Prevalence and Clinical Significance of Incidental Extracardiac Findings during Cardiac Magnetic Resonance Imaging: a Retrospective Study
ORIGINAL ARTICLE
Prevalence and Clinical Significance of Incidental Extracardiac Findings during Cardiac Magnetic Resonance Imaging: a Retrospective Study
HS Abdel Rahman1, AM Shawky2, EM Mehana3
1 Department of Radiology, Faculty of Medicine, Ain Shams University, Egypt
2 Department of Cardiology, Al-Azhar University, Egypt
3 Department of Radiology, Medical Research Institute, Alexandria University, Egypt
Correspondence: Dr EM Mehana, Department of Radiology, Medical Research Institute, Alexandria University, Egypt. Email: sayedmehana9@gmail.com
Submitted: 29 Jul 2021; Accepted: 5 Oct 2021.
Contributors: HSAR designed the study. All authors acquired and analysed the data. HSAR and EMM drafted the manuscript. All authors critically revised the manuscript for important intellectual content. All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of Interest: All authors have disclosed no conflicts of interest.
Funding/Support: This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data Availability: All data generated or analysed during the present study are available from the corresponding author on reasonable request.
Ethics Approval: This study was approved by the ethics committee of Saudi German Hospital, Jeddah, Saudi Arabia. The committee identified no ethical problem and granted a waiver on patient consent as this study was a retrospective description of clinical cases and no experiments or trials were done related to this study.
Abstract
Introduction
We sought to assess the prevalence and significance of incidental findings during cardiovascular magnetic resonance imaging (CMRI) and to investigate their impact on patient management.
Methods
We performed a retrospective evaluation of the CMRI images of all 131 referred patients suitable for
inclusion who presented to our radiology department between July 2017 and May 2019. Their images were evaluated
for any extracardiac findings beyond the pericardium detected and reported at the time of examination and classified
in terms of the effects of these findings on the patients’ treatment plans.
Results
A total of 109 incidental findings were detected in 53% of the scanned population, of which 27 (24.8%) were
clinically significant and potentially significant, including pulmonary consolidation (n = 11), extracardiac vascular
lesions (n = 3), and other chest and abdominal abnormalities. Among the 27 cases, four (all male; 3% of the study
population) showed clinically significant extracardiac findings, namely fibrocavitary tuberculosis, lymphoma, and
pericardial mesothelioma, as well as one case of patent ductus arteriosus, as patients were referred to other specialists
to treat the primary disease that was causative of the secondary cardiac problem.
Conclusions
Incidental extracardiac findings were common in CMRI, and although the prevalence of significant
lesions was low, they changed patient management. Thus, it is important to identify extracardiac findings and clarify
their significance during CMRI reporting.
Key Words: Cardiovascular system; Heart; Incidental findings; Magnetic resonance imaging
中文摘要
心臟磁共振成像時意外心臟外發現的發病率和臨床意義:回顧性研究
HS Abdel Rahman、AM Shawky、EM Mehana
簡介
我們評估心血管磁共振成像(CMRI)時偶然發現病變的普遍性和重要性,並調查它們對患者處理的影響。
方法
我們對2017年7月至2019年5月期間就診於我們放射科的所有131名適合納入的轉介患者的CMRI 圖像進行了回顧性評估,評估其圖像是否存在心包結構以外的任何心臟外發現,並根據這些發現對患者的治療計劃的影響進行分類。
結果
在53%的研究族群中共檢測到109項偶然發現,其中27項(24.8%)有臨床意義或具有潛在意義,包括肺實變(n = 11)、心外血管病變(n = 3)和其他胸部和腹部異常。患者總數中有四人(全部為男性;佔研究族群的3%)顯示有臨床意義的心外發現,即纖維腔結核、淋巴瘤和心包間皮瘤,以及一例動脈導管未閉。因為有導致繼發性心臟問題的原發性疾病,這些患者被轉介至其他專科醫生治療。
結論
意外的心外發現在CMRI中很常見,儘管顯著病變的發生率很低,但它們改變了患者的處理。因此,在CMRI報告中識別心外發現並闡明其意義非常重要。
INTRODUCTION
Cardiovascular magnetic resonance imaging (CMRI)
has proven to be one of the most established noninvasive
techniques to assess cardiac structure and performance
in multiple heart diseases, and hundreds of CMRI studies
have been performed subsequently.[1] During CMRI
acquisition, parts of the adjacent anatomical regions
within the thorax, upper abdomen, and root of the neck
are also imaged, especially in initial multi-section axial
and coronal images. These images can reveal a wide
range of pathologies outside the cardiovascular system.
