Iatrogenic Injury to the Iliolumbar Artery during Bone Marrow Biopsy Successfully Treated with Direct Embolisation through the Biopsy Needle: a Case Report
CASE REPORT
Iatrogenic Injury to the Iliolumbar Artery during Bone Marrow Biopsy Successfully Treated with Direct Embolisation through the Biopsy Needle: a Case Report
EYL Chu, B Fang
Department of Radiology, Queen Mary Hospital, Hong Kong
Correspondence: Dr EYL Chu, Department of Radiology, Queen Mary Hospital, Hong Kong. Email: edchu.radiology@gmail.com
Submitted: 31 May 2021; Accepted: 12 Aug 2021.
Contributors: Both authors designed the study, acquired the data, analysed the data, drafted the manuscript, and critically revised the manuscript for important intellectual content. Both authors had full access to the data, contributed to the study, approved the final version for publication, and
take responsibility for its accuracy and integrity.
Conflicts of Interest: All authors have disclosed no conflicts of interest.
Funding/Support: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data Availability: All data generated or analysed during the present study are available from the corresponding author on reasonable request.
Ethics Approval: The patient was treated in accordance with the tenets of the Declaration of Helsinki. The patient provided written informed
consent for the study.
INTRODUCTION
Bone marrow biopsy (BMB) is a standard bedside
procedure used to evaluate haematological disorders
and oncological diseases. Although rare, complications
of this procedure are well documented. In 2003, Bain[1]
reported 26 adverse events in a total of 54,890 BMB
procedures giving a complication rate of around 0.05%.
Haemorrhage, reported in 14 patients, was the most
frequent and serious adverse event, necessitating blood
transfusion in six patients and causing death in one. There
is no standard guideline for management of vascular
injury following BMB. We report a case of inadvertent
arterial injury during BMB that was successfully
managed by embolisation through the biopsy needle.
CASE REPORT
An 84-year-old woman underwent BMB during workup
for neutropenia. Her coagulation parameters were
normal. A Jamshidi needle (11 gauge) was advanced
from the back towards the right posterior iliac fossa.
Active arterial spurting was encountered on withdrawal of the stylet. The stylet was swiftly replaced. The patient
was transferred to the angiography suite and placed in
the left decubitus position with the needle still in place.
The stylet of the Jamshidi needle was replaced with a
haemostatic Y-adaptor. Contrast injection through the
Jamshidi needle demonstrated an iliolumbar artery
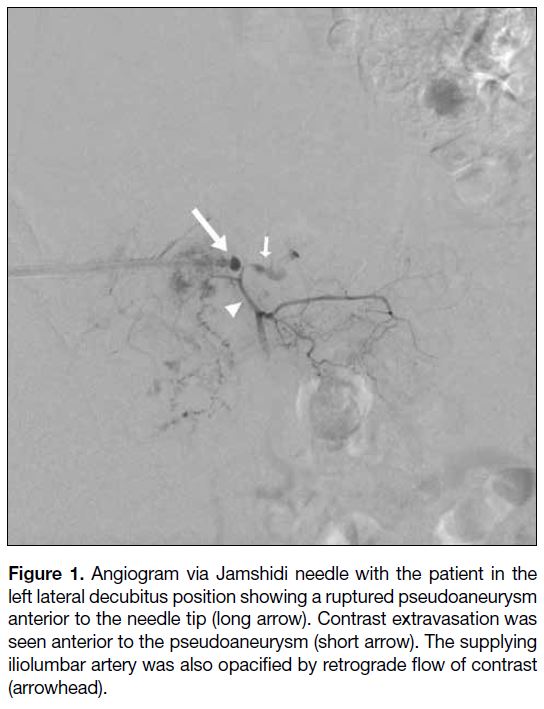
pseudoaneurysm with active extravasation (Figure 1).
No venous injury was evident. Staged embolisation
was performed with gelatin sponge particles first
injected through the Jamshidi needle under fluoroscopic
guidance until near stagnation of antegrade flow was
evident. A 4F Cobra catheter was then fed through the
Jamshidi needle and brought to just proximal to the
pseudoaneurysm at the needle tip. Injection of N-butyl-2-cyanoacrylate (NBCA)/Lipiodol mixture in a 1:3 ratio
through the Cobra catheter was performed until the
pseudoaneurysm and its adjacent branches were full.
