Fluorodeoxyglucose-Positron Emission Tomography–Computed Tomography Features of Atypical Femoral Lesions in Patients Prescribed Bone-modifying Agents: Two Case Reports
CASE REPORT
Fluorodeoxyglucose-Positron Emission Tomography–Computed Tomography Features of Atypical Femoral Lesions in Patients Prescribed Bone-modifying Agents: Two Case Reports
W Kumamoto, LY Cheng, WY Shen
Department of Orthopaedics and Traumatology, Queen Elizabeth Hospital, Hong Kong
Correspondence: Dr WY Shen. Department of Orthopaedics and Traumatology, Queen Elizabeth Hospital, Hong Kong. Email: wyshen@netvigator.com
Submitted: 1 Feb 2021; Accepted: 12 Apr 2021.
Contributors: WYS designed the study. WK and LYC acquired the data. WK drafted the manuscript. LYC and WYS critically revised the
manuscript for important intellectual content. All authors had full access to the data, contributed to the study, approved the final version for
publication, and take responsibility for its accuracy and integrity.
Conflicts of Interest: All authors have disclosed no conflicts of interest.
Funding/Support: This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data Availability: All data generated or analysed during the present study are included in this published article.
Ethics Approval: This study was approved by the Kowloon Central/Kowloon East Research Ethics Committee (KC/KE-20-0191/ER-3). This retrospective study did not affect management of the reported cases and does not contain any information that could identify patients. The Research Ethics Committee did not require patient consent.
INTRODUCTION
Atypical femoral fracture (AFF) has been reported
in patients prescribed high-dose bisphosphonates or
denosumab. Although metastatic bone lesions and pre-fracture
AFF lesions are evidenced by abnormal uptake in
technetium-99m methylene diphosphonate scintigraphy,
pre-fracture AFF lesions are non-fluorodeoxyglucose
(FDG)-avid. This is the first report of two cases in
which pre-AFF lesions were missed on FDG (positron
emission tomography–computed tomography [PET-CT]
performed routinely for monitoring of tumour progress).
Careful multiplanar reformation (MPR) scrutiny of CT
images on FDG-PET-CT might reveal the beaking typical
of a pre-AFF lesion in the proximal femur, and thus
offer a chance for timely plain radiograph confirmation
and consideration of prophylactic fixation based on full
assessment of clinical and imaging findings.
CASE REPORTS
Case 1
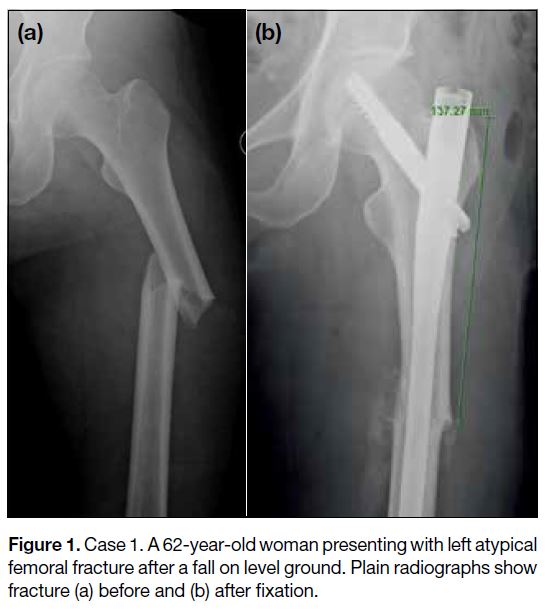
In April 2020, a 62-year-old woman presented with a left AFF after a fall on level ground. 9 years before this,
the patient was diagnosed with carcinoma of the breast,
which was treated with mastectomy and chemotherapy.
