Diagnostic Accuracy of Conventional T2- Versus Diffusion-Weighted Magnetic Resonance Imaging in Distinguishing Benign from Malignant Liver Lesions
ORIGINAL ARTICLE
Diagnostic Accuracy of Conventional T2- Versus Diffusion-Weighted Magnetic Resonance Imaging in Distinguishing Benign from Malignant Liver Lesions
F Çengel1, Öİ Karahan2
1 Health Sciences University, Gaziosmanpaşa Training and Research Hospital, Department of Radiology, Istanbul, Turkey
2 Erciyes University Medical Faculty, Department of Radiology, Kayseri, Turkey
Correspondence: Dr F Çengel, Health Sciences University, Gaziosmanpaşa Training and Research Hospital, Department of Radiology, Istanbul, Turkey. Email: doc_20_1@hotmail.com
Submitted: 19 Jan 2021; Accepted: 13 May 2021.
Contributors: Both authors designed the study and were responsible for acquisition of data and contributed to the analysis of data. FÇ drafted the manuscript. Both authors made critical revisions of the intellectual content of this article. Both authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of Interest: The authors have no conflicts of interest to declare.
Funding/Support: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data Availability: All data generated or analysed during the present study are available from the corresponding author on reasonable request.
Ethics Approval: This study was approved by our hospital ethics committee (Ref: 2015-182). The need for signed informed consent was waived due to the retrospective nature of the study.
Abstract
Objective
The aim of this retrospective study was to compare the diagnostic accuracy of conventional T2-weighted
images (T2WI) and diffusion-weighted imaging (DWI) to distinguish between benign and malignant liver lesions.
Methods
Lesions were assessed using a 1- to 5-point (1, benign; 5, definitely malignant) scoring system based on
T2WI and signal characteristics on DWI. The sensitivity, specificity, and accuracy of T2WI and DWI were calculated
for benign and malignant lesions.
Results
A total of 587 focal liver lesions in 561 patients were included in the study. There were 449 benign and
138 malignant lesions. The mean ± standard deviation scores of benign lesions obtained in T2WI and DWI were
1.4 ± 0.8 and 1.7 ± 1.0, respectively, while the same scores in malignant lesions were 4.5 ± 0.8 and 4.4 ± 0.9,
respectively. The sensitivity, specificity, and accuracy of T2WI in distinguishing benign from malignant liver lesions
was 94%, 94%, and 94%, respectively. The same values were calculated as 96%, 85% and 88% for DWI, respectively.
Conclusion
Both imaging methods had high efficiency in characterisation of benign and malignant liver lesions.
T2WI and DWI can be used safely in characterisation of liver lesions in individuals who cannot be given contrast
agents due to reasons such as renal failure and contrast allergy.
Key Words: Diagnostic tests, routine; Liver neoplasms; Magnetic resonance imaging; Sensitivity and specificity
中文摘要
常規T2與彌散加權磁共振成像區分良惡性肝病灶的診斷準確性
F Çengel、Öİ Karahan
目的
本回顧研究分析磁共振常規T2(T2WI)與彌散加權(DWI)成像區分性良惡性肝病灶的診斷準確性。
方法
使用基於T2WI和DWI信號特徵的1至5分評分系統評估病變(1 = 良性;5 = 絕對惡性)。計算T2WI和DWI對良惡性病變的敏感性、特異性和準確性。
結果
共納入561例患者的587個局灶性肝病變。良性病變449個,惡性病變138個。在T2WI和DWI的積分(均值 ± 標準差)在良性病變分別為1.4 ± 0.8和1.7 ± 1.0,在惡性病變分別為4.5 ± 0.8和4.4 ± 0.9。T2WI鑑別肝良惡性病變的敏感性、特異性和準確性分別為94%、94%和94%。DWI為96%、85%和88%。
結論
兩種影像學方法在鑑別肝臟良惡性病變方面效果良好。對於腎衰竭和造影劑過敏等原因而無法給予造影劑的患者,使用T2WI和DWI區分肝病變是安全的。
INTRODUCTION
Ultrasonography (US), computed tomography (CT),
and magnetic resonance imaging (MRI) are the most
commonly used imaging methodologies in the detection
and characterisation of liver lesions. Advances in MRI
technology and faster imaging techniques have made
it a problem-solving modality with high soft tissue
resolution in cases where CT and US are inconclusive.[1]
Diffusion-weighted imaging (DWI) is a technique
that does not require the use of contrast agents. It
is often employed in acute ischaemic processes in
neuroradiology.[1] Thanks to the development of rapid
imaging techniques, the reduction of artefacts caused
by respiratory motion has enabled DWI to be used in
abdominal imaging, especially in the evaluation of liver
lesions.[2] [3] [4] MRI is the modality of preference for imaging
the central nervous system (except for trauma patients),
musculoskeletal system, pelvic organs, and liver. Its
advantages include high soft tissue contrast resolution,
lack of ionising radiation, and the ability to employ of
liver-specific contrast agents.