The initial administration of gelatin sponge helped to
minimise distal migration of NBCA by slowing blood
flow. Additional NBCA/Lipiodol mixture was injected
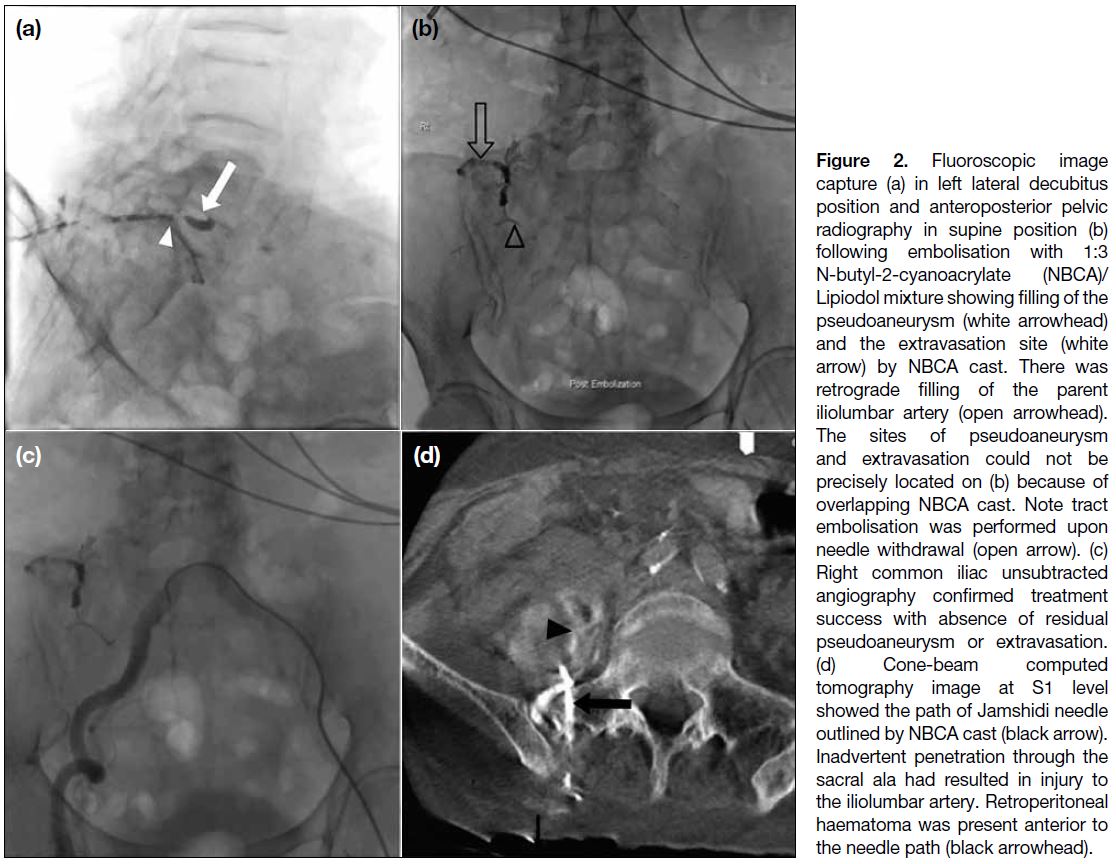
as the Jamshidi needle was withdrawn (Figure 2a and b). The patient was then positioned supine. Right common
iliac arteriogram performed with a 4F Cobra catheter
via the left common femoral artery confirmed occlusion
of the pseudoaneurysm and absence of contrast
extravasation (Figure 2c). Cone-beam computed
tomography (CT) demonstrated a large retroperitoneal
haematoma. The Jamshidi needle path, outlined by glue
cast (Figure 2d), was shown to have deviated superiorly
and medially from the intended trajectory, traversing
the sacral ala and injuring the iliolumbar artery. Despite
the large haematoma, the patient’s vital signs remained
stable throughout. The patient recovered uneventfully
and was discharged 3 days later.
Figure 1. Angiogram via Jamshidi needle with the patient in the
left lateral decubitus position showing a ruptured pseudoaneurysm
anterior to the needle tip (long arrow). Contrast extravasation was
seen anterior to the pseudoaneurysm (short arrow). The supplying
iliolumbar artery was also opacified by retrograde flow of contrast
(arrowhead).
Figure 2. Fluoroscopic image
capture (a) in left lateral decubitus
position and anteroposterior pelvic
radiography in supine position (b)
following embolisation with 1:3
N-butyl-2-cyanoacrylate (NBCA)/Lipiodol mixture showing filling of the
pseudoaneurysm (white arrowhead)
and the extravasation site (white
arrow) by NBCA cast. There was
retrograde filling of the parent
iliolumbar artery (open arrowhead).
The sites of pseudoaneurysm
and extravasation could not be
precisely located on (b) because of
overlapping NBCA cast. Note tract
embolisation was performed upon
needle withdrawal (open arrow). (c)
Right common iliac unsubtracted
angiography confirmed treatment
success with absence of residual
pseudoaneurysm or extravasation.
(d) Cone-beam computed
tomography image at S1 level
showed the path of Jamshidi needle
outlined by NBCA cast (black arrow).
Inadvertent penetration through the
sacral ala had resulted in injury to
the iliolumbar artery. Retroperitoneal
haematoma was present anterior to
the needle path (black arrowhead).