3 years later, the patient was started on zoledronic acid,
initially 4 mg every 3 weeks for 18 months, and then
4 mg every 3 months, continuing to the present (>6 years
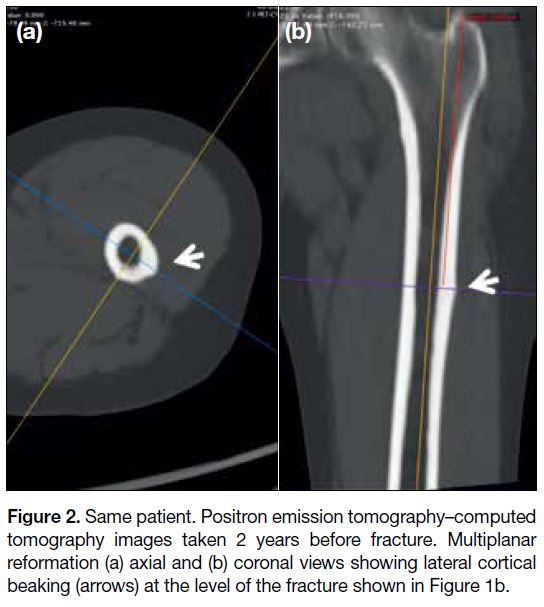
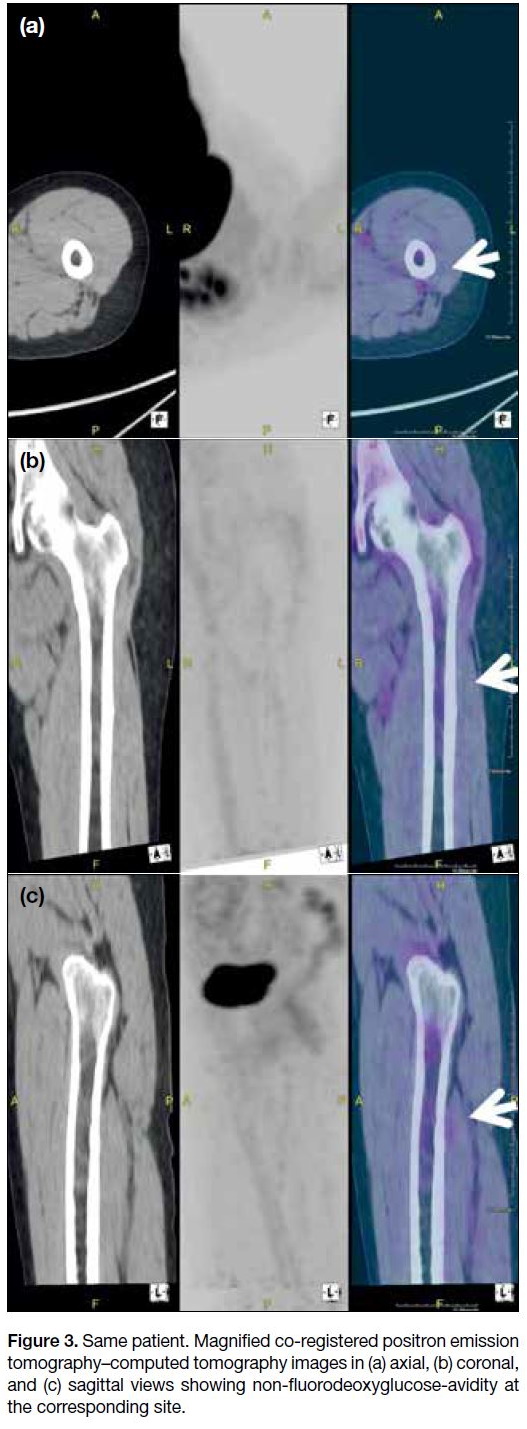
of zoledronic acid treatment). A retrospective review of
an FDG-PET-CT performed 20 months prior to the fall
revealed no FDG-avid lesion in either proximal femur.
