Transradial Diagnostic Cerebral Angiography: Local Experience, Technique, and Outcomes
ORIGINAL ARTICLE
Hong Kong J Radiol 2023 Jun;26(2):111-9 | Epub 12 Jun 2023
Transradial Diagnostic Cerebral Angiography: Local Experience, Technique, and Outcomes
HT Lau, YLE Chu, R Lee, WP Cheng, KW Ho
Department of Radiology, Queen Mary Hospital, Hong Kong SAR, China
Correspondence: Dr YLE Chu, Department of Radiology, Queen Mary Hospital, Hong Kong SAR, China. Email: edchu.radiology@gmail.com
Submitted: 23 Oct 2021; Accepted: 4 Mar 2022.
Contributors: All authors designed the study, acquired and analysed the data. HTL and YLEC drafted the manuscript. All authors critically revised the manuscript for important intellectual content. All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of Interest: All authors have disclosed no conflicts of interest.
Funding/Support: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data Availability: All data generated or analysed during the present research are available from the corresponding author on reasonable request.
Ethics Approval: This research was approved by the Hong Kong West Cluster Research Ethics Committee of Hospital Authority, Hong Kong (Ref No.: HKWC-2021-0649/ UW 21-617). The Ethics Committee waived the need for patient consent for this retrospective study.
Abstract
Introduction
Transradial approach (TRA) has become a popular alternative to traditional transfemoral approach
for catheter cerebral angiography, as it offers advantages such as improved patient comfort, safety profile, and
cost-effectiveness. This study aimed to evaluate the efficacy and safety of ‘radial-first’ approach in diagnostic
neuroangiography in our locality.
Methods
We retrospectively analysed our database of consecutive catheter cerebral angiographies performed via TRA between September 2020 and July 2021. Patient demographics, procedural and radiographic metrics, radial access site–related complications, and total procedural time were recorded.
Results
A total of 52 TRA diagnostic cerebral angiographies were performed. Radial artery access was successfully obtained in all patients (n = 52). The rate of successful navigation through the brachial artery was 98.1% (n = 51), with an overall femoral crossover rate of 1.9% (n = 1). Satisfactory diagnostic images were obtained in all TRA cases (n = 51). Complications related to radial artery access were recorded in two cases (3.8%), including a case of transient radial arterial spasm and a case of transient radial artery occlusion. No access site–related permanent ischaemic symptoms were reported. Other severe access site complications such as pseudoaneurysm and arteriovenous fistula were not demonstrated.
Conclusion
TRA is a safe and feasible technique for diagnostic cerebral angiography in our locality, with a low complication rate.
Key Words: Angiography, digital subtraction; Cerebral angiography; Radial artery
中文摘要
經橈動脈診斷性腦血管造影:本地經驗、技術和結果
劉凱桃、朱賢麟、李雷釗、鄭永鵬、何家慧
引言
經橈動脈入路已成為傳統經股動脈導管腦血管造影術的流行替代方法,因其具有改善患者舒適度、安全性和成本效益等優勢。本研究旨在評估「優先採用經橈動脈入路」方法在我們本地診斷性神經血管造影術中的有效性和安全性。
方法
我們回顧性分析在2020年9月至2021年7月期間通過經橈動脈入路進行連續導管腦血管造影術的數據庫。我們記錄了患者的人口統計資料、手術和影像學指標、經橈動脈入路部位相關併發症和總手術時間。
結果
共進行了52次經橈動脈入路診斷性腦血管造影。所有患者(n = 52)經橈動脈入路插入均成功。通過肱動脈的成功導航率為98.1%(n = 51),一例後續採用了股動脈經路(1.9%)。所有經橈動脈入路病例(n = 51)都獲得了滿意的診斷圖像。兩例(3.8%)發生了與橈動脈通路相關的併發症,包括一例短暫性橈動脈痙攣和一例短暫性橈動脈閉塞。沒有與穿刺部位相關的永久性缺血症狀。未見其他通路部位嚴重併發症如假性動脈瘤和動靜脈等。
結論
經橈動脈入路是本地診斷性腦血管造影安全可行的技術,併發症發生率低。
INTRODUCTION
Catheter cerebral angiography is a common diagnostic
method to examine cerebral vasculature. Traditionally,
the procedures have been performed via the transfemoral
route. However, the transfemoral approach (TFA) is not
always feasible. For example, it will be problematic
in patients with dissection of the thoracic aorta,
iliofemoral occlusive disease, and inguinal infections.