In this retrospective study, we aimed to investigate the diagnostic abilities of conventional T2-weighted imaging (T2WI) sequences and DWI to distinguish between
benign and malignant liver lesions and to compare the
diagnostic efficiency of the two examinations.
METHODS
Patients
In the present study, cases with liver lesions were retrieved retrospectively from abdominal MRI reports
taken in Health Sciences University, Haseki Training
and Research Hospital, Turkey between January 2014
and December 2014 using the hospital database. Cases
with no liver lesions, lesion size <1 cm, no T2WI or DWI
series, or images of unsuitable quality for evaluation
were excluded from the study. In cases with multiple
similar lesions, the largest lesion was considered as the
representative lesion and was evaluated. In addition,
benign regenerating nodules observed as hypointense
on T2WI sequences in cirrhotic liver patients were not
included in the evaluation.
In hepatocellular carcinoma cases, diagnosis was made by histopathological examination in 11 lesions, and by
typical imaging features (e.g., arterial hypervascular
lesion showing wash-out, mild hyperintense lesion in
T2W series, or nodule within a nodule), clinical and
laboratory findings (elevation of serum alpha fetoprotein)
and follow-up in 27 lesions. In cholangiocellular
carcinoma cases, diagnosis was made by histopathological
examination in five lesions, and by typical imaging
features (e.g., dilatation of the intrahepatic biliary tract,
retraction of the liver capsule, or infiltrative mass that
enhances towards the late phases), clinical and laboratory findings in one lesion. In metastatic cases, 49 lesions
were diagnosed by histopathological examination,
and 45 lesions were known malignancies and were
diagnosed with typical imaging features and follow-up
examinations. In benign cases, diagnosis of most
lesions was made by typical imaging features (e.g., T2W
markedly hyperintense lesions without enhancement for
simple parenchymal cysts or T2W hyperintense lesions
with flash filling or peripheral discontinuous nodular
enhancement for haemangiomas), clinical history, and
laboratory findings.
Magnetic Resonance Imaging
In our study, routine abdominal MRI was performed
using a 1.5T MRI device (Achieva; Philips Medical
Systems, Best, The Netherlands) and a 4-channel phased
array coil (SENSE body) directed to the abdomen. In
routine examination, T2WI in the axial and coronal
planes, fat-suppressed T2WI in the axial plane, DWI,
chemical shift imaging, unenhanced T1-weighted images
and dynamic axial contrast-enhanced T1-weighted
images were acquired.
In our centre, DWI is included in the routine abdominal MRI protocol. Before intravenous contrast agent
injection, DWI is acquired using a single-shot echoplanar
imaging sequence with parallel imaging technique in the
axial plane, (b: 0-50-500-1000 s/mm2) at the same level
and orientation as the routine sequences.
Image Analysis
The images were analysed on a PACS imaging
workstation (Infinitt PACS; Infinitt Healthcare, Seoul,
Korea) in a separate session, 2 months after the database
scan, in order to minimise memory bias. T2WI and DWI images were evaluated based on consensus by two
radiologists (ÖK with 15 years of abdominal radiology
experience, FÇ with 5 years of radiology experience),
who had no knowledge of clinical information or
pathologic diagnosis.
Lesions were evaluated according to the signal
characteristics on T2WI and DWI apparent diffusion
coefficient (ADC) maps at 3-week intervals (the same
lesion was evaluated in all sessions in cases with
multiple lesions), using a scoring system between 1 and 5
(Table 1, Figures 1 2 3). Sensitivity, specificity and
accuracy were calculated for T2WI and DWI.