However, MPR of the FDG-PET-CT images showed
evidence of lateral cortical beaking at the left proximal
femur, corresponding to the site of the subsequent AFF
(Figures 1 2 3). The fracture was surgically treated
with cephalomedullary nail fixation, and withdrawal of
the bone-modifying agent (BMA) / bone-targeted agent
(BTA). Histopathology results of bone biopsy were
negative for malignant cells.
Figure 1. Case 1. A 62-year-old woman presenting with left atypical
femoral fracture after a fall on level ground. Plain radiographs show fracture (a) before and (b) after fixation
Figure 2. Same patient. Positron emission tomography–computed
tomography images taken 2 years before fracture. Multiplanar
reformation (a) axial and (b) coronal views showing lateral cortical beaking (arrows) at the level of the fracture shown in Figure 1b
Figure 3. Same patient. Magnified co-registered positron emission
tomography–computed tomography images in (a) axial, (b) coronal,
and (c) sagittal views showing non-fluorodeoxyglucose-avidity at
the corresponding site
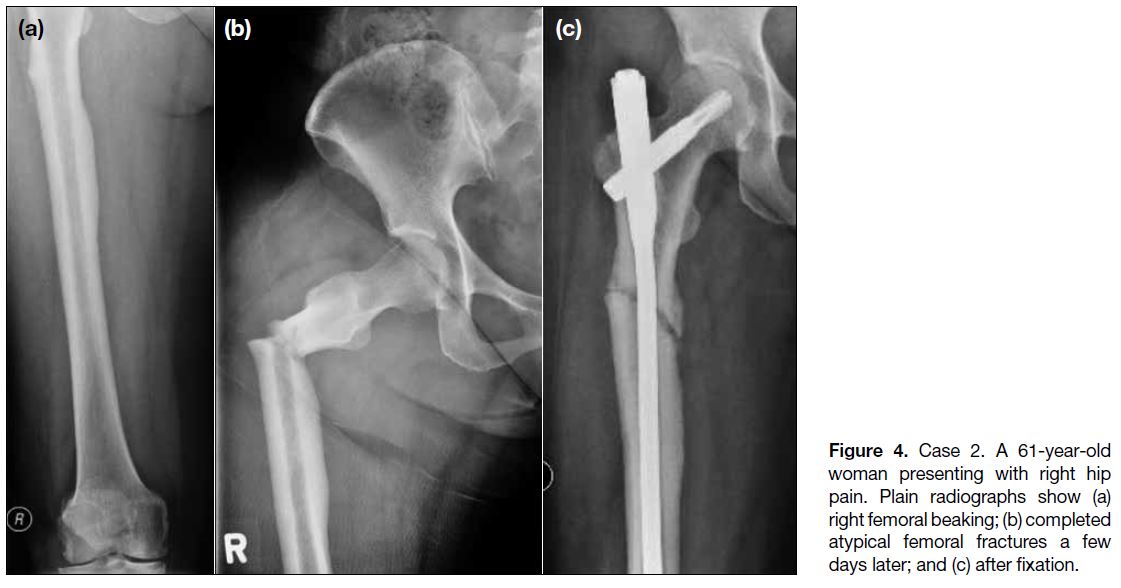
Case 2
In October 2018, a 61-year-old woman presented with right hip pain. 6 years before this, the patient was diagnosed with carcinoma of the breast, which was
treated with mastectomy and chemotherapy. 1 year
later, the patient was started on high-dose denosumab (120 mg every 4 weeks), continuing to the present
(>5 y of denosumab therapy). Plain radiograph revealed
lateral cortical beaking in the proximal femur. A few days later, she sustained a complete subtrochanteric fracture
of the right femur after trivial injury. Retrospective
review of the FDG-PET-CT done 3 months prior to the
fracture revealed no FDG-avid lesion in either proximal
femur, but MPR of the CT images showed evidence
of lateral cortical beaking at the right proximal femur
(Figures 4 5 6). The fracture was surgically treated
with cephalomedullary nail fixation, and withdrawal of
the BMA / BTA. Histopathology results of bone biopsy
were negative for malignant cells.