TFA angiography also requires patients to tolerate
uncomfortable groin compression and bed rest after the
procedures. Serious access site–related complications,
including pseudoaneurysm, retroperitoneal haemorrhage,
femoral artery dissection, and lower limb ischaemia are
well recognised.[1] [2] [3] [4]
There has been a notable trend of transition from TFA to
the transradial approach (TRA) in cerebral angiography
among the neuroangiography community. This transition
was primarily fuelled by robust findings of TRA’s
lower access-related complications, lower mortality
rates, decreased length of hospital stay, and increased
patient satisfaction in the cardiology literature.[5] [6] Both
neuroangiography and interventional cardiology require
arterial catheterisation supplying the vital organs which
have narrow margin of error. Also, both of them first
started as TFA. Given these similarities between the
two fields, it was believed that the significant safety advantages of TRA for interventional cardiology might
be transferrable to neuroangiography. This has been
supported by recent data from the neuroangiographic
literature, which have demonstrated favourable safety
profiles, patient experiences, and cost-effectiveness of
TRA over TFA.[3] [7] [8] [9] [10] [11]
In light of the body of evidence demonstrating the clinical benefits of TRA, our centre has adopted a ‘radial-first’
approach in neuroangiography since September 2020.
Here we present our initial experience in the transition
from the traditional TFA to a ‘radial-first’ approach for
diagnostic cerebral angiography, including the technical
feasibility, safety, and complications of the TRA
technique.
METHODS
Study Design
We retrospectively analysed our institutional database of consecutive catheter cerebral angiographies performed
via TRA between September 2020 and July 2021.
Patient demographics, procedural and radiographic
metrics, radial access site–related complications, and
total procedural time were recorded.
Patient selection
All patients underwent preprocedural ultrasound assessment in order to measure the diameter of the right
radial artery and its patency. Patients with a radial artery
diameter of <1.6 mm were excluded and the TFA was
used instead. Patients requiring intervention in addition
to diagnostic angiography were also excluded.
Operators
Transradial cerebral angiographies were performed
by three operators during this time, including a
neuroradiology trainee who had no prior endovascular
experience and performed the procedure under the direct
supervision of one of the two other Hong Kong College
of Radiologists fellowship–qualified radiologists,
who had performed a minimum of 500 TFA cerebral
angiographies each.
Transradial Access Techniques
All TRAs used the right arm as the initial access site. The
radial artery was accessed at a point 1 to 2 cm proximal
to the wrist crease (standard TRA). The more distal
radial artery was accessed at the anatomical snuffbox
site (distal TRA) according to operator’s preference.
The patient was prepared and draped with the right arm
placed at the patient’s right side and the puncture location
exposed. For a standard TRA, the patient’s right distal
forearm and hand were placed in a slightly supinated
position of around 60°. Full supination of the hand can
often result in discomfort and is not necessary. For distal
TRA, the patient’s arm was allowed to rest in a neutral
position and hand supination was not required. A total of
1 to 2 mL of 1% lidocaine was infiltrated into the skin
around the puncture site. Under ultrasound guidance,
the radial artery was punctured using a 20-gauge
needle via Seldinger or modified Seldinger technique
according to the operator’s preference. A 5-F vascular
radial sheath introducer (Glidesheath Slender; Terumo,
Tokyo, Japan or Prelude Radial Sheath; Merit Medical
Systems, Inc, South Jordan [UT], US) was then placed
over an 0.025-inch hydrophilic guidewire (Glidewire
Hydrophilic Coated Guidewire; Terumo, Somerset [NJ],
US). A cocktail containing 3000 units of heparin and
2.0 mg of verapamil diluted with 20 mL of blood prior to
the infusion in order to avoid patient discomfort during
injection was infused over 1 minute through the side-port
of the sheath for antithrombotic and antispasmodic
purposes, respectively. Heparin was withheld in cases
where brain haemorrhage was a concern.
