Focal Bone Lesions Following Ultrasound Diathermy: Case Series
ORIGINAL ARTICLE
Focal Bone Lesions Following Ultrasound Diathermy: Case Series
CSC Tsai1, RKL Lee1, KKW Tam2, PSH Yung3, JF Griffith1
1 Department of Imaging and Interventional Radiology, Prince of Wales Hospital, The Chinese University of
Hong Kong, Hong Kong
2 Orthopaedics, Asia Medical Specialists
3 Department of Orthopaedics and Traumatology, Prince of Wales Hospital, The Chinese University of Hong
Kong, Hong Kong
Correspondence: Prof. JF Griffith, Department of Imaging and Interventional Radiology, Prince of Wales Hospital, The Chinese University of Hong Kong, Hong Kong. Email: griffith@cuhk.edu.hk
Submitted: 15 May 2020; Accepted: 16 Nov 2020.
Contributors: CSCT, RKLL, and JFG designed the study. All authors acquired and analysed the data. CSCT, RKLL, and JFG drafted the manuscript. All authors critically revised the manuscript for important intellectual content. All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of Interest: All authors have disclosed no conflicts of interest.
Funding/Support: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data Availability: All data generated or analysed during the present study are available from the corresponding author on reasonable request.
Ethics Approval: This study was approved by the Joint Chinese University of Hong Kong–New Territories East Cluster Clinical Research Ethics Committee (Joint CUHK-NTEC CREC Ref: 2022.124).
Abstract
Introduction
We sought to describe focal bone lesions detected on magnetic resonance imaging (MRI) in patients
following ultrasound diathermy.
Methods
We performed a retrospective analysis of MRI characteristics of bone lesions in 10 patients who underwent
ultrasound diathermy for musculoskeletal conditions followed by plain radiographs and MRI for pain. Magnetic
resonance arthrography was performed in two patients and one patient had a second follow-up MRI examination.
A phone interview was conducted with all patients.
Results
All 10 patients had experienced mild to severe pain during ultrasound diathermy, with four (40%) prematurely
terminating the treatment session as a result. Plain radiographs were normal. On MRI, a total of 12 lesions were
observed in the 10 patients, with nine lesions in eight shoulder joints, two lesions in one ankle joint, and one lesion in
the first metacarpal base. All lesions were small to medium-sized (6 × 5 × 3 mm to 32 × 23 × 9 mm), well-demarcated
and subcortical in location with a crescentic or oblong configuration. Lesions were highly conspicuous on T2-weighted
images and relatively inconspicuous on T1- or intermediate weighted sequences. Typically, larger lesions had a
T2-hyperintense rim surrounding an isointense central area. Leakage of arthrographic contrast into the lesion was
observed. The overall features favoured focal osteonecrosis in all cases. The affected locations typically had little
overlying subcutaneous tissue, were close to tendon insertions, and corresponded to the site of ultrasound diathermy
application in all patients.
Conclusion
Appearances akin to focal osteonecrosis may result from application of ultrasound diathermy. Recognition
of the characteristic appearance will allow this connection to be made to avoid subsequent unnecessary workup.