Although many of these pathologies may represent
benign lesions of no clinical importance, others may
represent significant clues for new diagnoses, further
investigations, or early treatment.[2] [3]
The potential challenges and benefits associated
with these incidental extracardiac findings have been
investigated in multiple studies, the results of which
differed in terms of the prevalence of the findings and
their impact on the diagnosis and management plans
for patients.[1] [2] [3] [4] [5] [6] [7] [8] [9] [10] [11] [12] [13] [14] [15] [16] [17] However, these studies are in agreement
regarding the importance of incidental extracardiac
findings. Moreover, the importance of these extracardiac
findings has been recognised and implemented within
the European Association of Cardiovascular Imaging
core syllabus for the European Cardiovascular Magnetic
Resonance certification examination.[4] [5] [6] [7]
Extracardiac findings are also being increasingly
focused on while reporting CMRI findings at our centre.
Therefore, we performed this audit to retrospectively
evaluate the prevalence of incidental extracardiac
findings in clinically indicated CMRI examinations
performed at our institution and to assess their impact
on the patients’ diagnosis and management. Using the
obtained data, we hoped to provide recommendations for
changes to reporting of CMRI studies.
METHODS
Patient Population
In this study, we performed a retrospective evaluation of the CMRI images of all patients referred to the radiology
department at Saudi German Hospital, Jeddah, Saudi
Arabia between July 2017 and May 2019 for clinically
indicated CMRI to evaluate the prevalence of incidental
extracardiac findings in these cases. We excluded patients
with extended imaging, examinations with inadequate
image quality, and follow-up imaging assessments and
repeat scans. An incidental extracardiac finding was
defined as any change found beyond the pericardium,
e.g., great vessels, lung, pleural, or abdominal pathology.
Cardiovascular Magnetic Resonance Imaging Protocol
All CMRI examinations were performed on a 1.5T
Avanto MRI system (Siemens Healthcare, Germany) equipped with a 32-element cardiac coil array. All scans
were electrocardiography-gated for synchronisation
with the cardiac cycle and performed in end-expiration,
and were performed in accordance with a local standard
CMRI protocol that included the following sequences:
1. Three localising single-shot steady-state sequences in the three orthogonal planes, followed by axial, sagittal, and coronal multi-section half-Fourier acquisition single-shot turbo spin-echo (HASTE). These sequences were acquired from the top of the aortic arch to the diaphragm in the axial plane, from the sternum to the spine in the coronal plane, and from the right to left cardiac borders in the sagittal plane. The field of view (FOV) chosen was based on patient size and ranged from 340 × 233 mm2 to 390 × 344 mm2. Base and phase resolutions were 256 and 59%, respectively. Section thickness and section gap were 8 and 2 mm, respectively, yielding spatial resolutions from 2.3 mm × 1.3 mm × 8 mm to 2.5 mm × 1.5 mm × 8 mm.
2. Cine sequences with steady-state free precession (SSFP)–oriented 2-chamber vertical long-axis view, 4-chamber horizontal long-axis view, 3-chamber view, and short axis for studying the kinetics of the right and left ventricles (acquisition time, 7-12 s for each section; matrix, 192 × 192; flip angle, 180°; echo time, 1.69 ms).
3. Phase-contrast sequence to review valvular flow. This sequence was planned using a 3-chamber view and coronal aortic view, with one section perpendicular to the ascending aorta just distal to the valve leaflet tips, velocity encoding = 150 cm/s for normal flow (or greater for stenosis), retrospective gating, and short echo time for optimal flow sensitivity.
4. Phase-sensitive inversion recovery (PSIR) sequences for studying late gadolinium enhancement performed 10 to 15 minutes after intravenous administration of gadolinium (0.1-0.2 mmol/kg). FOV, 244 × 300 mm2; matrix, 156 × 256.
1. Three localising single-shot steady-state sequences in the three orthogonal planes, followed by axial, sagittal, and coronal multi-section half-Fourier acquisition single-shot turbo spin-echo (HASTE). These sequences were acquired from the top of the aortic arch to the diaphragm in the axial plane, from the sternum to the spine in the coronal plane, and from the right to left cardiac borders in the sagittal plane. The field of view (FOV) chosen was based on patient size and ranged from 340 × 233 mm2 to 390 × 344 mm2. Base and phase resolutions were 256 and 59%, respectively. Section thickness and section gap were 8 and 2 mm, respectively, yielding spatial resolutions from 2.3 mm × 1.3 mm × 8 mm to 2.5 mm × 1.5 mm × 8 mm.
2. Cine sequences with steady-state free precession (SSFP)–oriented 2-chamber vertical long-axis view, 4-chamber horizontal long-axis view, 3-chamber view, and short axis for studying the kinetics of the right and left ventricles (acquisition time, 7-12 s for each section; matrix, 192 × 192; flip angle, 180°; echo time, 1.69 ms).
3. Phase-contrast sequence to review valvular flow. This sequence was planned using a 3-chamber view and coronal aortic view, with one section perpendicular to the ascending aorta just distal to the valve leaflet tips, velocity encoding = 150 cm/s for normal flow (or greater for stenosis), retrospective gating, and short echo time for optimal flow sensitivity.
4. Phase-sensitive inversion recovery (PSIR) sequences for studying late gadolinium enhancement performed 10 to 15 minutes after intravenous administration of gadolinium (0.1-0.2 mmol/kg). FOV, 244 × 300 mm2; matrix, 156 × 256.