Figure 4. Case 2. A 61-year-old woman presenting with right hip pain. Plain radiographs show (a) right femoral beaking; (b) completed atypical femoral fractures a few days later; and (c) after fixation
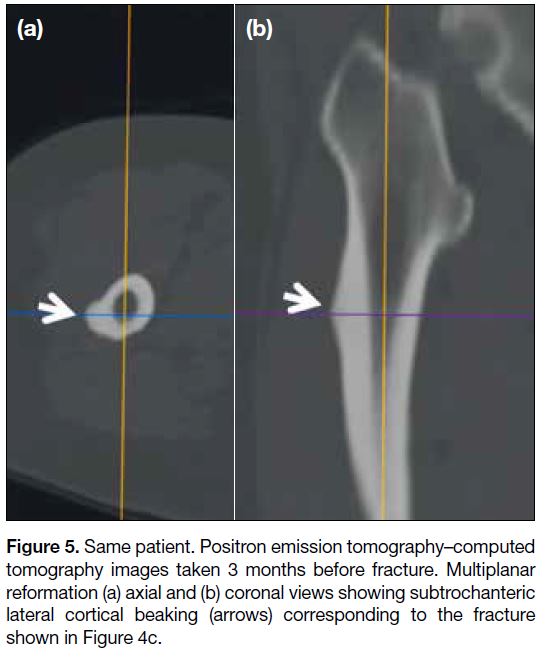
Figure 5. Same patient. Positron emission tomography–computed
tomography images taken 3 months before fracture. Multiplanar
reformation (a) axial and (b) coronal views showing subtrochanteric
lateral cortical beaking (arrows) corresponding to the fracture
shown in Figure 4c
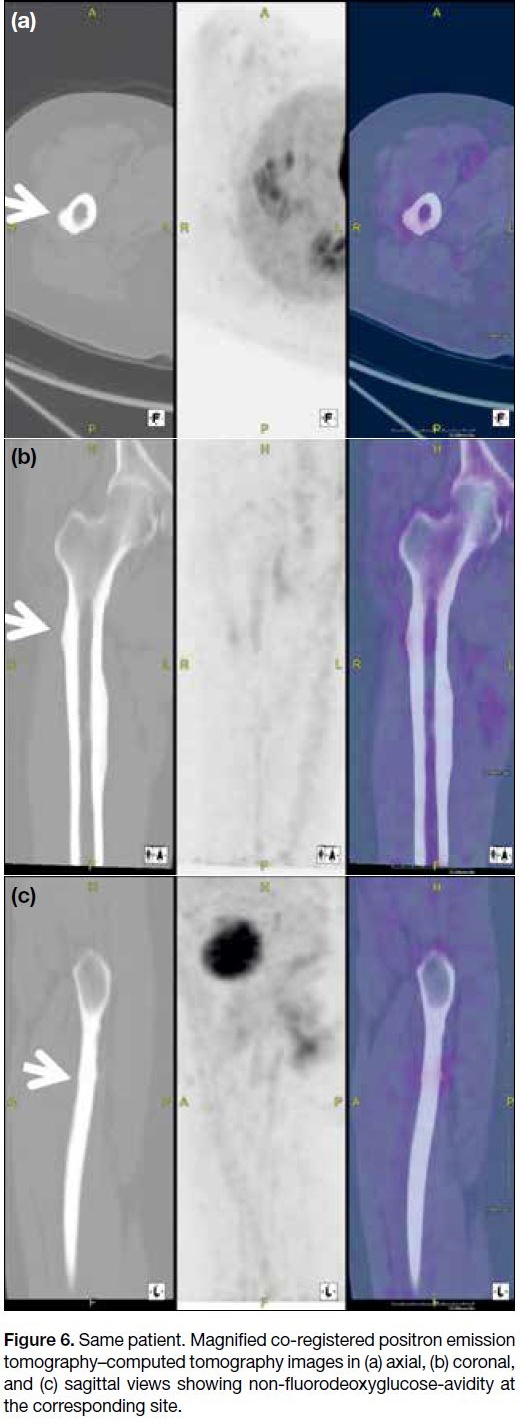
Figure 6. Same patient. Magnified co-registered positron emission
tomography–computed tomography images in (a) axial, (b) coronal,
and (c) sagittal views showing non-fluorodeoxyglucose-avidity at
the corresponding site
DISCUSSION
AFF is a serious complication of BMAs or BTAs used in the treatment of bone metastases from breast, prostate
and other solid malignancies. Osteoclast inhibitors,
bisphosphonates and denosumab are powerful BMAs.