DISCUSSION
BMB is a commonly performed procedure for
haematological conditions. Although BMB is generally
considered safe, adverse events occasionally occur,
particularly retroperitoneal haemorrhage.[1] Incidents of
inadvertent needle puncture through to the anterior side
of the sacrum or iliac bone causing injury to the iliac,
iliolumbar, iliac circumflex, hypogastric, median sacral,
or superior gluteal arteries have been reported, some
leading to fatalities.[2] There is currently no standard guideline on the management of retroperitoneal bleeding
following BMB. Some recommend transarterial
embolisation as first-line treatment.[2] [3] Conservative and
surgical management have also been described. Our
group has previously reported a case of inadvertent
internal iliac artery puncture during BMB that was
successfully embolised with NBCA glue through the
biopsy needle.[4] Tsai et al[5] described a case of Jamshidi
needle-induced iliac artery injury managed by coil
embolisation, also directly through the biopsy needle.
In our case, packing the pseudoaneurysm sac with coils
carried the risk of coil migration or even rupture of the
pseudoaneurysm. For these reasons we opted to use a
liquid embolic agent with the intention of filling the
aneurysm. The major risk was inadvertent embolisation
and tissue ischaemia. The iliolumbar artery arises
from the posterior division of the internal iliac artery
and further divides into an iliac branch that supplies
the iliacus muscle and ilium, and a lumbar branch that
supplies the psoas major and quadratus lumborum
muscles. The lumbar branch also supplies a spinal
branch to the cauda equina.[6] Spilling of embolic agent to
the cauda equina could lead to paraesthesia and paralysis
consequential to nerve damage. To minimise this risk,
we performed a test run with a bolus of contrast medium
prior to administration of NBCA glue to examine the flow
dynamics. During injection of gelatin sponge particles
and NBCA glue, we used the lumbar vertebral bodies
as a landmark, and every effort was made to ensure that
the embolic agent did not cross the lateral border of the
vertebrae to reach the cauda equina. The use of gelatin
sponge prior to NBCA glue also helped to slow arterial
flow and reduce the risk of distal inadvertent spillage of
NBCA glue. Potential advantages of this direct through-the-needle approach over the conventional transarterial
route include more direct access to the bleeding site and
consequent shorter time to haemostasis and less blood
loss due to local tamponade by the needle. A potential
drawback of this percutaneous approach is increased
risk of extravascular deposition of NBCA glue that can
induce foreign body reaction in the soft tissue.[7] A high
index of suspicion for arterial injury during BMB and
retention of the needle in its position are required for this
embolisation technique. Of note, CT angiography was
not performed prior to embolisation. Since spurting of
blood was encountered on stylet withdrawal, arterial
injury was thought to be likely, and the decision was
made to bypass CT and transfer the patient directly to the
angiography suite. The presence of arterial injury was
subsequently confirmed by contrast injection through the
Jamshidi needle. This approach had the advantages of expediting treatment and minimising patient movement
from bed transferral that may have dislodged the needle
and caused life-threatening haemorrhage.
CONCLUSION
Retroperitoneal haemorrhage rarely occurs following
BMB but is potentially fatal. If arterial injury is suspected during BMB, keeping the biopsy needle in place and urgent interventional radiological treatment can be lifesaving.
REFERENCES
1. Bain BJ. Bone marrow biopsy morbidity: review of 2003. J Clin Pathol. 2005;58:406-8. Crossref
2. Gregorio CD, Spalla F, Padricelli A, Narese D, Bracale U, Ferrara D, et al. The endovascular management of an iatrogenic superior gluteal artery rupture following bone marrow biopsy.
Intern Med. 2017;56:2639-43. Crossref
3. Zahrani YA, Peck D. Median sacral artery injury following a bone
marrow biopsy successfully treated with selective trans-arterial
embolization: a case report. J Med Case Rep. 2016;10:42. Crossref
4. Chu F, Tse D, Chan T, Kwong YL. Arterial injury during bone
marrow aspiration: embolization through the biopsy needle. J Vasc
Interv Radiol. 2018;29:584. Crossref
5. Tsai CS, Yu SC. Inadvertent arterial & venous injury by bone
marrow biopsy needle: case report on rescue embolization
techniques. CVIR Endovasc. 2020;3:80. Crossref
6. Bilhim T, Pereira JA, Fernandes L, Rio Tinto H, Pisco JM.
Angiographic anatomy of the male pelvic arteries. AJR Am J
Roentgenol. 2014;203:W373-82. Crossref
7. Canter HI, Vargel I, Mavlll ME, Gököz A, Erk Y. Tissue response to
N-butyl-2-cyanoacrylate after percutaneous injection into cutaneous
vascular lesions. Ann Plast Surg. 2002;49:520-6. Crossref