Key Words: Bone diseases; Diathermy; Magnetic resonance imaging; Ultrasonography
中文摘要
超聲波透熱療後的局灶性骨病變:病例系列報告
蔡紹俊、李嘉樂、譚國偉、容樹恒、JF Griffith
引言
本研究旨在描述超聲波透熱療後患者在磁共振成像(MRI)檢測的局灶性骨病變。
方法
我們回顧分析10名因肌肉骨骼疾病接受超聲波透熱療的患者的骨病變MRI 特徵,隨後通過X光平片和MRI進行疼痛檢查。對兩名患者進行MR關節造影,一名患者進行第二次隨訪MRI。對所有患者進行電話訪談。
結果
所有患者在超聲波透熱療期間都出現中度至劇烈疼痛,其中4名患者(40%)因此提前終止治療。X光平片結果無異常情況。10例患者於MRI檢查發現共12個病灶,其中肩關節8例共9個病灶、踝關節1例共2個病灶,以及第一掌骨基部1個病灶。所有病灶屬細至中等大小(介乎6 × 5 × 3 mm至32 × 23 × 9 mm),邊界清楚且位於皮質下,呈新月形或橢圓形。病變在T2加權圖像上非常明顯,在T1加權或中間加權序列上相對不明顯。較大的病灶通常在等信號中心區域邊緣呈T2高信號,以及關節造影顯影劑滲出病灶。所有病例的整體特徵有利局灶性骨壞死。受影響位置通常幾乎沒有覆蓋的皮下組織、靠近肌腱插入處,且與所有患者的超聲波透熱療應用部位對應。
結論
類似局灶性骨壞死的外觀可能由於使用超聲透熱療所致。識別這種特徵外觀有助避免不必要的後續檢查。
INTRODUCTION
Musculoskeletal symptoms including pain, tenderness,
and restricted movement, are common indications
for referral to physiotherapy treatment. One of the
physiotherapy treatments used to relieve inflammation
and promote healing is the application of heat treatment
either in the form of hot packs or deep heat diathermy.[1] [2] [3]
Deep heat diathermy can be achieved using therapeutic
ultrasound, shockwaves, or microwaves.[4] [5]
Some studies have indicated ultrasound diathermy to be effective[4] [6] while others show no demonstrable benefit.[7] [8]
Ultrasound diathermy can result in thermal injury to the
skin, subcutaneous tissue and muscles.[1] [2] [3] An uncommon
complication of diathermy is injury to the cortical bone,
causing osteonecrosis.[9] During the past 3 years, we
encountered 10 patients who had received diathermy
treatment and had bone lesions visible on subsequent
magnetic resonance imaging (MRI) examinations
performed for pain. These bone lesions were identical to
the osteonecrosis previously reported as being related to
diathermy treatment.9 Some of these bone lesions were
not initially recognised as being possibly iatrogenic,
prompting unnecessary additional investigations. The
aim of this study was to both review the magnetic resonance (MR) appearances of these lesions, and to
increase awareness of their occurrence and significance.
METHODS
Patients who presented to our institution in 2018 and
2019 with symptomatic bone lesions of the shoulder,
ankle, or wrist following diathermy treatment were
identified and reviewed. All patients had been referred for
musculoskeletal joint symptoms following diathermy.
For all patients, radiographs of the symptomatic sites
taken before MRI examination showed no abnormalities.
After MRI examinations, all patients underwent a
telephone interview conducted by one of the authors
(RKLL). Specific features queried during this interview
were whether ultrasound diathermy was performed, the
time lag between diathermy and MRI, the number of
diathermy sessions, and the pain level (mild, moderate,
severe) during the diathermy session.
MRI examinations were performed on a 1.5 T MRI
scanner (Ingenia 1.5T MR System; Philips, Best, the
Netherlands) in one of two imaging centres using
standard joint imaging protocols. Two patients underwent
MR arthrography and one patient had a subsequent follow-up MRI examination. Intravenous contrast was
not administered to any patient. All MR examinations
were analysed by two musculoskeletal radiologists
with 3 and 29 years’ experience, respectively. Features
noted were the appearance of bone lesion on T1-, proton
density, and T2-fat-saturated sequences; lesion number,
location, configuration, and dimensions; as well as the
appearance of the overlying soft tissue. The relationship
between lesion volume (width × depth × length × 0.52)
or maximum depth and lesion appearance was analysed.