Catheter Navigation and Selection of the
Great Vessels
After TRA was obtained, a 5-F Simmons 2 catheter (S2) (Radifocus Optitorque; Terumo, Somerset [NJ], US) was
navigated over a 0.035-inch guidewire into the ipsilateral
subclavian artery. The navigation of the forearm and
brachium was performed under a monoplane setup with
radial roadmap guidance (Artis zee biplane; Siemens
Healthineers, Erlangen, Germany) in all of our cases,
with the bed at a 10-degree clockwise rotation along
patient’s coronal plane. The radial roadmap is obtained
in order to elucidate any radial artery anomalies and to
avoid lodging the guidewire into small arterial branches
during access to the subclavian. Loops that were
difficult to pass with a 0.035-inch wire were navigated
with a microcatheter system (Progreat Micro Catheter
System; Terumo, Somerset [NJ], US) which would often
straighten out the loop. Once the Simmons catheter was
brought into the subclavian artery, the table was returned
to its neutral position and the lateral plane was brought
into position at 90° to the anteroposterior plane (Artis
zee biplane).
In cases where imaging of the posterior fossa was of
interest, we preferred to first catheterise the right vertebral
artery, as this is often the great vessel encountered
coming in from the right subclavian artery, and its
catheterisation does not usually require reforming the S2
catheter. The catheter was then navigated to the arch to
access the other great vessels. We preferred to reform the
reverse curve of the Simmons catheter in the descending
aorta first whenever possible. In cases where the aorta
was too unfolded or too capacious to allow access to the
descending aorta with the guidewire, we reformed it off
the aortic valve.
Catheterisation and angiograms of the rest of the
great vessels was then performed with a formed S2
catheter. In cases where it was difficult to select the left
vertebral artery, depending on the operator’s preference,
catheterisation of the vessel with a S3 catheter was
attempted. Alternatively, subclavian injection with a
blood pressure cuff around the left arm was performed.
Haemostasis Technique
All arteriotomy closures were achieved with haemostatic
compression bands. In standard TRA, a radial wristband
(TR Band; Terumo, Somerset [NJ], US) was secured
to the arteriotomy site and inflated. The sheath was
then removed with the band inflated. The band was
then slowly deflated until a small amount of bleeding
occurred, after which we injected another 1 to 2 cc of air.
By using the minimum amount of compression needed
for haemostasis, we maximise the chances of preserved radial artery patency. A similar approach is used in the
closure of the distal TRA with a haemostasis device
(PreludeSYNC DISTAL; Merit Medical Systems, Inc,
South Jordan [UT], US).
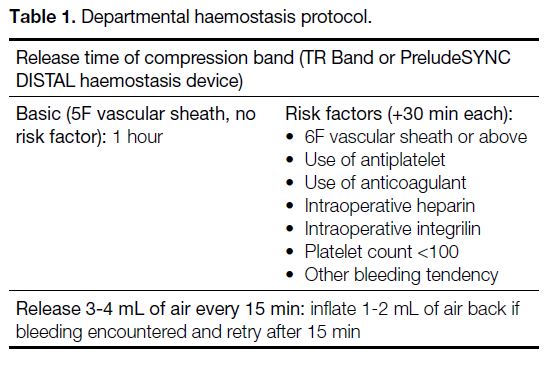
We followed a departmental protocol for releasing
the compression band in the postoperative unit (Table 1).
Table 1. Departmental haemostasis protocol.