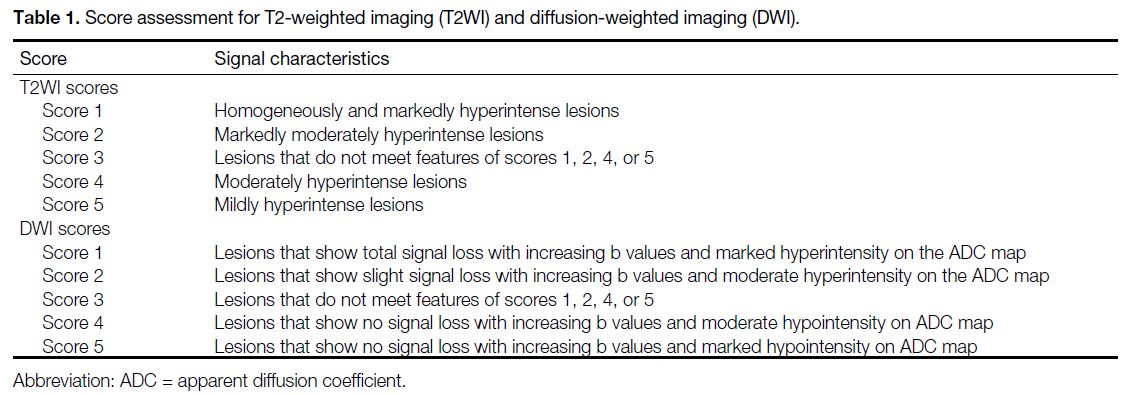
Table 1. Score assessment for T2-weighted imaging (T2WI) and diffusion-weighted imaging (DWI)
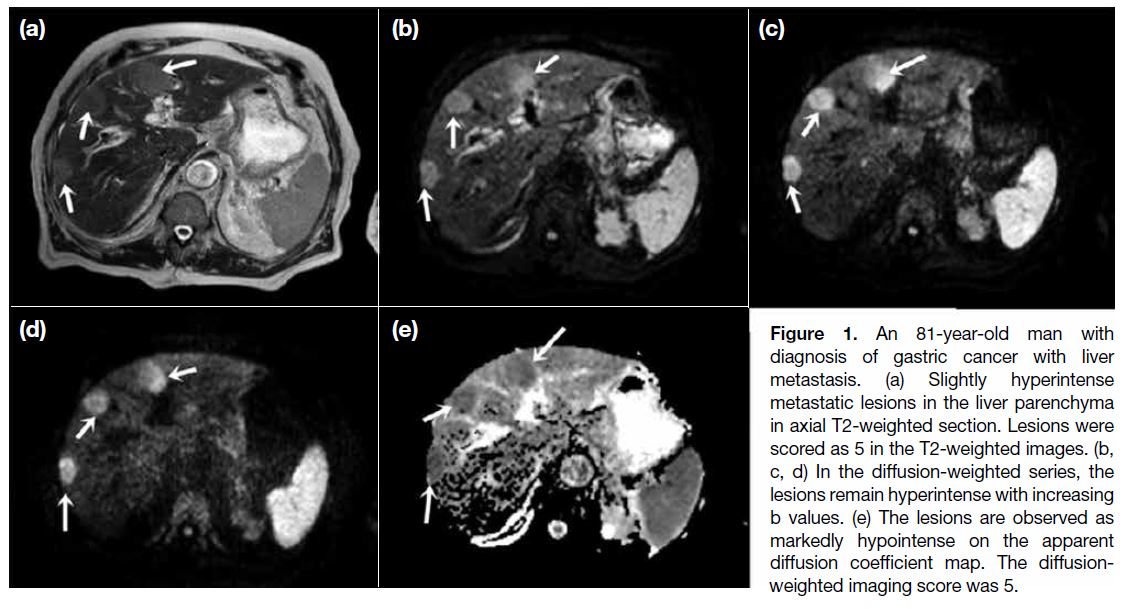
Figure 1. An 81-year-old man with
diagnosis of gastric cancer with liver
metastasis. (a) Slightly hyperintense
metastatic lesions in the liver parenchyma
in axial T2-weighted section. Lesions were
scored as 5 in the T2-weighted images. (b,
c, d) In the diffusion-weighted series, the
lesions remain hyperintense with increasing
b values. (e) The lesions are observed as
markedly hypointense on the apparent
diffusion coefficient map. The diffusion-weighted
imaging score was 5.
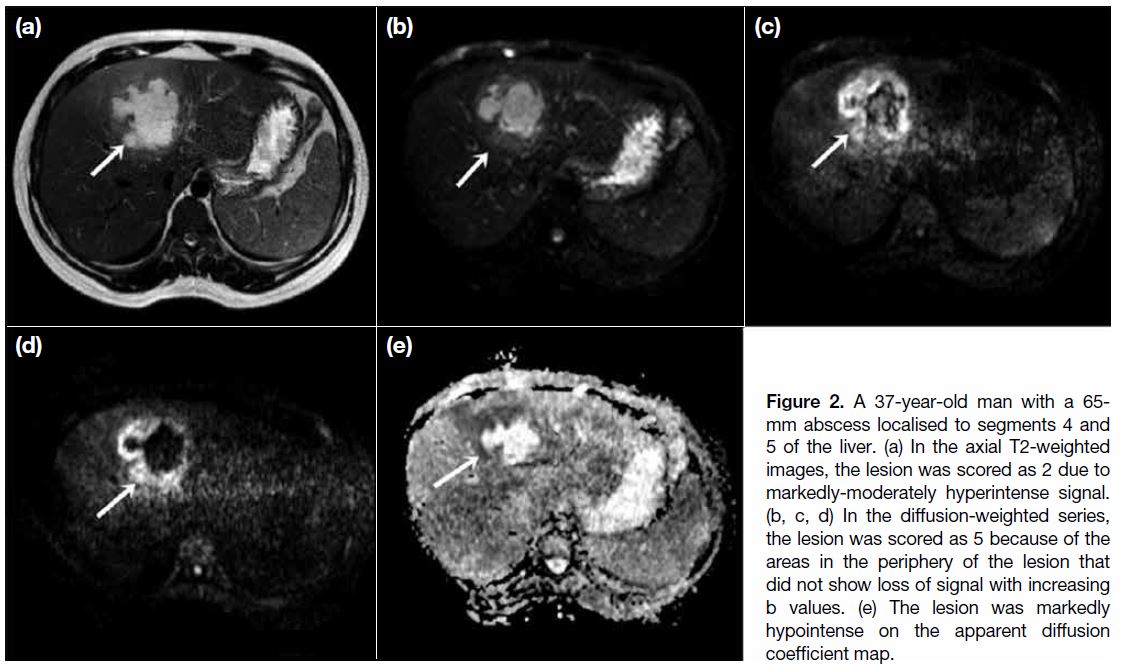
Figure 2. A 37-year-old man with a 65-mm abscess localised to segments 4 and
5 of the liver. (a) In the axial T2-weighted
images, the lesion was scored as 2 due to
markedly-moderately hyperintense signal.
