Ruptured Ectopic Pregnancy after Previous Hysterectomy: a Case Report
CASE REPORT
Ruptured Ectopic Pregnancy after Previous Hysterectomy: a Case Report
YY Man, YN Tam
Department of Radiology, North District Hospital, Hong Kong
Correspondence: Dr YY Man, Department of Radiology, North District Hospital, Hong Kong. Email: manyan93@connect.hku.hk
Submitted: 20 Oct 2020; Accepted: 23 Dec 2020
Contributors: YYM and YNT designed the study. YYM acquired the data, analysed the data, drafted the manuscript, and critically revised the
manuscript for important intellectual content. YNT provided administrative, technical, and material support. Both authors had full access to the
data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of Interest: All authors have disclosed no conflicts of interest.
Funding/Support: This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data Availability: All data generated or analysed during the present study are available from the corresponding author on reasonable request.
Ethics Approval: The patient was treated in accordance with the tenets of the Declaration of Helsinki. Informed verbal consent was obtained via
telephone contact due to COVID-19 restrictions.
INTRODUCTION
Pregnancy-associated complications would not usually
be considered among differential diagnoses in a patient
with a previous history of hysterectomy. Nonetheless
such cases are not rare and may include ruptured ectopic
pregnancy.
CASE REPORT
A 41-year-old woman presented to the emergency
department with lower abdominal pain and hypotension.
She had a history of previous emergency Caesarean
section 1 year previously with subsequent abdominal
hysterectomy including the posterior lip of cervix
secondary to severe pre-eclampsia and placenta accreta.
She had no bowel or urinary symptoms and no per-vaginal
bleeding. A pregnancy test was carried out and
was positive. Bedside ultrasonography in the emergency
department showed free fluid in Morrison’s pouch.
A gynaecologist was consulted and urgent computed
tomography (CT) scan performed.
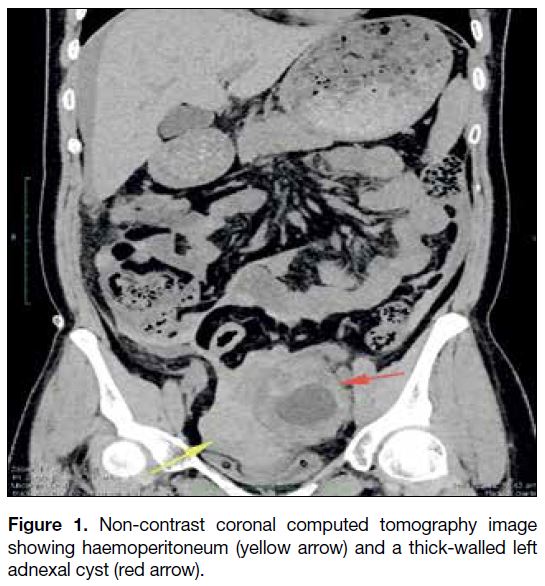
Review of CT revealed moderate haemoperitoneum
with a thick-walled cystic mass over the left adnexal region (Figure 1). The mass was highly vascular with
feeding vessels from the left ovarian artery. No product of gestation was evident inside the mass and no sentinel
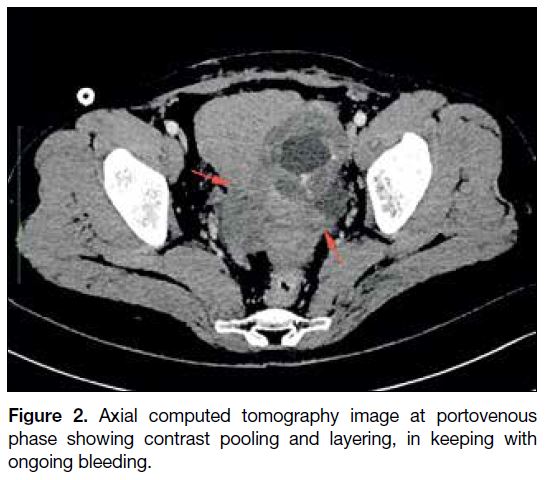
bleeding site was identified but contrast pooling with
layering was noted at the pelvis, suggestive of active
bleeding (Figure 2). Other gastrointestinal structures and
the urinary tract were unremarkable. The provisional
diagnosis was bleeding ovarian tumour.
Figure 1. Non-contrast coronal computed tomography image
showing haemoperitoneum (yellow arrow) and a thick-walled left
adnexal cyst (red arrow).
Figure 2. Axial computed tomography image at portovenous
phase showing contrast pooling and layering, in keeping with
ongoing bleeding.
Emergency laparoscopic surgery was performed a few
hours later. Intra-operatively, an 8-cm left adnexal mass
with active bleeding from a 1-cm rupture site was noted.
No normal left ovarian tissue could be identified and
left salpingo-oophorectomy was performed. A normal left ovary and 1.5-cm fetal pole were seen inside the left
adnexal mass. A diagnosis of ruptured ectopic pregnancy
was thus confidently made and tubal pregnancy
confirmed by pathology.
DISCUSSION
Given the history of previous hysterectomy, the
possibility of ectopic pregnancy was not considered.
Nonetheless with the finding of free intraperitoneal
fluid, lack of trauma history and positive pregnancy
test, this possibility should not have been excluded.
Ultrasonography is readily available with the advantages
of being real-time and equipped with Doppler function,
facilitating the diagnosis of ectopic pregnancy.
Ultrasonography of the pelvis in this patient enabled
detection of the thick-walled left adnexal cystic lesion.