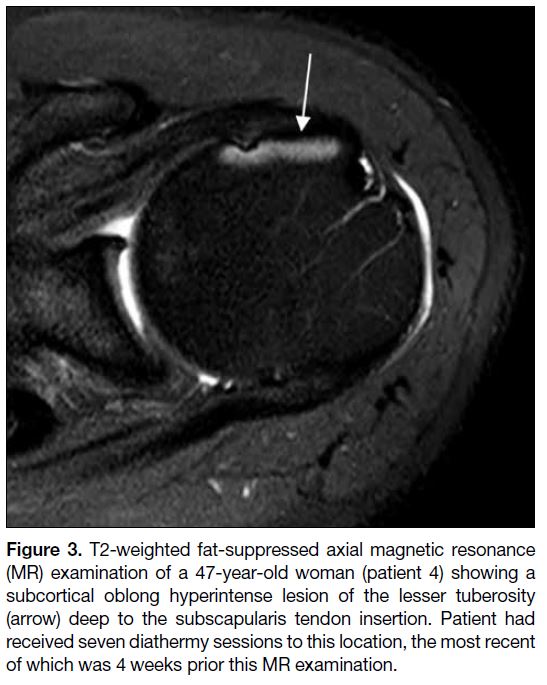
RESULTS
In total, 10 patients (8 men, 2 women; mean age=40.7
years, range, 29-52) were identified and reviewed in
2018 and 2019. All patients had received ultrasound diathermy therapy for symptoms of the shoulder (n=8,
80%), ankle (n=1, 10%) and wrist (n=1, 10%) [Table].
All the unusual bone lesions evident on MR were
located at the site of diathermy treatment. The number of
diathermy sessions before the MRI examination ranged
from 3 to 7 sessions (mean, 5 sessions) [Table]. The time
lag between diathermy and the MRI ranged from 1 to
24 weeks (mean=6 ± 7 weeks). All patients reported pain
during diathermy, graded as mild in six (60%) patients
and severe in four (40%) patients. These four patients
with severe pain discontinued diathermy treatment due
to pain.
Table. Patient and magnetic resonance details
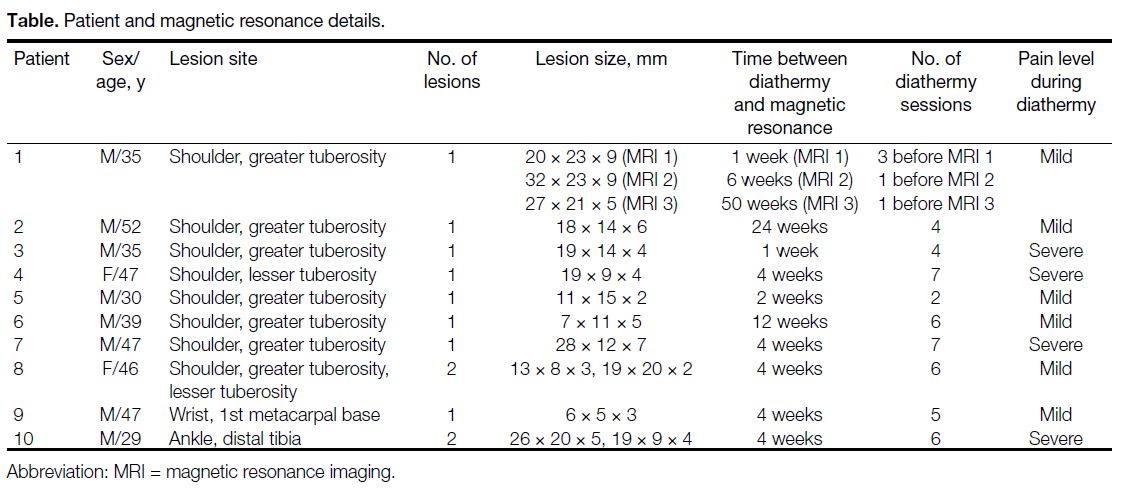
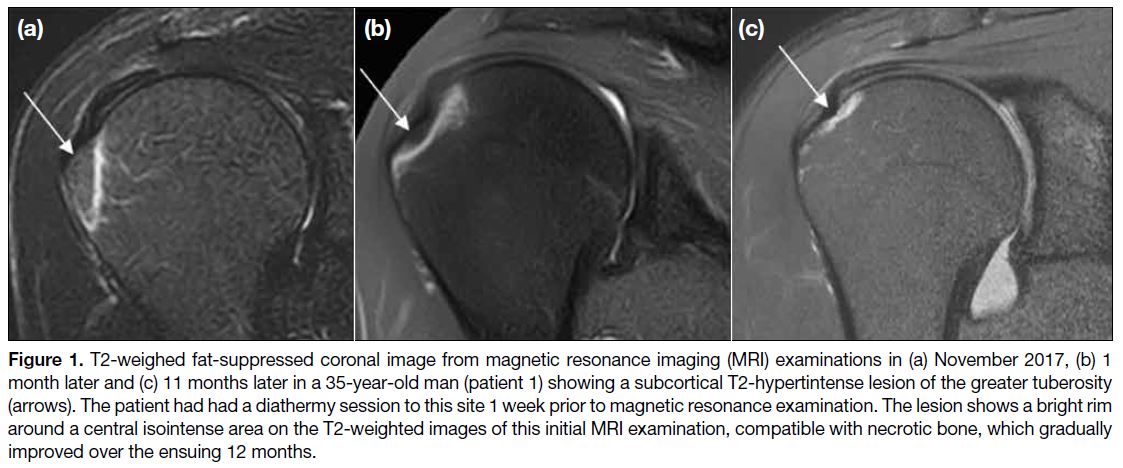
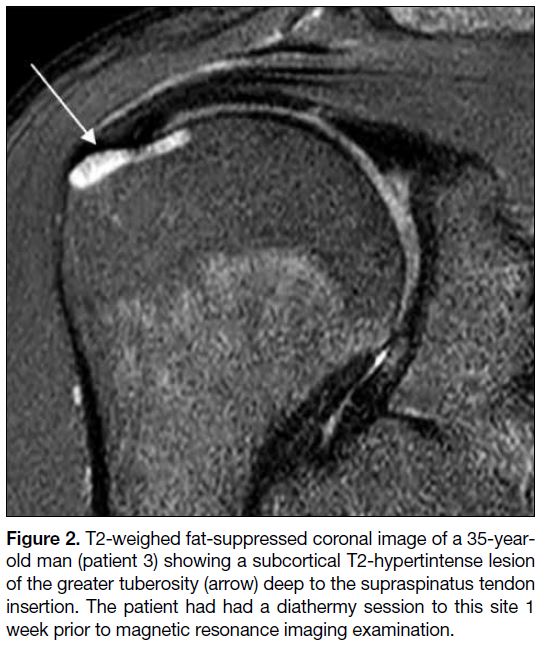
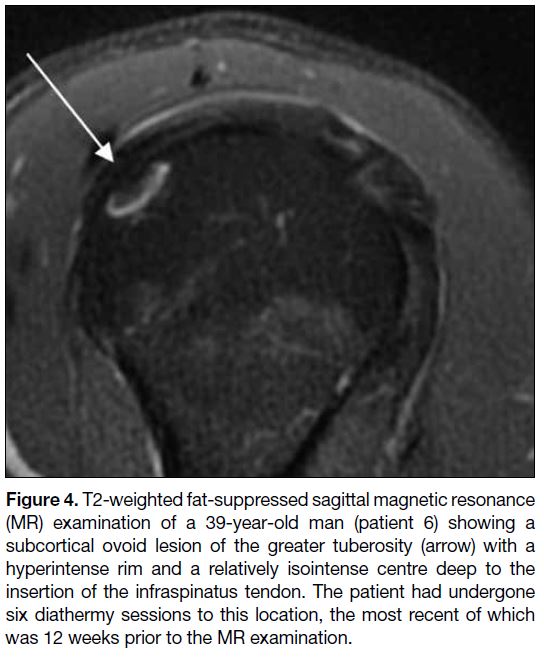