RESULTS
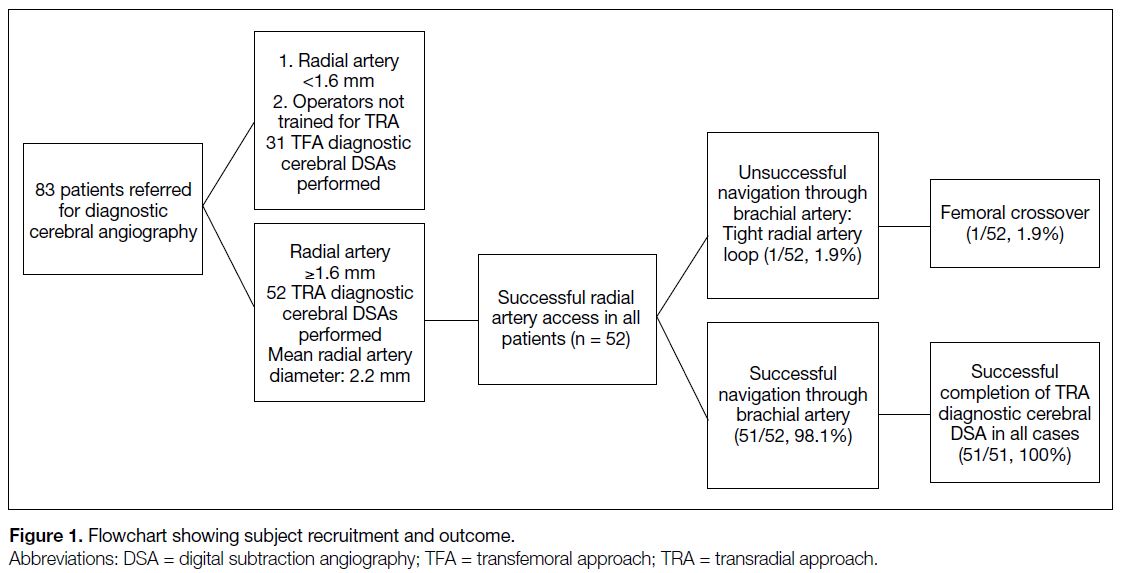
A total of 83 patients underwent diagnostic cerebral
angiography in our institution from September 2020
to July 2021. TRA was used as the primary access
technique in 52 patients (19 women and 33 men) with a
median age of 53 years, ranging from 20 to 81 years. The results are summarised in Figure 1.
Figure 1. Flowchart showing subject recruitment and outcome.
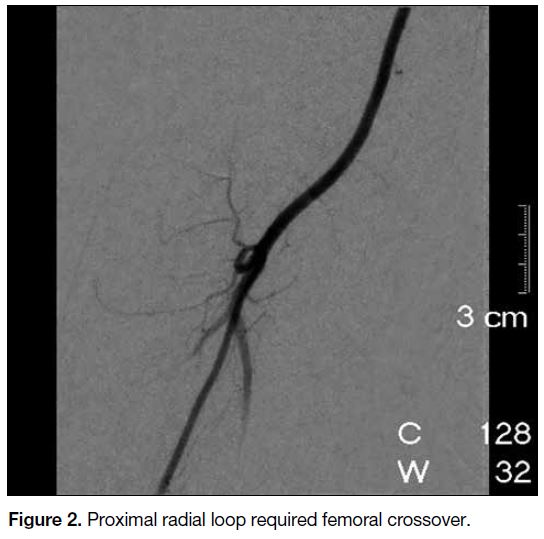
Radial artery access (including standard and distal TRA)
was successfully obtained in all 52 patients. Radial artery
anomalies, including a radial loop (Figure 2) and severe
radial artery tortuosity (Figure 3) were demonstrated
in two cases (3.8%). The rate of successful navigation
through the radial and subsequent brachial artery via TRA
was 98.1% (n = 51). A microcatheter-microwire system
(Progreat Micro Catheter System) was used in one of the
successful cases with severe radial tortuosity. In another
case, a tight loop was encountered in the proximal radial
artery (Figure 2) and the operator decided to crossover
to a TFA.