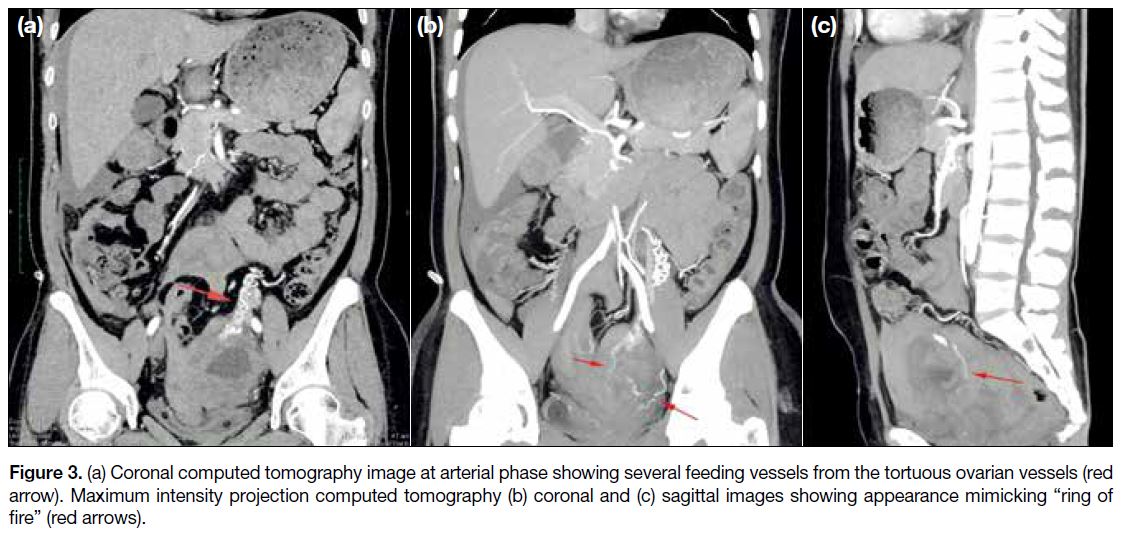
Ectopic pregnancy would be subsequently diagnosed if
there was a heartbeat suggesting a viable fetus within the
lesion or ‘ring of fire’ appearance around the lesion with
low resistance flow (Figure 3). Although ultrasonography
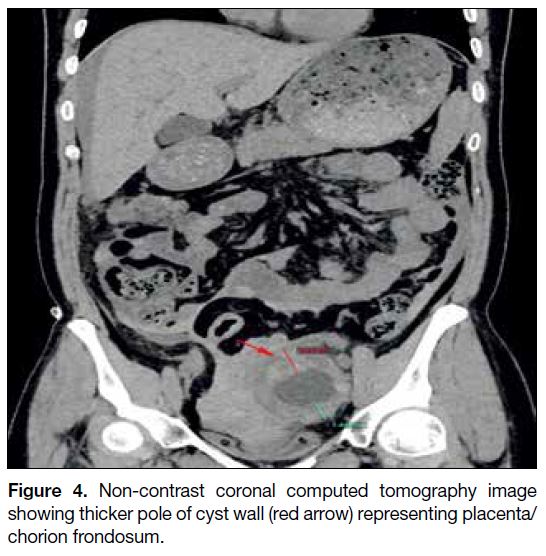
is superior to CT in diagnosing pregnancy, the thicker
pole of the cyst wall that was evident on CT is suggestive
of pregnancy, representing the placenta/chorion
frondosum,[1] as shown on Figure 4.
Figure 3. (a) Coronal computed tomography image at arterial phase showing several feeding vessels from the tortuous ovarian vessels (red
arrow). Maximum intensity projection computed tomography (b) coronal and (c) sagittal images showing appearance mimicking “ring of
fire” (red arrows).
Figure 4. Non-contrast coronal computed tomography image
showing thicker pole of cyst wall (red arrow) representing placenta/chorion frondosum.
Some studies have demonstrated a higher rate of
vaginal-to-peritoneum tract formation for Caesarean
hysterectomy,[2] [3] [4] [5] as in our patient. Cervical dilatation
at the time of Caesarean section often results in a
remnant of cervix or larger vaginal vault that increases the probability of communication between the vagina
and peritoneum with consequent creation of a possible pathway for fertilisation. To prevent this, the residual
cervical canal should be obliterated or isolated surgically.
CONCLUSION
With proper ultrasonography, early diagnosis of ectopic
pregnancy in patients with prior hysterectomy can be
made. This will enable early surgical intervention to save
patients who are often young and otherwise healthy.
REFERENCES
1. Shin DS, Poder L, Courtier J, Naeger DM, Westphalen AC,
Coakley FV. CT and MRI of early intrauterine pregnancy. AJR
Am J Roentgenol. 2011;196:325-30. Crossref
2. Barhate KP, Domkundwar S, Patil N, Pai B. Sonographic diagnosis
of ectopic pregnancy 2 years after total hysterectomy, J Clin
Ultrasound. 2009;37:347-9. Crossref
3. Anupama R, Beegum TR, Indu RN. Ruptured ectopic pregnancy 11
years after supracervical hysterectomy: a case report. Eur J Obstet
Gynecol Reprod Biol. 2012;162:116-7. Crossref
4. Villegas E, González-Mesa E, Benítez MJ, Luna S, Gómez C,
Marsac A, et al. Tubal ectopic pregnancy two years after
laparoscopic supracervical hysterectomy. BMC Womens Health.
2014;14:69. Crossref
5. Fylstra DL. Ectopic pregnancy after hysterectomy may not be so
uncommon: a case report and review of the literature. Case Rep
Womens Health. 2015;7:8-11. Crossref