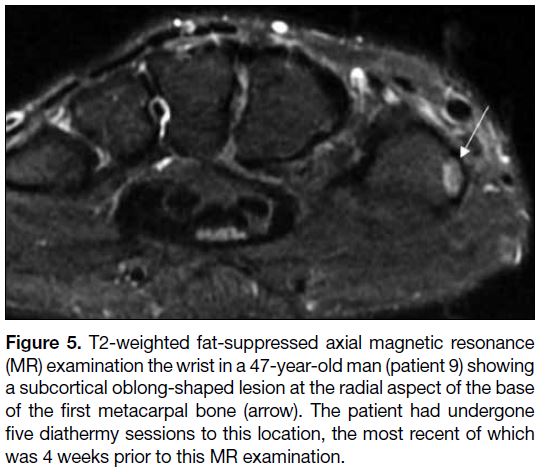
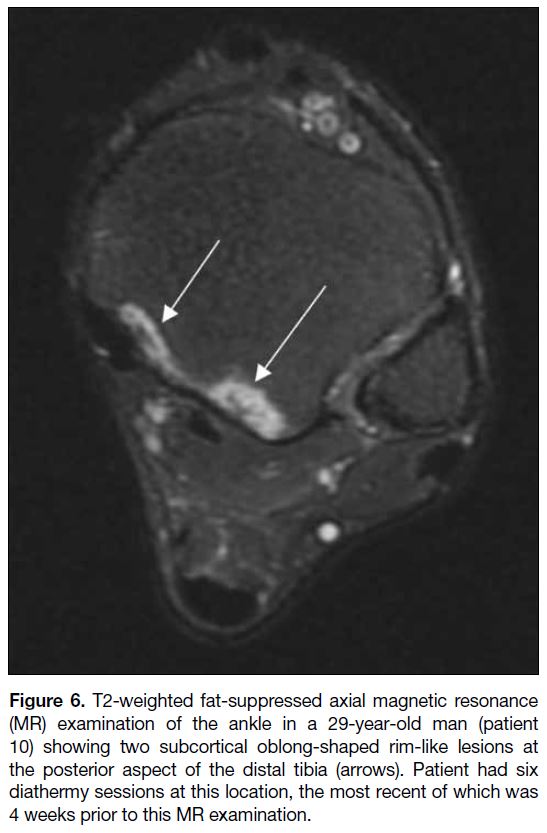
A total of 12 bone lesions were present in the 10 patients (Figures 1 2 3 4 5 6). All bone lesions were subcortical and at a relatively superficial location, i.e. with little soft
tissue between the skin and the bone surface. All bone
lesions had a rounded or oblong lesion shape with a thick hyperintense rim on T2-weighted images. A central
isointense area was present in eight (67%) of the 12
lesions. No relationship between lesion volume (p=0.30)
or lesion depth (p=0.43) and this central isointense area
was found. There was no surrounding bone marrow
oedema. The overlying cortex was intact without bone
collapse or fracture and the overlying soft tissues were
also unremarkable without oedema or inflammation.
Figure 1. T2-weighed fat-suppressed coronal image from magnetic resonance imaging (MRI) examinations in (a) November 2017, (b) 1
month later and (c) 11 months later in a 35-year-old man (patient 1) showing a subcortical T2-hypertintense lesion of the greater tuberosity
(arrows). The patient had had a diathermy session to this site 1 week prior to magnetic resonance examination. The lesion shows a bright rim
around a central isointense area on the T2-weighted images of this initial MRI examination, compatible with necrotic bone, which gradually
improved over the ensuing 12 months.
Figure 2. T2-weighed fat-suppressed coronal image of a 35-year-old
man (patient 3) showing a subcortical T2-hypertintense lesion
of the greater tuberosity (arrow) deep to the supraspinatus tendon
insertion. The patient had had a diathermy session to this site 1
week prior to magnetic resonance imaging examination.
Figure 3. T2-weighted fat-suppressed axial magnetic resonance
(MR) examination of a 47-year-old woman (patient 4) showing a
subcortical oblong hyperintense lesion of the lesser tuberosity
(arrow) deep to the subscapularis tendon insertion. Patient had
received seven diathermy sessions to this location, the most recent
of which was 4 weeks prior this MR examination.
