at the right kidney, (b) stones within dilated
right renal pelvis, (c) perinephric collection at the posterolateral aspect of the right kidney, and (d) right subphrenic collection.
Figure 2. Contrast-enhanced computed tomography of the abdomen and pelvis of the patient. (a) Oblique coronal image showing an
obstructing calculus at the right proximal ureter (arrow) with upstream hydronephrosis. (b) Axial image showing right hydronephrosis with
focal mural defect (white asterisk) at the posterior aspect of the right renal pelvis and associated perinephric fluid collection (arrow) on axial
images. (c) Delayed phase axial image showing contrast extravasation (black asterisk) from the renal pelvis. (d) Delayed phase coronal
image showing contrast extravasation and pooling around the perinephric region (arrows).
Following diagnosis, insertion of a double-J stent was
attempted for urinary diversion but was unsuccessful
due to difficulty in identifying the ureteric orifice in the
presence of multiple urinary diverticula. Percutaneous
nephrostomy was performed instead the following
day. Ultrasound-guided drainage of a retroperitoneal
collection was also performed subsequently for control
of sepsis.
Open pyeloplasty was performed around 2 months after
the first presentation as underlying ureteric stricture was
suspected. Surgery was unsuccessful and complicated
by persistent stricture. Further balloon dilatation was
attempted but this also failed. After multidisciplinary
discussion, a decision was made for a long-term internal
ureteric stent to remain in situ. Our patient is now well
following removal of the percutaneous nephrostomy
catheter. A ureteric stent remains in situ and clean
intermittent catheterisation continues.
DISCUSSION
Menkes disease has an estimated incidence of 1 in
35 000 population[2] to 1 in 360 000 population[1], varying
widely in different localities. The ATP7A gene encodes
a protein that is responsible for transcellular copper
transport. A defect in such protein causes impaired copper absorption in the intestines and consequent copper
deficiency. This in turn results in reduced activity of
various copper-dependent enzymes throughout the body,
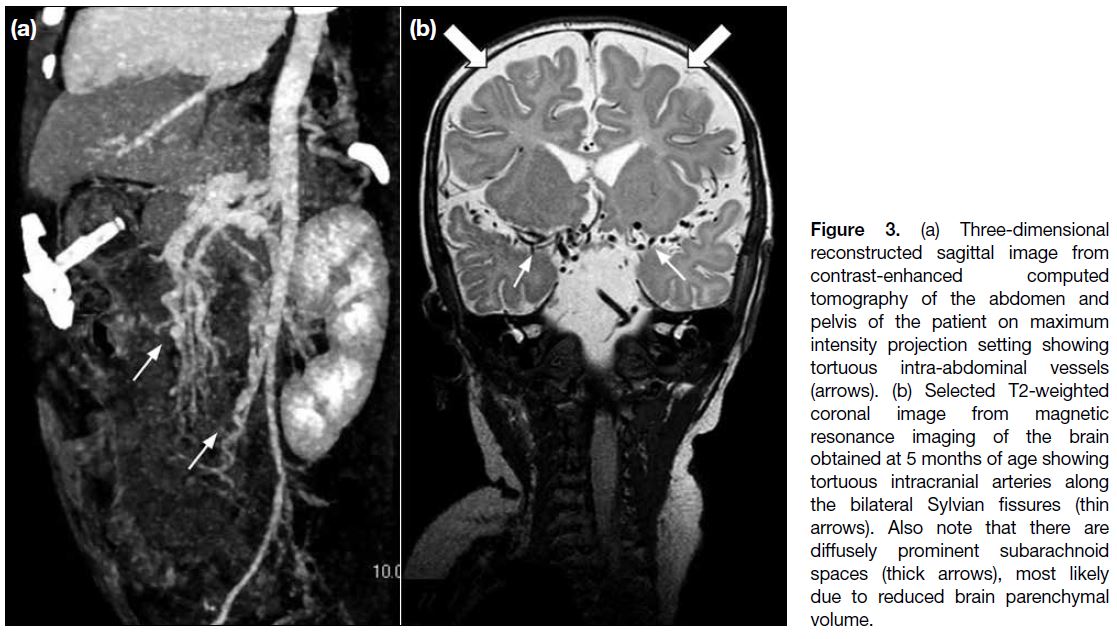
leading to neurodegeneration and defective connective
tissue synthesis, manifesting in the form of connective
tissue abnormalities such as frail hypopigmented hair
and vascular tortuosity (Figure 3).[1]
Figure 3. (a) Three-dimensional reconstructed sagittal image from contrast-enhanced computed tomography of the abdomen and pelvis of the patient on maximum intensity projection setting showing tortuous intra-abdominal vessels (arrows). (b) Selected T2-weighted coronal image from magnetic resonance imaging of the brain obtained at 5 months of age showing tortuous intracranial arteries along the bilateral Sylvian fissures (thin arrows). Also note that there are diffusely prominent subarachnoid spaces (thick arrows), most likely due to reduced brain parenchymal volume.