Figure 2. Proximal radial loop required femoral crossover.
Figure 3. Radial artery tortuosity required microcatheter-microwire system.
Satisfactory diagnostic images were obtained in cases
where catheters were successfully advanced past the
brachial artery (n = 51). None of these cases required
conversion to a TFA. The overall TFA crossover rate
was 1.9% (n = 1) in our cohort.
The mean diameter of the radial artery and distal radial
artery were 2.2 mm (range, 1.6-3.4) and 1.9 mm (range,
1-3), respectively. Distal TRA was attempted in 20
out of 52 cases. Access to the distal radial artery was
unsuccessful in two cases requiring crossover to a
standard TRA. Overall, standard TRA was performed
in 34 cases (65.4%) and distal TRA were performed
in 18 cases (34.6%). The mean diameter of the distal radial artery of successful distal TRAs was 2.2 mm, as
compared to 1.7 mm in the two unsuccessful cases. The
mean diameter of the radial artery in successful standard
TRAs was 2.2 mm.
The mean total procedural time was 45 minutes (range,
7-98), while the mean number of supra-aortic vessel
angiograms performed was 4.7. Choices of diagnostic
catheters for successful angiograms of different vessels
in our series are described in Table 2.
Table 2. Choice of diagnostic catheter used in successful angiograms.
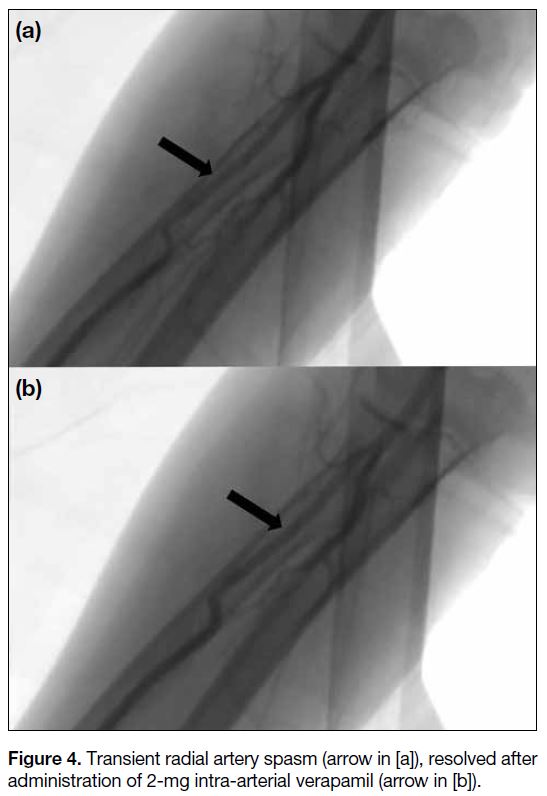
Complications related to radial artery access were
recorded in two cases (3.8%). This included a case
of transient radial arterial spasm (Figure 4) which
was managed with administration of 2-mg intra-arterial
verapamil. The angiogram was successfully
completed after the radial artery spasm was resolved.
No complications were encountered and the patient
was discharged on the day of the procedure. In the
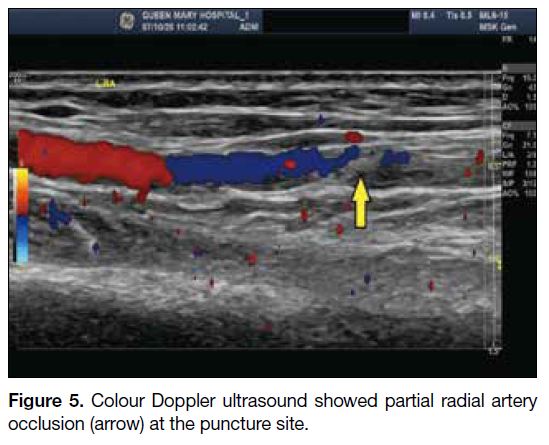
second case (distal TRA), the patient complained of
reduced muscle strength of his right hand and fingers,
which recovered spontaneously over a 2-week period.