Data Interpretation
Two radiologists with at least 5 years of experience in
reporting and supervising cardiovascular MR imaging
and without prior knowledge of the objectives of
the study reinterpreted the CMRI examinations. All
extracardiac findings were recorded as incidental
findings and formed the basis for diagnosis. To assess
the clinical implications of the incidental extracardiac
findings, clinical data were analysed by reviewing the
electronic medical records database of the hospital. All
those findings were characterised and classified into three categories: (1) non-significant, which are findings that
did not warrant further action; (2) potentially significant,
which are findings with possible clinical significance
that warranted further imaging or specialist consultation
but did not warrant a change of the treatment plan or
primary diagnosis; and (3) significant, which are findings
with major clinical significance that warranted a change
in the patient’s treatment plan and primary diagnosis.
The prevalence of incidental extracardiac findings and
their sites were evaluated and reported. Evaluation of
the previous radiological reports for the patients was
also performed to assure that significant and potentially
significant findings had not been missed and qualified for
a change of the treatment plan of the patients, if any.
RESULTS
A total of 140 patients underwent CMRI examinations
during the study period; of these, we included 131 patients
after excluding nine patients for the following reasons:
extended imaging (e.g., cardiac MR and abdominal MR
in one session; 2 patients), examinations with inadequate
image quality (e.g., artifacts, arrhythmia, or incomplete
examination because of patient-related factors; 4
patients), and follow-up imaging assessments and repeat
scans (3 patients). The patients’ ages ranged from 1 to
84 years (mean, 44). The study population included 14
children (one aged 1 year and 13 adolescents aged 10-19
years). The 131 patients included 104 males (79%) and
27 females (21%).
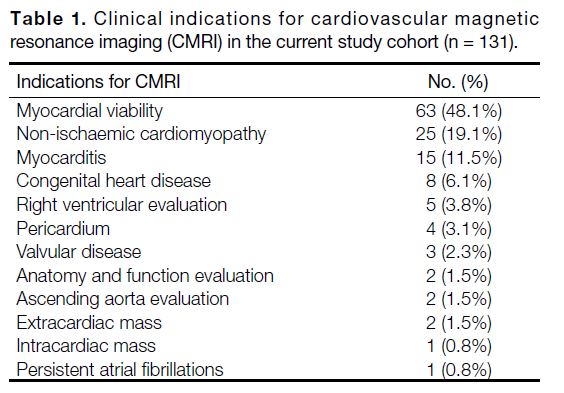
An analysis of the clinical indications for our study cohort is presented in Table 1. Most of our patients were referred
for evaluation of myocardial viability (63 patients,
48.1%), followed by non-ischaemic cardiomyopathy
(25 patients, 19.1%) and myocarditis (15 patients,
11.5%); other indications included congenital heart disease, right ventricular evaluation, valvular disease,
and intra- or extracardiac masses.
Table 1. Clinical indications for cardiovascular magnetic resonance imaging (CMRI) in the current study cohort (n = 131).
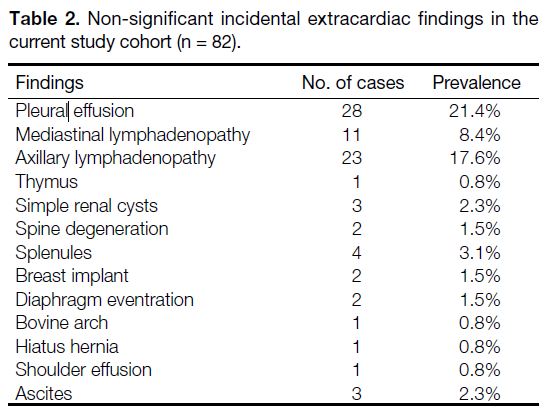
A total of 109 incidental extracardiac findings were
recorded in 70 patients (53.4% of the study population),
while 61 patients (46.6%) did not show any extracardiac
findings. Of these findings, 82 (75.2% of the findings)
were mild or of no clinical significance (Table 2) and
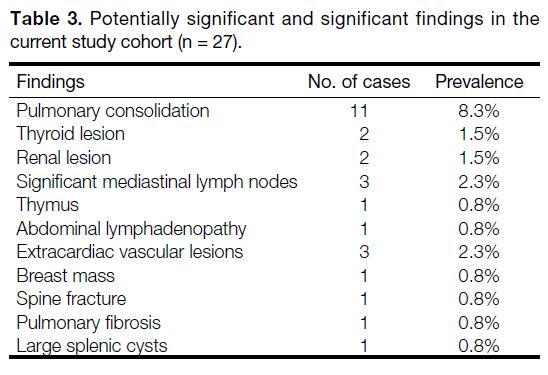
27 (24.8% of the findings) warranted further diagnostic
workup or consultation since they were considered
significant or potentially significant (Table 3).
Table 2. Non-significant incidental extracardiac findings in the current study cohort (n = 82).