Figure 4. T2-weighted fat-suppressed sagittal magnetic resonance
(MR) examination of a 39-year-old man (patient 6) showing a
subcortical ovoid lesion of the greater tuberosity (arrow) with a
hyperintense rim and a relatively isointense centre deep to the
insertion of the infraspinatus tendon. The patient had undergone
six diathermy sessions to this location, the most recent of which
was 12 weeks prior to the MR examination.
Figure 5. T2-weighted fat-suppressed axial magnetic resonance
(MR) examination the wrist in a 47-year-old man (patient 9) showing
a subcortical oblong-shaped lesion at the radial aspect of the base
of the first metacarpal bone (arrow). The patient had undergone
five diathermy sessions to this location, the most recent of which
was 4 weeks prior to this MR examination.
Figure 6. T2-weighted fat-suppressed axial magnetic resonance
(MR) examination of the ankle in a 29-year-old man (patient
10) showing two subcortical oblong-shaped rim-like lesions at
the posterior aspect of the distal tibia (arrows). Patient had six
diathermy sessions at this location, the most recent of which was
4 weeks prior to this MR examination.
DISCUSSION
We present a series of patients with unusual bone lesions
on MRI following diathermy treatment. All lesions
were similar in appearance, being well-demarcated,
subcortical in location, small- to medium-sized, located
close to the skin surface, with a thick rim of hyperintense
signal on T2-weighted images indicative of immature
granulation tissue or inflammation with a central more
isointense area indicative of osteonecrotic tissue.
All patients had received diathermy to the affected
areas shortly before MRI examination. As no MRI
prior to ultrasound diathermy was available, cause and
effect were not established, though, a direct causation
relationship was, nevertheless, very likely. A single
previous report of eight patients demonstrating identical
bone lesions in the shoulder, knee, and wrist following
ultrasound diathermy treatment also considered these
bone lesions to be iatrogenic.[9]
Although none of the bone lesions presented here or
previously[9] underwent biopsy, the imaging appearances
are compatible with subcortical osteonecrosis.
Subcortical osteonecrosis typically has an oblong-shaped
configuration with a hyperintense rim on T2-weighted
images due to immature reparative granulation tissue and
an isointense central area due to necrotic bone.[10] It has
been found that if the osteonecrotic area is large, vascular
compromise will limit repair to a degree that appreciable
healing will not occur.[11] However, if the osteonecrotic
area is small, the initial vascular compromise can be
circumvented, provided the initial insult is discontinued,
enabling small areas of osteonecrosis to heal over time
with revascularisation and bone repair.[12] Such a healing
response was apparent in the one case presented that
underwent follow-up MRI and in three (38%) of the
eight patients reported by Yeh et al.[9]
Therapeutic ultrasound can be low or high intensity.
Low-intensity (0.03-3.0 Wcm2) therapeutic ultrasound is
used in ultrasound diathermy to treat soft tissue injury.
Low-intensity pulsed ultrasound is used to accelerate
fracture healing.[4] [13] At the other end of the scale, high-intensity
focused ultrasound (~1000 Wcm2) uses a
tightly focused ultrasound beam to treat tumours of the
breast, prostate, liver, uterus, and bone.[5] Absorption of
ultrasound energy leads to tissue heating. Diathermy aims
to heat the soft tissues to increase local blood flow and
promote tissue healing.[4] [5] Any heating effect is highest
at the skin surface and reduces with increasing depth
due to ultrasound beam absorption and reflection.[14] As
bone is a highly reflective interface, ultrasound energy
absorption into bone is minimal. However, at very
high energy levels, high-intensity focused ultrasound
can induce bone osteonecrosis, by osteocyte damage
and vascular thrombosis, with a direct relationship
existing between ultrasound exposure duration, tissue
temperature and bone damage for temperatures above
43°C.[11] Other than the patients presented here and the
one previous report,[9] low-intensity ultrasound diathermy
has not been recognised to cause bone changes. While
the superficial location of the affected bone areas would
have increased susceptibility to any ultrasound beam,
the effect of specific technical parameters such as
ultrasound duration, mode (continuous, long or short
pulsed), beam intensity, and frequency is not known
as these were not investigated in this study. Ultrasound
diathermy treatment parameters were available in three
(38%) of the eight patients previously reported and all
of these were considered to be within the recommended
treatment range.[9]
Ultrasound diathermy was performed for focal joint
symptoms with radiographs and MRI being requested for
persistent symptoms. As we did not specifically enquire
whether symptoms deteriorated or changed following
ultrasound diathermy treatment, we could not ascertain
how, if at all, symptoms were directly attributable
to the bone lesions. Small areas of osteonecrosis are
often asymptomatic.[10] [12] Focal symptoms did, however,
improve in all previously reported patients for whom
follow-up data were available.[9]
In conclusion, a series of patients with focal bone lesions following ultrasound diathermy treatment is presented.