Sonographic assessment at initial presentation showed
partial radial artery occlusion at the puncture site (Figure 5). This was spontaneously resolved together with the
symptoms 2 weeks after the procedure. No access site–related permanent ischaemic symptoms were reported.
Figure 4. Transient radial artery spasm (arrow in [a]), resolved after administration of 2-mg intra-arterial verapamil (arrow in [b]).
Figure 5. Colour Doppler ultrasound showed partial radial artery occlusion (arrow) at the puncture site.
Other severe procedure-related vascular complications
such as pseudoaneurysm, arteriovenous fistula, or
functional disability of the hand described in the
literature[4] [7] [8] were not demonstrated in our series.
In all, 38 patients underwent elective TRA diagnostic
cerebral angiography and 13 cases were performed on an
emergency basis. For elective cases, most of the patients
were discharged on the same day as the procedure
(n = 32, 84.2%), while five were discharged the
following day according to different departmental
practice. One patient, who underwent elective superficial
temporal artery to middle cerebral artery bypass surgery
for moyamoya disease on the same admission, was
discharged 3 days after the TRA procedure.
Overall, a success rate of 98.1% (n = 51) for transradial cerebral angiography was achieved. In the case where the
TRA was unsuccessful, the procedure was completed via
TFA, for an overall crossover rate to femoral approach of
1.9%. Cerebral angiograms were successfully obtained
in all cases when catheters were able to be advanced
beyond the brachial artery. The radial access site–related
complication rate was 3.8%.
DISCUSSION
Transradial Approach Benefits
All patients who underwent TRA cerebral angiography
in an outpatient setting were ambulatory immediately
after the procedure and most of them could be discharged
on the same day.
It is well-established that observation time after
TRA cerebral angiography is significantly shortened
as compared to TFA; this in turn reduces nursing
workload and hospital costs.[9] TRA is also associated
with significantly fewer access site complications.[11]
Uncomfortable groin compression and prolonged bed
rest can be avoided for TRA procedures.
Preprocedural Collateral Circulation
Assessment
We do not routinely perform preprocedural collateral
testing such as Barbeau or Allen tests in accordance with
recommendations from the American Heart Association,
as they have been proven to be unreliable in predicting
the incidence of hand ischaemia.[12] [13] [14]
Radial Cocktail
Nitroglycerine is one of the most common vasodilators
applied prophylactically to prevent radial artery
vasospasm.[3] [7] [10] [15] However, its use in patients with
potential neurovascular disease such as carotid stenosis
may lead to complications such as transient ischaemic
attack or even haemodynamic stroke due to an abrupt
fall in blood pressure.[16] [17] In our centre, we only included
2 mg of verapamil and 3000 units of heparin as a
standard radial cocktail to reduce the risk of vasospasm
during TRA. Overall, the rate of vasospasm, radial
access site complications, and femoral crossover were
all comparable to recent large-scale trials involving TRA
cerebral angiograms with prophylactic nitroglycerine.[3] [7] [10]
Radial Artery Anomaly and Technical
Challenges
Anomalous radial artery anatomy, including a radial
loop, high-bifurcating radial origin, arterial tortuosity,
atherosclerosis, and accessory branches, is relatively
common. A recent study of 1540 patients reported the
overall incidence of radial artery anomalies was 13.8%,
and procedural failure was far more common in patients
with anomalous anatomy than in patients with normal
anatomy.[18]
A radial roadmap was essential in identifying difficult
radial anatomy and therefore performed in all of our
cases. We encountered three cases of difficult radial
artery anatomy, including two cases of radial artery
anomalies (radial loop and severe radial tortuosity) and
a case of radial artery spasm despite pretreatment with
verapamil and heparin.