Table 3. Potentially significant and significant findings in the current study cohort (n = 27).
Out of the 109 incidental extracardiac findings, four
findings in four patients had a clinically significant
impact on patient diagnosis and management (prevalence
among incidental extracardiac findings, 3.7%) but were
not clinically significant before imaging. These were as
follows:
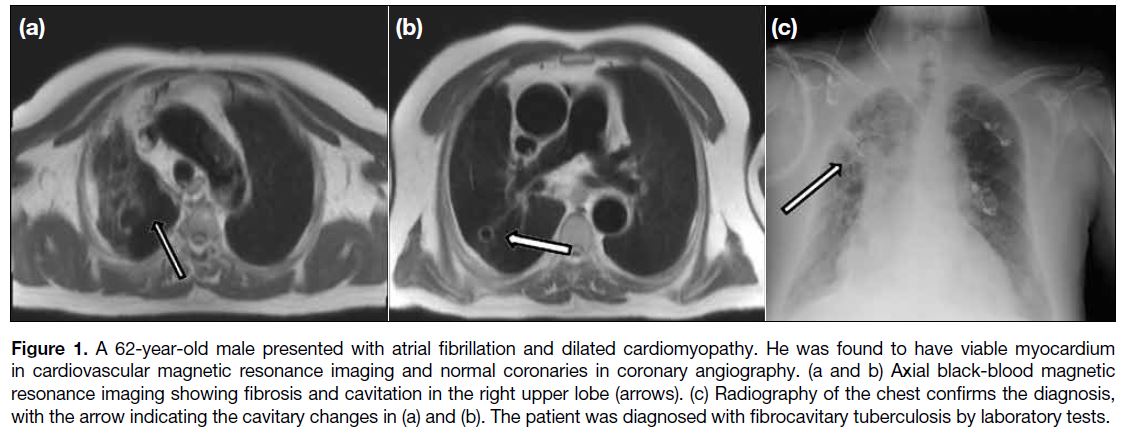
1. Right upper lobe consolidation and cavitation (fibrocavitary tuberculosis) in a patient presenting with dilated cardiomyopathy. This was confirmed by radiography and laboratory tests (Figure 1). The patient was referred to a pulmonologist, and the cardiac problem was treated as secondary, not primary, dilated cardiomyopathy as the dilation of the cardiac chamber was secondary to the inflammatory process caused by tuberculosis which may be reversable after treating the cause.
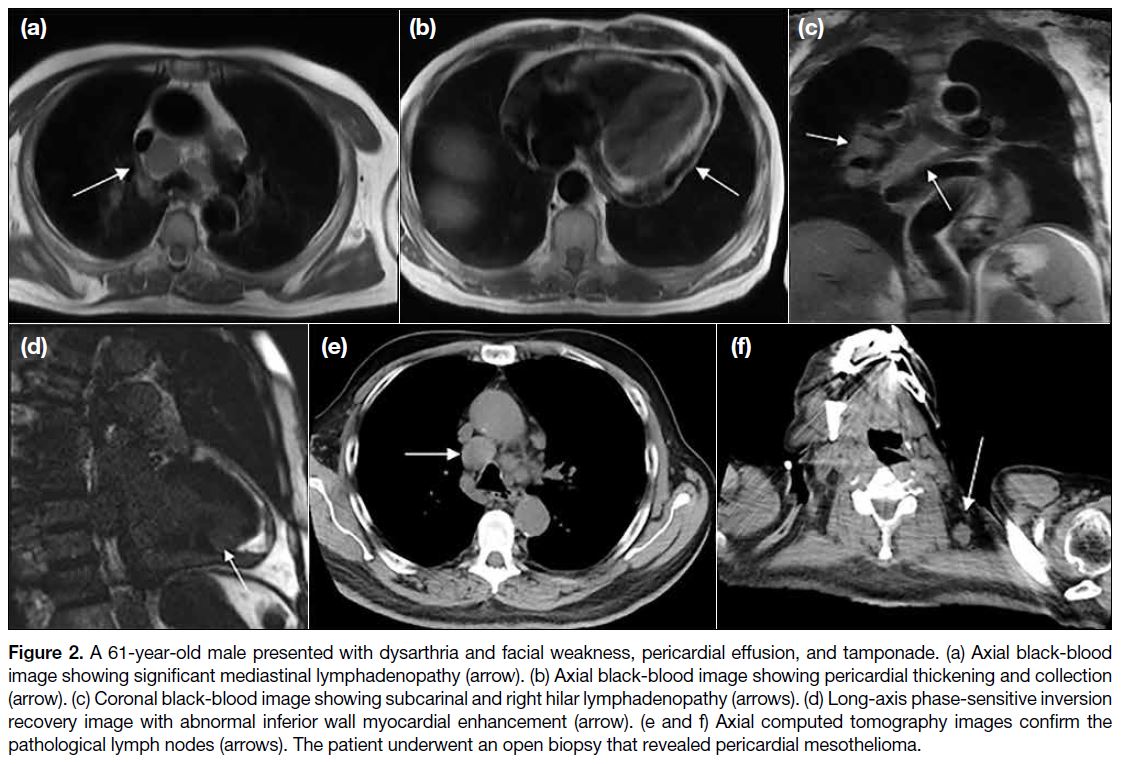
2. Marked mediastinal lymph node enlargement, moderate pericardial effusion, and enhancement (pericardial mesothelioma) in a patient with persistent haemorrhagic pericardial effusion. This was diagnosed by an open biopsy in cardiopulmonary surgery (Figure 2). The patient was subsequently referred to an oncologist to receive treatment for the condition in conjunction with the cardiology management.