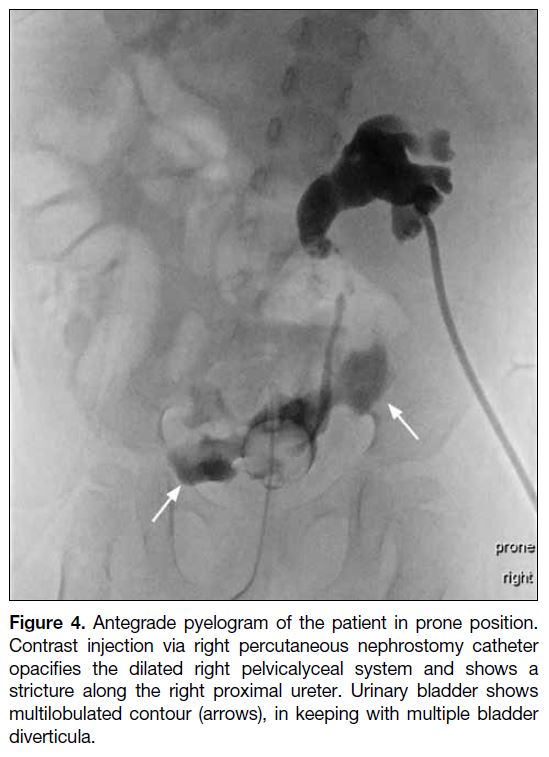
Urological abnormalities are also frequent in Menkes
disease. While the most common is urinary bladder
diverticula (Figure 4), others such as vesicoureteric
reflux, dilatation of the pelvicalyceal system and/or
ureters, and rupture of urinary bladder diverticula
have also been reported. These conditions may lead
to urinary stasis and can predispose patients to
recurrent urinary tract infections and urinary calculus
formation.[3]
Figure 4. Antegrade pyelogram of the patient in prone position.
Contrast injection via right percutaneous nephrostomy catheter
opacifies the dilated right pelvicalyceal system and shows a
stricture along the right proximal ureter. Urinary bladder shows
multilobulated contour (arrows), in keeping with multiple bladder
diverticula.
Rupture of the urinary collecting system is rare in
the paediatric population. It has been reported in
the presence of trauma[4] or due to obstruction of the
collecting system, for example by stone or congenital
anomaly (e.g., posterior urethral valve or ureteropelvic
junction obstruction).[5] [6] Conditions that cause soft
tissue abnormalities such as Klinefelter syndrome and
Cushing’s syndrome have been reported to be associated
with ureteric rupture and are thought to be predisposing
factors.[7] [8] We believe that Menkes disease was likely a
predisposing factor for renal pelvic rupture in our patient.
Clinically, it is difficult to differentiate renal pelvic rupture from other causes of abdominal pain and
tenderness; hence, the mainstay of diagnosis is imaging.
In the paediatric population, ultrasound is usually the first-line
imaging investigation to determine an underlying
cause of acute abdominal pain due to its lack of ionising
radiation. Nonetheless it is difficult to confirm the
diagnosis of renal pelvic rupture by ultrasound alone. In
cases with a high index of suspicion, contrast-enhanced
CT urography can help confirm the diagnosis, albeit at
the expense of ionising radiation.
In our patient, the most suspicious feature on ultrasound was the presence of perinephric and subphrenic fluid
collection. This warranted further imaging with contrast-enhanced
CT to delineate its extent and cause. As review
of subsequent CT images was suspicious of renal pelvic
rupture, delayed phase images were obtained. The
presence of contrast extravasation from the collecting
system confirmed the diagnosis.
Treatment should be individualised for each patient and
take account of the degree of sepsis, extent of urinoma
or abscess formation, and any suggestion of persistent
urinary leakage. Small urinomas can resorb over
time and may not require drainage. In cases of sizable
urinoma, image-guided drainage and urinary diversion
in the form of percutaneous nephrostomy or double-J
stent can be considered. Surgical repair of the defect may
be appropriate for ongoing urine leakage.
CONCLUSION
Rupture of the renal pelvis is an uncommon condition
and difficult to diagnose clinically, particularly in
children. Imaging with ultrasonography and contrast-enhanced
CT urography can aid diagnosis and facilitate
prompt management. Non-surgical treatment options
are commonly considered for drainage of urinoma and
urinary diversion, with surgical treatment reserved for
cases of persistent urinary leakage.
REFERENCES
1. Tümer Z, Møller LB. Menkes disease. Eur J Hum Genet. 2010;18:511-8. Crossref
2. Kaler SG, Ferreira CR, Yam LS. Estimated birth prevalence of Menkes disease and ATP7A-related disorders based on the Genome Aggregation Database (gnomAD). Mol Genet Metab Rep.
2020;24:100602. Crossref
3. Kim MY, Kim JH, Cho MH, Choi YH, Kim SH, Im YJ, et al. Urological problems in patients with Menkes disease. J Korean Med Sci. 2018;34:e4. Crossref
4. Mariotto A, Zampieri N, Cecchetto M, Camoglio FS. Ureteral rupture after blunt abdominal trauma in a child with unknown horseshoe kidney. Pediatr Med Chir. 2015;37:pmc.2015.110. Crossref
5. Taşkınlar H, Yiğit D, Avlan D, Naycı A. Unusual complication of a urinary stone in a child: spontaneous rupture of the renal pelvis with the migration of calculus into the retroperitoneum. Turk J Urol. 2016;42:48-50. Crossref
6. Heikkilä J, Taskinen S, Rintala R. Urinomas associated with posterior urethral valves. J Urol. 2008;180:1476-8. Crossref
7. Reva S, Tolkach Y. Spontaneous pelvic rupture as a result of renal colic in a patient with Klinefelter syndrome. Case Rep Urol. 2013;2013:374973. Crossref
8. Fuse H, Hara S, Ito H, Shimazaki J. Spontaneous rupture of the ureter of a patient with Cushing’s syndrome. Eur Urol. 1985;11:346-7. Crossref