For the patient with severe radial tortuosity, a
microcatheter-microwire system (Progreat Micro
Catheter System) was used to overcome the tortuous
vessel. An additional 2-mg intra-arterial verapamil dose
was used in the case with radial artery spasm. Successful
TRA cerebral angiography was subsequently performed
in both cases.
One patient failed TRA due to the presence of a tight radial loop. In retrospect, it is possible that this could
have been resolved with the use of a microcatheter or
soft tip guidewire.
Choices of Diagnostic Catheter
The 5-F S2 catheter was our catheter of choice for
diagnostic cerebral angiography, similar to many other
centres worldwide.[7] [8] [19] First-pass success rate was 82.4%
(n = 42) of the cases. With the aid of a 5-F Glidecath
Hydrophilic Coated Catheter (Terumo, Somerset [NJ],
US) in S2 tip shape, 88.2% (n = 45) of cases were
completed. In our series, the right common carotid artery,
both internal carotid arteries, the right external carotid
artery, and both subclavian arteries were all successfully
cannulated by either a S2 or Glidecath (in S2 tip shape)
catheter.
The vertebral arteries are often different in diameter,
with the left side more frequently being dominant.[20] The
success rate of direct left vertebral artery catheterisation
from a right radial approach is known to be lower
compared to that of the rest of the great vessels.[19]
Specifically, the passage of a diagnostic catheter from
the aortic arch to the left vertebral artery through the
left subclavian artery could be difficult, and the success
rate depends on the angle of origin of the left vertebral
artery.[21] Successful left vertebral artery catheterisation is
less likely if the angle between the left vertebral artery
and left subclavian artery is <90°.[21]
In our series, 91.3% (21 out of 23) of left vertebral artery
angiograms were performed with a S2 or Glidecath (in S2
tip shape) catheter. The other two cases were performed
with S1 (Radifocus Optitorque; Terumo, Somerset [NJ],
US) and S3 (SIM3, Torcon NB Advantage Catheter;
Cook Medical, Bloomington [IN], US) catheters,
respectively. There was difficulty in forming the S2
curve in the descending arch in one patient, and the
operator therefore switched to a S1 catheter to cannulate
the left-sided supra-aortic vessels, including the left
vertebral artery. In another case, a S3 catheter was used
to perform a left vertebral artery angiogram as the S2
catheter failed to catheterise the vessel securely.
Haemostasis Protocol
All arteriotomy closures were achieved with a haemostatic compression band as mentioned (Table 1). None of our
patients experienced severe bleeding complications at
the radial artery access site, such as pseudoaneurysm or
significant haematoma.
Limitations
Our study had some limitations, including its
retrospective design and small sample size. Larger-scale
studies are needed to validate our initial findings.
CONCLUSION
TRA is a safe and feasible way for diagnostic cerebral
angiographies, with a low complication rate.
REFERENCES
1. Heiserman JE, Dean BL, Hodak JA, Flom RA, Bird CR, Drayer BP, et al. Neurologic complications of cerebral angiography. AJNR Am J Neuroradiol. 1994;15:1408-11.