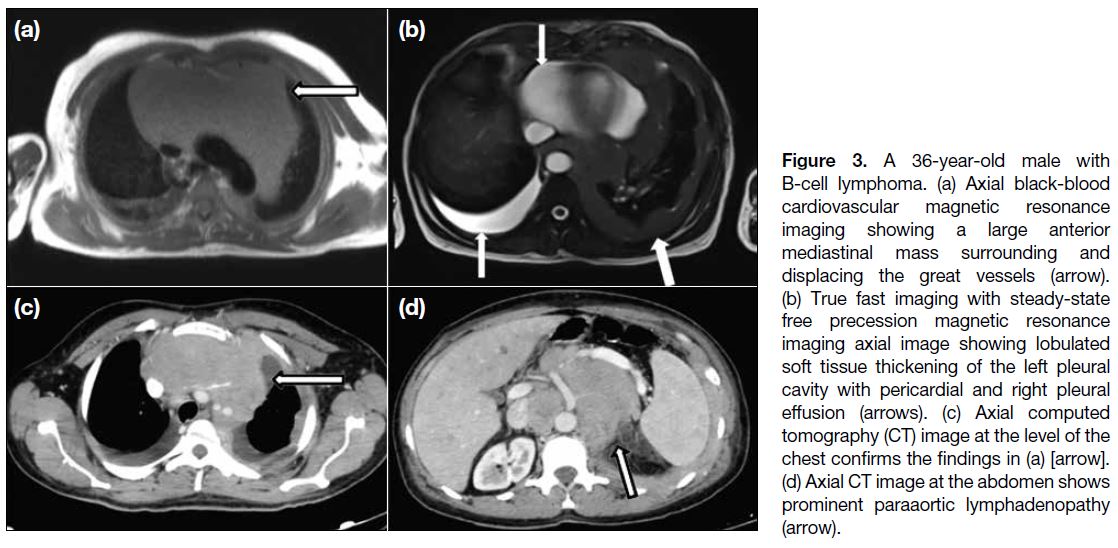
3. Multiple left lung patchy consolidations, enlarged left supraclavicular lymph node, and marked abdominal paraaortic lymphadenopathy (B-cell lymphoma) in a patient with a large anterior mediastinal mass. This was confirmed by biopsy (Figure 3) and the patient was referred to an oncologist for treatment of the primary condition.
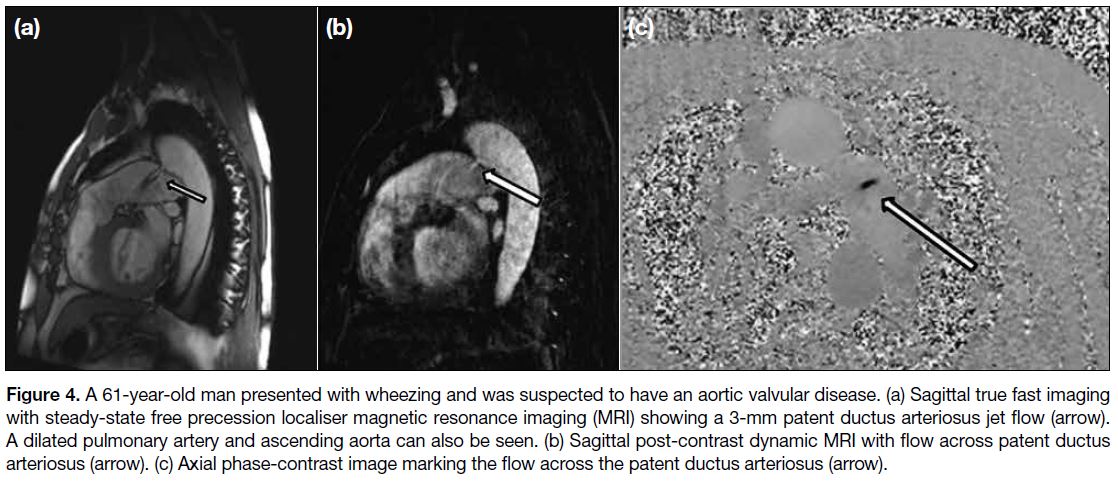
4. Patent ductus arteriosus in an adult patient with dilated right ventricle and pulmonary artery and suspected pulmonary hypertension. The pulmonary-to-systemic blood flow ratio was 0.6:1, while the estimated shunted blood volume through the patent ductus arteriosus was 111 mL. He was referred to undergo cardiothoracic surgery for adequate management (Figure 4).