(b, c, d) In the diffusion-weighted series,
the lesion was scored as 5 because of the
areas in the periphery of the lesion that
did not show loss of signal with increasing
b values. (e) The lesion was markedly
hypointense on the apparent diffusion
coefficient map.
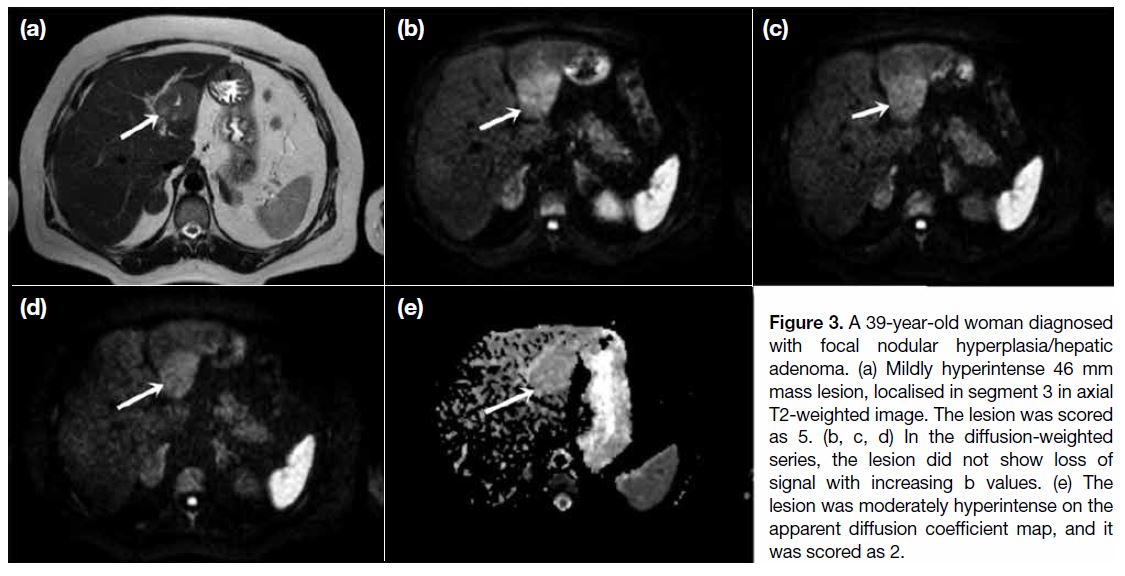
Figure 3. A 39-year-old woman diagnosed
with focal nodular hyperplasia/hepatic
adenoma. (a) Mildly hyperintense 46 mm
mass lesion, localised in segment 3 in axial
T2-weighted image. The lesion was scored
as 5. (b, c, d) In the diffusion-weighted
series, the lesion did not show loss of
signal with increasing b values. (e) The
lesion was moderately hyperintense on the
apparent diffusion coefficient map, and it
was scored as 2.
Statistical Analyses
All statistical analyses were made using commercial
software (SPSS, Windows version 15.0; SPSS Inc.,
Chicago [IL], United States). The data are presented as
mean ± standard deviation, medians (range), minimum,
maximum, frequency, and percentages. The diagnostic
value of T2WI and DWI in distinguishing benign from
malignant liver lesions was evaluated using a two-sample
t test and the Chi-square test for continuous and
discrete variables, respectively. Fisher’s exact test was
used instead of the Chi-square test in small samples
of data. A p value <0.05 was considered statistically
significant.
RESULTS
In total, 3523 cases with liver lesions between January 2014 and December 2014 were extracted from hospital
records. Cases were excluded if they had no liver lesions
(n=2791), lesion size of <1 cm (n=130), no T2WI or DWI
series, or images of unsuitable quality for evaluation
(n=28). Patients were also excluded from the study who had previously undergone surgical/interventional
treatment, chemotherapy, or radiotherapy (n=13).