2. Ricci MA, Trevisani GT, Pilcher DB. Vascular complications of cardiac catheterization. Am J Surg. 1994;167:375-8. Crossref
3. Wang Z, Xia J, Wang W, Xu G, Gu J, Wang Y, et al. Transradial versus transfemoral approach for cerebral angiography: a prospective comparison. J Interv Med. 2019;2:31-4. Crossref
4. Lee DH, Ahn JH, Jeong SS, Eo KS, Park MS. Routine transradial access for conventional cerebral angiography: a single operator’s experience of its feasibility and safety. Br J Radiol. 2004;77:831-8. Crossref
5. Bertrand OF, Bélisle P, Joyal D, Costerousse O, Rao SV, Jolly SS, et al. Comparison of transradial and femoral approaches for percutaneous coronary interventions: a systematic review and hierarchical Bayesian meta-analysis. Am Heart J. 2012;163:632-48. Crossref
6. Bertrand OF, Patel T. Radial approach for primary percutaneous coronary intervention: ready for prime time? J Am Coll Cardiol. 2012;60:2500-3. Crossref
7. Jo KW, Park SM, Kim SD, Kim SR, Baik MW, Kim YW. Is transradial cerebral angiography feasible and safe? A single center’s experience. J Korean Neurosurg Soc. 2010;47:332-7. Crossref
8. Matsumoto Y, Hongo K, Toriyama T, Nagashima H, Kobayashi S. Transradial approach for diagnostic selective cerebral angiography: results of a consecutive series of 166 cases. AJNR Am J Neuroradiol. 2001;22:704-8.
9. Romano DG, Frauenfelder G, Tartaglione S, Diana F, Saponiero R. Trans-radial approach: technical and clinical outcomes in neurovascular procedures. CVIR Endovasc. 2020;3:58. Crossref
10. Park JH, Kim DY, Kim JW, Park YS, Seung WB. Efficacy of transradial cerebral angiography in the elderly. J Korean Neurosurg Soc. 2013;53:213-7. Crossref
11. Tso MK, Rajah GB, Dossani RH, Meyer MJ, McPheeters MJ, Vakharia K, et al. Learning curves for transradial access versus transfemoral access in diagnostic cerebral angiography: a case
series. J Neurointerv Surg. 2022;14:174-8. Crossref
12. Mason PJ, Shah B, Tamis-Holland JE, Bittl JA, Cohen MG,
Safirstein J, et al. An update on radial artery access and best
practices for transradial coronary angiography and intervention in
acute coronary syndrome: a scientific statement from the American
Heart Association. Circ Cardiovasc Interv. 2018;11:e000035. Crossref
13. Bertrand OF, Carey PC, Gilchrist IC. Allen or no Allen: that is the question! J Am Coll Cardiol. 2014;63:1842-4. Crossref
14. Valgimigli M, Campo G, Penzo C, Tebaldi M, Biscagllia S, Ferrari R, et al. Transradial coronary catheterization and intervention across the whole spectrum of Allen test results. J Am
Coll Cardiol. 2014;63:1833-41. Crossref
15. da Silva RL, Luciano LS, Moreira DM, Fattah T, Trombetta AP, Panata L, et al. Randomised clinical trial comparing transradial catheterisation with or without prophylactic nitroglycerin. Br J Cardiol. 2017;24:100-4.
16. Ruff RL, Talman WT, Petito F. Transient ischemic attacks
associated with hypotension in hypertensive patients with carotid
artery stenosis. Stroke. 1981;12:353-5. Crossref
17. Belcaro G, Marchionno L. Hypotension as cause of TIAs (transient
ischemic attacks) in patients with severe carotid stenosis and
hypertension. Acta Chir Belg. 1983;83:436-8.
18. Lo TS, Nolan J, Fountzopoulos E, Behan M, Butler R,
Hetherington SL, et al. Radial artery anomaly and its influence on
transradial coronary procedural outcome. Heart. 2009;95:410-5. Crossref
19. Layton KF, Kallmes DF, Cloft HJ. The radial artery access site for interventional neuroradiology procedures. AJNR Am J Neuroradiol. 2006;27:1151-4.
20. Hong JM, Chung CS, Bang OY, Yong SW, Joo IS, Huh K. Vertebral artery dominance contributes to basilar artery curvature and peri-vertebrobasilar junctional infarcts. J Neurol Neurosurg Psychiatry. 2009;80:1087-92. Crossref
21. Luo N, Qi W, Tong W, Meng B, Feng W, Zhou X, et al. The effect of vascular morphology on selective left vertebral artery catheterization in right-sided radial artery cerebral angiography. Ann Vasc Surg. 2019;56:62-72. Crossref