1. Right upper lobe consolidation and cavitation (fibrocavitary tuberculosis) in a patient presenting with dilated cardiomyopathy. This was confirmed by radiography and laboratory tests (Figure 1). The patient was referred to a pulmonologist, and the cardiac problem was treated as secondary, not primary, dilated cardiomyopathy as the dilation of the cardiac chamber was secondary to the inflammatory process caused by tuberculosis which may be reversable after treating the cause.
2. Marked mediastinal lymph node enlargement, moderate pericardial effusion, and enhancement (pericardial mesothelioma) in a patient with persistent haemorrhagic pericardial effusion. This was diagnosed by an open biopsy in cardiopulmonary surgery (Figure 2). The patient was subsequently referred to an oncologist to receive treatment for the condition in conjunction with the cardiology management.
3. Multiple left lung patchy consolidations, enlarged left supraclavicular lymph node, and marked abdominal paraaortic lymphadenopathy (B-cell lymphoma) in a patient with a large anterior mediastinal mass. This was confirmed by biopsy (Figure 3) and the patient was referred to an oncologist for treatment of the primary condition.
4. Patent ductus arteriosus in an adult patient with dilated right ventricle and pulmonary artery and suspected pulmonary hypertension. The pulmonary-to-systemic blood flow ratio was 0.6:1, while the estimated shunted blood volume through the patent ductus arteriosus was 111 mL. He was referred to undergo cardiothoracic surgery for adequate management (Figure 4).
Figure 1. A 62-year-old male presented with atrial fibrillation and dilated cardiomyopathy. He was found to have viable myocardium
in cardiovascular magnetic resonance imaging and normal coronaries in coronary angiography. (a and b) Axial black-blood magnetic
resonance imaging showing fibrosis and cavitation in the right upper lobe (arrows). (c) Radiography of the chest confirms the diagnosis,
with the arrow indicating the cavitary changes in (a) and (b). The patient was diagnosed with fibrocavitary tuberculosis by laboratory tests.
Figure 2. A 61-year-old male presented with dysarthria and facial weakness, pericardial effusion, and tamponade. (a) Axial black-blood
image showing significant mediastinal lymphadenopathy (arrow). (b) Axial black-blood image showing pericardial thickening and collection
(arrow). (c) Coronal black-blood image showing subcarinal and right hilar lymphadenopathy (arrows). (d) Long-axis phase-sensitive inversion
recovery image with abnormal inferior wall myocardial enhancement (arrow). (e and f) Axial computed tomography images confirm the
pathological lymph nodes (arrows). The patient underwent an open biopsy that revealed pericardial mesothelioma.
Figure 3. A 36-year-old male with B-cell lymphoma. (a) Axial black-blood cardiovascular magnetic resonance imaging showing a large anterior mediastinal mass surrounding and displacing the great vessels (arrow). (b) True fast imaging with steady-state free precession magnetic resonance imaging axial image showing lobulated soft tissue thickening of the left pleural cavity with pericardial and right pleural effusion (arrows). (c) Axial computed tomography (CT) image at the level of the chest confirms the findings in (a) [arrow]. (d) Axial CT image at the abdomen shows prominent paraaortic lymphadenopathy (arrow).
Figure 4. A 61-year-old man presented with wheezing and was suspected to have an aortic valvular disease. (a) Sagittal true fast imaging
with steady-state free precession localiser magnetic resonance imaging (MRI) showing a 3-mm patent ductus arteriosus jet flow (arrow).
A dilated pulmonary artery and ascending aorta can also be seen. (b) Sagittal post-contrast dynamic MRI with flow across patent ductus
arteriosus (arrow). (c) Axial phase-contrast image marking the flow across the patent ductus arteriosus (arrow).
Among the anatomical sites where incidental
extracardiac findings were detected, the chest showed
the highest prevalence of findings among the whole
patient population, including pleural effusion (n = 28,
21.4%), axillary lymphadenopathy (n = 23, 17.6%) or
mediastinal lymphadenopathy (n = 14, 10.7%), followed
by pulmonary parenchymal lesions (n = 12, 9.2%),
thymus (n = 2, 1.5%), breast lesions (n = 3, 2.3%), spine
abnormalities (n = 3, 2.3%), vascular extracardiac lesions
(n = 4, 3.1%), and a shoulder effusion (n = 1, 0.8%).
In contrast, abdominal findings were less prevalent and
included ascites (n = 3, 2.3%), diaphragmatic hiatal
hernia (n = 1, 0.8%), splenic lesions (n = 5, 3.8%), renal
lesions (n = 5, 3.8%), abdominal lymphadenopathy (n = 1, 0.8%), and diaphragmatic eventration (n = 2, 1.5%).
The site showing the lowest prevalence of findings
was the root of the neck with only two thyroid nodules
reported (1.5%).