The aim of this presentation was to increase clinical
awareness of these unusual bone lesions, which most
likely represent areas of subcortical osteonecrosis. In
the appropriate clinical context, no further investigation
is necessary. Reports with follow-up of these lesions
suggest they are reversible with no long-term sequelae.
REFERENCES
1. Giombini A, Giovannini V, Di Cesare A, Pacetti P, Ichinoseki-Sekine N, Shiraishi M, et al. Hyperthermia induced by microwave
diathermy in the management of muscle and tendon injuries. Br
Med Bull. 2007;83:379-96. Crossref
2. Leung MS, Cheing GL. Effects of deep and superficial heating in
the management of frozen shoulder. J Rehabil Med. 2008;40:145-50. Crossref
3. Robertson VJ, Ward AR, Jung P. The effect of heat on tissue extensibility: a comparison of deep and superficial hearting. Arch Phys Med Rehabil. 2005;86:819-25. Crossref
4. Watson T. Ultrasound in contemporary physiotherapy practice. Ultrasonics. 2008;48:321-9. Crossref
5. ter Haar G. Therapeutic applications of ultrasound. Prog Biophys Mol Biol. 2007;93:111-29. Crossref
6. Khanna A, Nelmes RT, Gougoulias N, Maffulli N, Gray J. The
effects of LIPUS on soft-tissue healing: a review of literature. Br
Med Bull. 2009;89:169-82. Crossref
7. Shanks P, Curran M, Fletcher P, Thompson R. The effectiveness of
therapeutic ultrasound for musculoskeletal conditions of the lower
limb: a literature review. Foot (Edinb). 2010;20:133-9. Crossref
8. Alexander LD, Gilman DR, Brown DR, Brown JL, Houghton PE. Exposure to low amounts of ultrasound energy does not improve soft tissue shoulder pathology: a systematic review. Phys Ther. 2010;90:14-25. Crossref
9. Yeh LR, Chen CK, Tsai MY, Teng HC, Lin KL. Focal bone
abnormality as a complication of ultrasound diathermy: a report
of eight cases. Radiology. 2011;260:192-8. Crossref
10. Schmitt R, Kalb KH, Christopoulos G, Grunz JP. Osteonecrosis of the upper extremity: MRI-based zonal patterns and differential diagnosis. Semin Musculoskelet Radiol. 2019;23:523-33. Crossref
11. Long T, Xu J, McClure SR, Amin V, Haynes J. Potential femoral
head osteonecrosis model induced by high-intensity focused
ultrasound. Ultrasound Med Biol. 2013;39:1056-65. Crossref
12. Griffith JF. Musculoskeletal complications of severe acute respiratory syndrome. Semin Musculoskelet Radiol. 2011;15:554-60. Crossref
13. Watanabe Y, Matsushita T, Bhandari M, Zdero R, Schemitsch EH. Ultrasound for fracture healing: current evidence. J Orthop Trauma. 2010;24 Suppl 1:S56-61. Crossref
14. Demmink JH, Helders PJ, Hobaek H, Enwemeka C. The variation of heating depth with therapeutic ultrasound frequency in physiotherapy. Ultrasound Med Biol. 2003;29:113-8. Crossref