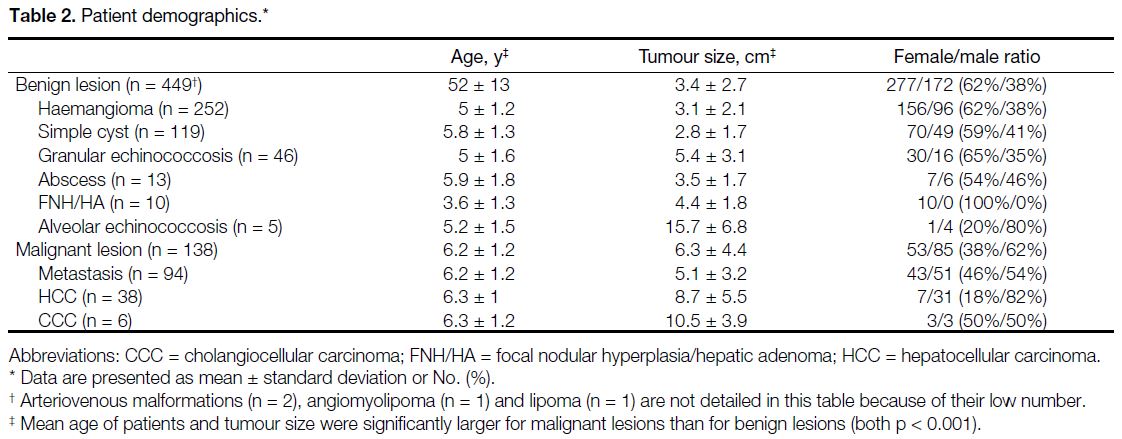
In total, 587 focal liver lesions in 561 patients (315 female, 56%; 246 male, 44%) aged 54.55 ± 13.68 years (range, 11-95 years) were included in the study (Table 2).
Table 2. Patient demographics
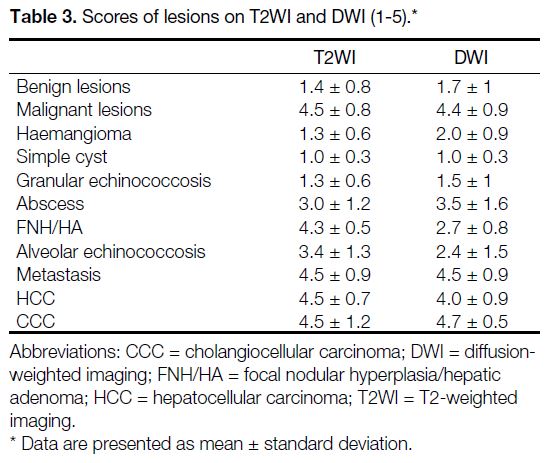
In the characterisation of benign lesions, the mean scores in T2WI and DWI were 1.4 ± 0.8 and 1.7 ± 1.0, respectively. The scores in malignant lesions were
4.5 ± 0.8 and 4.4 ± 0.9 (Table 3).
Table 3. Scores of lesions on T2WI and DWI (1-5).
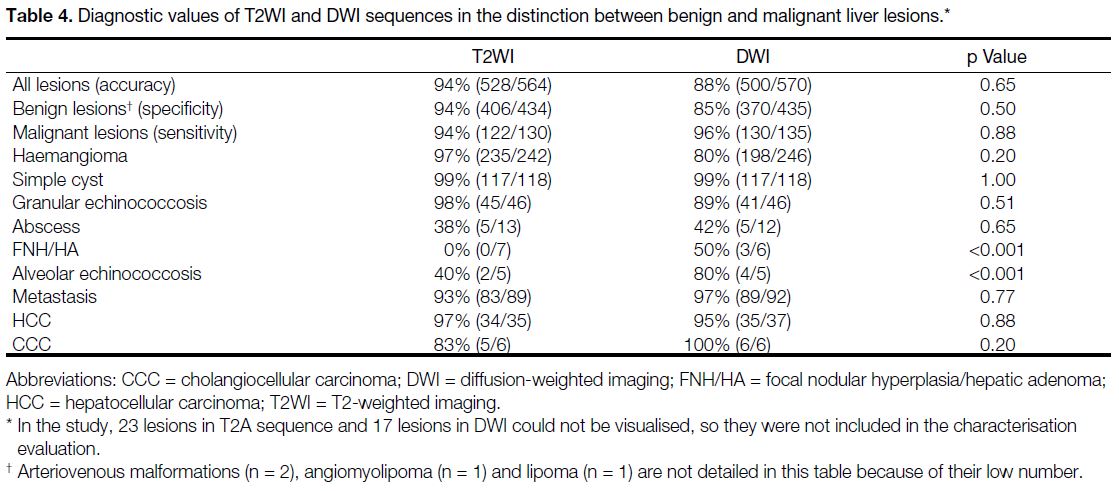
The sensitivity, specificity, and accuracy of T2WI in distinguishing between benign and malignant liver
lesions were 94%, 94%, and 94%, respectively. The
values for DWI were 96%, 85% and 88% respectively
(Table 4).
Table 4. Diagnostic values of T2WI and DWI sequences in the distinction between benign and malignant liver lesions
A total of 23 lesions in T2WI sequence and 17 lesions in DWI could not be visualised; they were not included in the accuracy evaluation. Among these lesions, 11 lesions
could not be visualised in both T2W sequence and DWI
images. Nine lesions on T2W images and 42 lesions on
DWI images were scored as 3. Lesions scoring 3 were
evaluated as incorrect reading.