The incidence of AFF beaking in patients prescribed
BMAs has been reported at 12.5% and frank fracture
at 7.8%.[1] A recent search of the literature revealed no
reports of pre-fracture AFF lesions detected on PET-CT.
Takahashi et al[2] mentioned that PET-CT revealed no
abnormal uptake although radiographs showed cortical
thickening in one of the cases reported, indicating that
these pre-fracture AFF lesions might not be FDG-avid.
This is the first report that pre-fracture AFF lesions, such
as lateral cortical beaking in the femur, can be identified
on MPR of PET-CT images.
Because PET-CT is regularly used to monitor disease progress in patients prescribed BMAs/BTAs, radiologists
should be specifically alerted to their drug history. This
should prompt more detailed MPR study of proximal
femur CT images to look for the presence of cortical
thickening despite the potential absence of FDG-avid
lesions.
Radiologically, the earliest suggestion of AFF is a localised lesion with increased thickness of the lateral
cortex described as “beaking”. As it progresses, a
“dreaded black line” may be seen at the most prominent
part of the beak. These radiological features of pre-fracture
AFF can be confirmed on timely plain radiograph
of the femur and serve as warning signs of an impending
AFF. Although different surgeons may have different
thresholds for prophylactic fixation, this early finding
may alert the clinician to the need for further clinical
and imaging assessment of the suspicious lesion.[3]
Prophylactic fixation of pre-fracture AFF is highly
effective in preventing the agony and complications of
a complete AFF.[4] Treatment of completed AFF is more
technically demanding and associated with a high risk of
delayed union, non-union and implant failures.[5]
Pre-fracture AFF is not evidenced as abnormal uptake in FDG scan but may be detected on detailed MPR scrutiny
of CT images. The referring clinician should alert the
radiologist of a patient’s drug history in order to make
best use of PET-CT for disease progress monitoring.
REFERENCES
1. Ota S, Inoue R, Shiozaki T, Yamamoto Y, Hashimoto N, Takeda O, et al. Atypical femoral fracture after receiving antiresorptive drugs in breast cancer patients with bone metastasis. Breast Cancer. 2017;24:601-7. Crossref
2. Takahashi M, Ozaki Y, Kizawa R, Masuda J, Sakamaki K,
Kinowaki K, et al. Atypical femoral fracture in patients with bone
metastasis receiving denosumab therapy: a retrospective study and
systematic review. BMC Cancer. 2019;19:980. Crossref
3. Lee KJ, Min BW, Bae KC, Cho CH, Lee SW, Kim BS. Progression
of asymptomatic contralateral femur in patients with complete
atypical femoral fracture, according to initial radiographic findings.
J Bone Joint Surg Am. 2021;103:123-30. Crossref
4. Egol KA, Park JH, Prensky C, Rosenberg ZS, Peck V, Tejwani NC.
Surgical treatment improves clinical and functional outcomes for
patients who sustain incomplete bisphosphonate-related femur
fractures. J Orthop Trauma. 2013;27:331-5. Crossref
5. Koh A, Guerado E, Giannoudis PV. Atypical femoral fractures related to bisphosphonate treatment: issues and controversies related to their surgical management. Bone Joint J. 2017;99-B:295-302. Crossref