The most relevant sequences that detected extracardiac
findings were the initial localiser sequences (HASTE)
within the three orthogonal planes that allowed a global
view, with all incidental extracardiac findings visualised
in this sequence. Other relevant sequences were the
morphological post-contrast PSIR sequences in which 10 out of 109 of the findings were visualised, and cine-SSFP sequences in which five findings were visualised.
DISCUSSION
CMRI is a highly reproducible tool to assess
cardiovascular diseases. In CMRI examinations, an informed assessment of extracardiac structures can help
detect multiple non-cardiac diseases. However, few
studies in the literature have reported the prevalence
and nature of incidental extracardiac findings on CMRI;
although the comparisons of these studies are difficult
because of different study designs (i.e., the study cohorts,
clinical setting, sequences applied, and reading session
format), the general agreement is that missing these
incidental extracardiac findings can result in a significant
delay in the appropriate management of the patients,
which may be associated with progressive morbidity, as
well as legal consequences and costs.[3] [8] [9]
For the classification of incidental extracardiac findings,
we adopted the scheme proposed by Gravina et al,[3]
who divided incidental extracardiac findings into three
groups: (1) findings with mild or no clinical significance;
(2) findings with possible clinical significance; and
(3) clinically significant findings that required further
diagnostic workup or the initiation of a new specific
treatment different from the current treatment or ended
by a non-cardiac diagnosis of the disease process of
the patient. However, some other studies categorised
incidental extracardiac findings as relevant if they
required further diagnostic workup or the initiation of a new specific treatment different from the current
treatment or clinically irrelevant/insignificant if they
necessitated no change in the patient’s management.[1] [9] [10] [11]
Previous studies have also differed in their considerations
for relevant findings. For example, Jacobs et al[12]
considered pleural effusion as a potentially relevant
finding, whereas other studies[10] [13] [14] performed a separate
assessment in each case to classify the significance of
the findings. In our study, we also assessed the patients
individually and found that pleural effusion in all the
patients was non-significant and was related to their
cardiac condition since a large group of our patients had
ischaemic heart disease.
Our study is consistent with other studies with regard to the significant lesions. However, the difference between
our study and those of other studies was rooted in the
non-significant lesions, which did not influence patient
management. In our retrospective cross-sectional study
with a focused review of 131 CMRI examinations (based
on an image review), extracardiac abnormal findings
were prevalent in 53% of the study population. Similar
studies reported the rates of extracardiac abnormal
findings from 10 to 62%.[7] [8] [15] This great variability may
be attributed to differences in study designs, the use of
different definitions of incidental extracardiac findings,
as well as the differences in the number of patients
included within the studies. In this study, we found that
3.7% of incidental extracardiac findings were clinically
significant, which was comparable to other studies with
reported rates of 2 to 5%.[3] [10] However, a much lower
prevalence of 0.9% was reported.[7] This variation could
be attributed to the larger patient population included
in their study, the differences in the study protocols,
variations in the FOV coverage, and, possibly, the
differences in the number of sections per sequence.[9]
In our evaluation of the site of prevalence of extracardiac findings either in the lower neck, chest, or upper
abdomen, we found that most were localised in the chest,
such as pleural effusion; this may be because most of
our patients were referred for ischaemic cardiomyopathy
(48.1%). Sokolowski et al[7] also reported a high association between vascular and congenital heart
disease indications and a high prevalence of vascular
findings and a low prevalence of major findings. Despite
a male predominance in our study compared with
other reports,[1] [3] the overall prevalence of incidental
extracardiac findings was higher in female patients
(77.8% vs. 47.1%).
With regard to the influence of MRI sequences on
detection of incidental extracardiac findings, we found
that while the lesions could be detected in multiple
sequences, 100% of such findings were identified in
the HASTE sequence due to its large FOV and tissue
coverage, despite the lower spatial resolution, while the
single-section cine-SSFP and multi-section post-contrast
PSIR sequences were useful in confirming some of these
findings or limiting the differential diagnosis on the basis
of signal intensity and enhancement characteristics.
This is in agreement with other reports[3] [16] but with the
difference that they used multiplane SSFP localisers
instead of HASTE. Another study[17] compared these two large-FOV sequences and stated that the transaxial
balanced SSFP (bSSFP) sequence with a wide FOV is
more accurate in the detection of incidental extracardiac
findings than the HASTE localiser images due to its better
spatial resolution. In our study, we depended on HASTE
localiser images for evaluation of incidental extracardiac
findings since all of these were detected in these large-FOV images, with confirmation or clarification of some
of the findings in other sequences such as late post-contrast
images, as a result of the poorer resolution of HASTE localiser images.
One limitation of our study and a potential source of
bias is its small size, which hindered evaluation of
the incidental extracardiac finding prevalence by age-group.
Another limitation was the absence of histologic
confirmation since many lesions were managed on the
basis of suspected imaging diagnoses alone. We should
also mention that our routine localised large-FOV
sequence was the HASTE sequence, and we would have
preferred to compare these findings to those obtained
with the large-FOV bSSFP sequence, which has a higher
spatial resolution and provides greater coverage in a very
short time.