DISCUSSION
Focal liver masses have a wide pathological spectrum from benign lesions to aggressive malignancies, and
characterisation of lesions is key. Today, the detection of
liver lesions is increasing in parallel with the increasing use of imaging methods such as US, CT, and MRI. MRI,
which does not expose patients to ionising radiation,
provides a high level of lesion/liver contrast, and with
hepatocyte-specific contrast agent option is considered
to be the most successful radiological diagnostic method
that can be used in the detection and characterisation of
focal liver lesions.[5] [6]
Developments in parallel imaging techniques have
provided an increase in image quality of DWI, a
shortening of scanning time and a decrease in artefacts.
These have enabled the DWI to be used in abdominal
imaging.[4] [5] There are studies with positive results where
DWI was used in the detection of liver lesions and ADC
measurement in lesion characterisation.[7] [8] However, use of DWI in the characterisation of liver lesions is still controversial due to overlap in findings in different types
of lesions.[6] [7] [8] [9] [10] [11] [12] [13] [14] [15] [16]
T2WI is used in routine abdominal MRI protocols and
is very useful in the diagnosis of focal lesions in the
cirrhotic and non-cirrhotic liver.[17] [18] [19] However, it has
some limitations such as difficulty in distinguishing
between vascular structures and lesions, and in
detecting small lesions.[14] DWI was found to be
more successful than T2WI in detecting malignant
lesions when evaluated using lower b values (b:0 and
50 s/mm2).[14] [15] [16] [20] Higher success of DWI in detecting
lesions was attributed to the better contrast-to-noise ratio,
and suppression of signals originating from surrounding
vascular structures.[5] [14] Although high b values
(>500 s/mm2) can be disadvantageous in lesion detection
due to artefacts and low signal-to-noise ratio, they
contribute positively to lesion characterisation.[20]
Although measuring ADC in DWI is beneficial in
terms of lesion characterisation, it has no practical
consequence, especially in busy centres such as our
clinic. Also, there are wide overlaps in benign-malignant
lesions and problems arise on where to take the ADC
measurement in heterogeneous lesions. In this study, we
reached an accuracy rate of 88% with visual evaluation of
DWI in liver lesion characterisation. To our knowledge,
there are limited studies in the English-language
literature comparing DWI and T2WI MRI sequences
in the characterisation of liver lesions by direct visual
evaluation.[14] [20]
In this study, the sensitivity, specificity and accuracy rates of T2WI and DWI in the characterisation of liver lesions were 94%/96%, 94%/85%, and 94%/88%, respectively,
with no statistically significant difference between the
two sequences. However, in light of these data, the
specificity of T2WI was found to be higher compared
to DWI in lesion characterisation. This was due to the
fact that the T2W sequence had a high specificity rate
of 97% in benign lesions, especially in haemangiomas.
The fact that some haemangiomas showed increased
signal intensity with increasing b values and contained
hypointense areas in ADC (probably due to thrombus
content in some haemangiomas and a fibrous tissue
component in hyalinised haemangiomas) resulted
in some haemangiomas receiving malignant scores,
which decreased the specificity of DWI to 80%.
In a study conducted by Parikh et al,[14] sensitivity,
specificity, and accuracy rates of T2WI and DWI in
lesion characterisation were 92%/92%, 80%/83%, and
87%/89%, respectively. In a study performed by Yang
et al,[20] the same values were calculated as 97%/97%,
86%/88%, and 91%/91%, respectively. Although the
values largely overlap, the specificity values of the
T2WI were better in our study. This high specificity
value was thought to be due to the higher percentage of
haemangiomas in our study compared to the other two
studies.
In this study, T2WI was found to have higher accuracy
rates in cases of haemangioma (97% vs. 80%), whereas
DWI had higher accuracy rates in focal nodular
hyperplasia/hepatic adenoma (FNH/HA, 0% vs. 50%)
and alveolar echinococcosis (40% vs. 80%). In FNH/HA cases, the lesion shows a slightly hyperintense
signal intensity on T2WI that can be barely discerned
from the surrounding liver parenchyma, and as found
in other studies[21] [22] these cases can be confused with
malignant lesions due to low ADC values on DWI,
which decreased the diagnostic value of these sequences
in lesion characterisation.
Abscess, FNH/HA, and alveolar echinococcosis cases are benign lesions that can be mistaken for malignant liver
lesions in both sequences. In alveolar echinococcosis
cases, the DWI value in lesion characterisation was
significantly lower compared to other cystic liver lesions
and overlapped with malignant lesions. This was thought
to be due to the presence of chronic fibroinflammatory,
necrotic tissue and a solid component with diffusion
restriction.[23] Similar reasons and calcified areas cause
the signal to decrease in T2WI, and infiltrative extension to surrounding tissues, as in malignant lesions resulted
in the lesion to receive a malignant score in T2WI. The
accuracy rates of T2WI and DWI in abscess cases were
found to be 38% and 42%, respectively. In these cases,
the diffusion restriction due to abscess content[22] [24] and
the mild hyperintense signal areas in T2WI due to its
heterogeneous content resulted in malignant scores
and significantly decreased the accuracy rates of both
sequences.
Benign and malignant focal liver lesions can be
distinguished by measuring ADC in DWI. Although
there were overlaps, the ADC value of malignant liver
lesions was found to be significantly lower compared
to that of benign lesions. The threshold ADC values for
differentiation vary in different studies depending on the
MRI parameters used and the strength of the diffusion
gradient.[8] [10] [14] [16] [25] [26] [27] According to the literature, there is
a significant overlap between hypercellular benign liver
lesions such as FNH/HA and malignant liver lesions
such as hepatocellular carcinoma and metastases.[28] In
this study, measurements made with ADC in lesion
characterisation had results similar to those of visual
evaluation.
Most benign liver lesions are asymptomatic and are detected predominantly in middle-aged women.[29] In this
study, a significant difference was found between the
patient groups with benign and malignant liver masses in
terms of age and sex. The mean age of patients and size of
malignant lesions were found to be significantly greater
than those of benign lesions. Benign lesions were mostly
seen in women and malignant lesions were mostly seen
in men. In addition, although it is a benign lesion, the
size in alveolar echinococcosis cases overlapped with
that of malignant lesions.
This study has some limitations. First, interobserver variability was not calculated because the observers did not evaluate the cases independently. Second, there were
pathologically unconfirmed lesions in the present study.
However, we think that the misdiagnosis rate is very low
as a result of careful evaluation of other MR sequences
and contrast-enhanced images and evaluation of all
examinations in the system.
CONCLUSION
In conclusion, although both imaging methods had high efficiency in the characterisation of benign and malignant
liver lesions, it was found that conventional T2WI had
higher specificity and accuracy rates compared to DWI.
In addition, T2WI was more successful in haemangioma cases, whereas DWI was marginally more successful
in FNH/HA and alveolar echinococcosis cases. Both
sequences had low success rates in abscess, FNH/HA,
and alveolar echinococcosis cases. We think that T2WI
and DWI can be used safely for characterisation of
lesions in individuals who cannot be given contrast due
to reasons such as renal failure and contrast allergy.
REFERENCES
1. Taouli B, Koh DM. Diffusion-weighted MR imaging of the liver.
Radiology. 2010;254:47-66. Crossref
2. Thoeny HC, De Keyzer F, Chen F, Ni Y, Landuyt W, Verbeken EK,
et al. Diffusion-weighted MR imaging in monitoring the effect of a
vascular targeting agent on rhabdomyosarcoma in rats. Radiology.
2005;234:756-64. Crossref
3. Dzik-Jurasz A, Domenig C, George M, Wolber J, Padhani A,
Brown G, et al. Diffusion MRI for prediction of response of rectal
cancer to chemoradiation. Lancet. 2002;360:307-8. Crossref
4. Qayyum A. Diffusion-weighted imaging in the abdomen and pelvis:
concepts and applications. Radiographics. 2009;29:1797-810. Crossref
5. Nasu K, Kuroki Y, Nawano S, Kuroki S, Tsukamoto T, Yamamoto S,
et al. Hepatic metastases: diffusion-weighted sensitivity-encoding
versus SPIO-enhanced MR imaging. Radiology. 2006;239:122-30. Crossref
6. Dilek O, Gulek B, Yilmaz C, Kaya O, Soker G, Akin MA. The
comparison of the efficacy of diffusion weighted imaging (DWI)
sequences with 3 different T2-weighted sequences in the detection
of focal liver lesions. Acta Gastroenterol Belg. 2019;82:267-72.
7. Li J, Yang Y. Clinical study of diffusion-weighted imaging in the
diagnosis of liver focal lesion. J Med Syst. 2019;43:43. Crossref
8. Calistri L, Castellani A, Matteuzzi B, Mazzoni E, Pradella S,
Colagrande S. Focal liver lesions classification and characterization:
what value do DWI and ADC have? J Comput Assist Tomogr.
2016;40:701-8. Crossref
9. Caro-Domínguez P, Gupta AA, Chavhan GB. Can diffusion-weighted
imaging distinguish between benign and malignant
pediatric liver tumors? Pediatr Radiol. 2018;48:85-93. Crossref
10. Taouli B, Vilgrain V, Dumont E, Daire JL, Fan B, Menu Y.
Evaluation of liver diffusion isotropy and characterization of
focal hepatic lesions with two single-shot echo-planar MR
imaging sequences: prospective study in 66 patients. Radiology.