We recommend adding a subtitle to CMRI reports
to include the extracardiac findings encountered
during reporting and their significance or the further
recommended management. We also recommend the
use of bSSFP sequences with a wide FOV during routine
CMRI in the axial and coronal planes to replace the
HASTE localising sequences at the beginning of the
CMRI study owing to their better resolution.
CONCLUSION
Incidental extracardiac findings are common in cardiac
MRI, and, despite the low prevalence of significant lesions (around 3% of patients), they changed patient
management and facilitated the delivery of an accurate
diagnosis. Hence, it is important to identify incidental
extracardiac findings and clarify their significance during
CMRI reporting.
REFERENCES
1. Ulyte A, Valeviciene N, Palionis D, Kundrotaite S, Tamosiunas A.
Prevalence and clinical significance of extracardiac findings
in cardiovascular magnetic resonance. Hellenic J Cardiol.
2016;57:256-60. Crossref
2. Rodrigues JC, Lyen SM, Loughborough W, Amadu AM, Baritussio A, Dastidar AG, et al. Extra-cardiac findings in
cardiovascular magnetic resonance: what the imaging cardiologist
needs to know. J Cardiovasc Magn Reson. 2016;18:26. Crossref
3. Gravina M, Stoppino LP, Casavecchia G, Moffa AP, Vinci R,
Brunetti ND, et al. Incidental extracardiac findings and
their characterization on cardiac MRI. Biomed Res Int.
2017;2017:2423546. Crossref
4. Dunet V, Barras H, Boulanger X, Monney P, Qanadli SD, Meuli R, et al. Impact of extracardiac findings during cardiac MR on patient management and outcome. Med Sci Monit. 2015;21:1288-96. Crossref
5. Dunet V, Schwitter J, Meuli R, Beigelman-Aubry C. Incidental
extracardiac findings on cardiac MR: systematic review and metaanalysis.
J Magn Reson Imaging. 2016;43:929-39. Crossref
6. Petersen SE, Almeida AG, Alpendurada F, Boubertakh R,
Bucciarelli-Ducci C, Cosyns B, et al. Update of the European
Association of Cardiovascular Imaging (EACVI) core syllabus for
the European Cardiovascular Magnetic Resonance Certification
Exam. Eur Heart J Cardiovasc Imaging. 2014;15:728-9. Crossref
7. Sokolowski FC, Karius P, Rodríguez A, Lembcke A, Wagner M,
Hamm B, et al. Extracardiac findings at cardiac MR imaging: a single-centre retrospective study over 14 years. Eur Radiol. 2018;28:4102-10 Crossref
8. Wyttenbach R, Médioni N, Santini P, Vock P, Szucs-Farkas Z.
Extracardiac findings detected by cardiac magnetic resonance
imaging. Eur Radiol. 2012;22:1295-302. Crossref
9. Mora-Encinas JP, Martín-Martín B, Nogales-Montero J, Mora-Monago R, Romero JA. Prevalence and significance of extracardiac
findings in cardiac magnetic resonance imaging. Rev Argent Radiol.
2016;80:171-7. Crossref
10. Atalay MK, Prince EA, Pearson CA, Chang KJ. The prevalence and clinical significance of noncardiac findings on cardiac MRI. AJR Am J Roentgenol. 2011;196:W387-93. Crossref
11. McKenna DA, Laxpati M, Colletti PM. The prevalence of incidental findings at cardiac MRI. Open Cardiovasc Med J. 2008;2:20-5. Crossref
12. Jacobs PC, Mali WP, Grobbee DE, van der Graaf Y. Prevalence of incidental findings in computed tomographic screening of the chest: a systematic review. J Comput Assist Tomogr. 2008;32:214-21. Crossref
13. Sohns JM, Schwarz A, Menke J, Staab W, Spiro JE, Lotz J, et al. Prevalence and clinical relevance of extracardiac findings at cardiac MRI. J Magn Reson Imaging. 2014;39:68-76. Crossref
14. Irwin RB, Newton T, Peebles C, Borg A, Clark D, Miller C, et al. Incidental extra-cardiac findings on clinical CMR. Eur Heart J Cardiovasc Imaging. 2013;14:158-66. Crossref
15. Chan PG, Smith MP, Hauser TH, Yeon SB, Appelbaum E, Rofsky NM, et al. Noncardiac pathology on clinical cardiac
magnetic resonance imaging. JACC Cardiovasc Imaging.
2009;2:980-6. Crossref
16. Khosa F, Romney BP, Costa DN, Rofsky NM, Manning WJ. Prevalence of noncardiac findings on clinical cardiovascular MRI. AJR Am J Roentgenol. 2011;196:W380-6. Crossref
17. Mantini C, Mastrodicasa D, Bianco F, Bucciarelli V, Scarano M, Mannetta G, et al. Prevalence and clinical relevance of extracardiac findings in cardiovascular magnetic resonance imaging. J Thorac Imaging. 2019;34:48-55. Crossref