2003;226:71-8. Crossref
11. Ichikawa T, Haradome H, Hachiya J, Nitatori T, Araki T. Diffusionweighted
MR imaging with a single-shot echoplanar sequence:
detection and characterization of focal hepatic lesions. AJR Am J
Roentgenol. 1998;170:397-402. Crossref
12. Moteki T, Horikoshi H. Evaluation of hepatic lesions and hepatic
parenchyma using diffusion-weighted echo-planar MR with three
values of gradient b-factor. J Magn Reson Imaging. 2006;24:637-45. Crossref
13. Moteki T, Sekine T. Echo Planar MR imaging of the liver: comparison of images with and without motion probing gradients. J Magn Reson Imaging. 2004;19:82-90. Crossref
14. Parikh T, Drew SJ, Lee VS, Wong S, Hecht EM, Babb JS, et al.
Focal liver lesion detection and characterization with diffusion-weighted MR imaging: comparison with standard breath-hold
T2-weighted imaging. Radiology. 2008;246:812-22. Crossref
15. Bruegel M, Gaa J, Waldt S, Woertler K, Holzapfel K, Kiefer B, et al.
Diagnosis of hepatic metastasis: comparison of respiration-triggered diffusion-weighted echo-planar MRI and five T2-weighted turbo spin-echo sequences AJR Am J Roentgenol. 2008;191:1421-9. Crossref
16. Bruegel M, Holzapfel K, Gaa J, Woertler K, Waldt S, Kiefer B, et al.
Characterization of focal liver lesions by ADC measurements using
a respiratory triggered diffusion-weighted single-shot echo-planar
MR imaging technique. Eur Radiol. 2008;18:477-85. Crossref
17. Soyer P, De Givry SC, Gueye C, Lenormand S, Somveille E, Scherrer A. Detection of focal hepatic lesions with MR imaging: prospective comparison of T2-weighted fast spin-echo with and without fat suppression, T2-weighted breath-hold fast spin-echo, and gadolinium chelate–enhanced 3D gradient-recalled imaging. AJR Am J Roentgenol. 1996;166:1115-21. Crossref
18. Soyer P, Gouhiri M, Rondeau Y, Spelle L, Mosnier H, Scherrer A.
Non-breath-hold fast spin-echo versus breath-hold fast spin-echo
and spoiled gradient-recalled echo MR imaging in the detection
of hepatic tumors: correlation with surgical findings. AJR Am J
Roentgenol. 1997;168:1199-204. Crossref
19. Pawluk RS, Tummala S, Brown JJ, Borrello JA. A retrospective
analysis of the accuracy of T2-weighted images and dynamic
gadolinium-enhanced sequences in the detection and characterization
of focal hepatic lesions. J Magn Reson Imaging. 1999;9:266-73. Crossref
20. Yang DM, Jahng GH, Kim HC, Jin W, Ryu CW, Nam DH, et al.
The detection and discrimination of malignant and benign focal
hepatic lesions: T2 weighted vs. diffusion-weighted MRI. Br J
Radiol. 2011;84:319-26. Crossref
21. Agnello F, Ronot M, Valla DC, Sinkus R, Van Beers BE, Vilgrain V.
High-b-value diffusion-weighted MR imaging of benign
hepatocellular lesions: quantitative and qualitative analysis.
Radiology. 2012;262:511-9. Crossref
22. Kanematsu M, Goshima S, Watanabe H, Kondo H, Kawada H, Noda Y, et al. Detection and characterization of focal hepatic lesions with diffusion-weighted MR imaging: a pictorial review. Abdom Imaging. 2013;38:297-308. Crossref
23. Becce F, Pomoni A, Uldry E, Halkic N, Yan P, Meuli R, et al.
Alveolar echinococcosis of the liver: diffusion-weighted MRI
findings and potential role in lesion characterisation. Eur J Radiol. 2014;83:625-31. Crossref
24. Demir OI, Obuz F, Sağol O, Dicle O. Contribution of diffusion-weighted
MRI to the differential diagnosis of hepatic masses. Diagn
Interv Radiol. 2007;13:81-6.
25. Miller FH, Hammond N, Siddiqi AJ, Shroff S, Khatri G, Wang Y, et al.
Utility of diffusion-weighted MRI in distinguishing benign and
malignant hepatic lesions. J Magn Reson Imaging. 2010;32:138-47. Crossref
26. Yamada I, Aung W, Himeno Y, Nakagawa T, Shibuya H. Diffusion
coefficients in abdominal organs and hepatic lesions: evaluation
with intravoxel incoherent motion echo-planar MR imaging.
Radiology. 1999;210:617-23. Crossref
27. Gourtsoyianni S, Papanikolaou N, Yarmenitis S, Maris T,
Karantanas A, Gourtsoyiannis N. Respiratory gated diffusion-weighted imaging of the liver: value of apparent diffusion
coefficient measurements in the differentiation between most
commonly encountered benign and malignant focal liver lesions.
Eur Radiol. 2008;18:486-92. Crossref
28. Chandarana H, Taouli B. Diffusion and perfusion imaging of the
liver. Eur J Radiol 2010;76:348-58. Crossref
29. Terkivatan T, Hussain SM, De Man RA, Ijzermans JN. Diagnosis and treatment of benign focal liver lesions. Scand J Gastroenterol Suppl. 2006;243:102-15. Crossref