Location of the Internal Mammary Arteries in Relation to the Lateral Border of the Sternum: A Key to Avoid Injury during Computed Tomography-Guided Biopsy of Anterior Mediastinal Masses
ORIGINAL ARTICLE
Location of the Internal Mammary Arteries in Relation to the Lateral Border of the Sternum: A Key to Avoid Injury during Computed Tomography-Guided Biopsy of Anterior Mediastinal
Masses
PR Gurijala1, GE Punnen1, T Mani2, SN Keshava3
1 Department of Radiology, Division of Clinical Radiology, Christian Medical College, Vellore, India
2 Department of Biostatistics, Christian Medical College, Vellore, India
3 Department of Interventional Radiology, Division of Clinical Radiology, Christian Medical College, Vellore,
India
Correspondence: Prof SN Keshava, Department of Interventional Radiology, Division of Clinical Radiology, Christian Medical College, Vellore, India. Email: shyamkumar.n.keshava@gmail.com
Submitted: 21 Sep 2020; Accepted: 7 Dec 2020.
Contributors: All authors designed the study. PRG acquired the data. PRG, GEP and TM analysed the data. All authors drafted the manuscript
and critically revised the manuscript. All authors had full access to the data, contributed to the study, approved the final version for publication,
and take responsibility for its accuracy and integrity.
Conflicts of Interest: All authors have disclosed no conflicts of interest.
Funding/Support: This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors
Data Availability: All data generated or analysed during the present study are available from the corresponding author on reasonable request.
Ethics Approval: This study was approved by our Institutional Review Board (Ref: 12734). The need for consent was waived off in view of the retrospective nature of the study.
Abstract
Introduction
Accurate knowledge of the location of the internal mammary arteries (IMAs) in relation to the lateral
border of the sternum is important in preventing haemorrhagic complications during biopsy of anterior mediastinal
masses using an anterior parasternal approach. This study aimed to document the location of the IMAs in relation
to the sternum and their course to guide parasternal transthoracic interventions.
Methods
The shortest distance between each IMA and the sternum midway between the main pulmonary artery and
the aortic arch was measured on axial sections of contrast-enhanced chest computed tomography of 150 adult patients.
Results
The mean distance of the right IMA from the lateral border of the sternum was 11.7 ± 2.51 mm and that of
the left IMA was 10.88 ± 2.41 mm.
Conclusion
Our study established the position of the IMAs in relation to the sternum’s lateral border in the Indian
population. This knowledge is useful in planning percutaneous anterior mediastinal biopsies without injuring the
IMA. We recommend a parasternal approach with a safe window of 11.3 mm between the lateralmost margin of
the sternum and the medial margin of the IMA for percutaneous transthoracic anterior mediastinal procedures.
Key Words: Image-guided biopsy; Mammary arteries; Needles; Supine position
中文摘要
內乳動脈相對於胸骨外側緣的位置:計算機斷層掃描引導前縱隔腫塊活檢過程中避免損傷的關鍵
PR Gurijala、GE Punnen、T Mani、SN Keshava
引言
準確了解內乳動脈(IMA)相對於胸骨外側緣的位置對於預防前胸骨旁入路對前縱隔腫塊進行活檢時出現出血併發症非常重要。本研究旨在記錄IMA相對於胸骨位置及其路線,以指導胸骨旁經胸介入。
方法
在150名成人患者的胸部計算機斷層掃描增強掃描的軸向切面圖像上,測量主肺動脈和主動脈弓中間的胸骨與每個IMA之間的最短距離。
結果
右側IMA距胸骨外側緣的平均距離為11.7 ± 2.51 mm,左側IMA平均距離為10.88 ± 2.41 mm。
結論
本研究確定印度人口中IMA相對於胸骨外側緣的位置。這些知識有助於在不損傷IMA的情況下規劃經皮前縱隔活檢。對於經皮經胸前縱隔手術,我們推薦胸骨最外側邊緣和IMA內側邊緣之間的安全窗為11.3 mm的胸骨旁入路。
INTRODUCTION
Biopsy of anterior mediastinal masses using a
parasternal approach under both computed tomographic
(CT) and ultrasonic guidance is widely practised.[1] [2]
CT-guided percutaneous biopsy of anterior mediastinal
masses is considered a safe diagnostic procedure
with a high diagnostic yield.[3] [4] [5] [6] [7] The course of the left
internal mammary artery (LIMA) and the right internal
mammary artery (RIMA) adjacent to the sternum makes
them susceptible to iatrogenic injury during anterior
parasternal transthoracic procedures, which can lead
to life-threatening haemorrhage.[8] Knowledge of the
location of the IMAs in relation to the lateral border of the
sternum is key in planning biopsy of anterior mediastinal
masses using the parasternal approach.
Anatomical Considerations: Does the
Location Matter?
As the IMAs (usually the LIMA) are the primary conduit
used for coronary artery bypass grafts, there are many
cadaveric studies that have generated information on
their anatomy.[9] [10] [11]
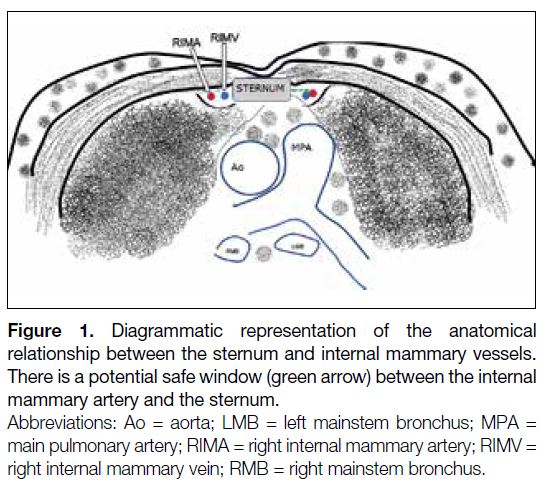
The IMA originates from the first part of the subclavian
artery and descends along the posterior aspect of the first
to sixth costal cartilages. Medial to the artery, there are
two internal mammary veins (IMVs), which variably
unite and drain into the brachiocephalic vein.[12] The IMA
and IMV are located approximately 1.3 cm from the lateral edge of the sternum on either side. Usually, the
IMA is situated lateral to the IMV (Figure 1). However,
studies have shown that the position of these vessels can
be variable and the lateral border to sternum to artery
distance can range from 0.42 to 1.66 cm for the IMV and
from 0.98 to 2.42 cm for the IMA.[12] [13] [14] Differences in the
points of measurement across studies (e.g., midpoint of
an IMA to the lateral border of the sternum or medial
border of an IMA to the lateral border of the sternum)
or different craniocaudal levels of measurement can contribute to the wide range of variations in the distance
from the lateral border of the sternum to the IMA.
Figure 1. Caption
Most of the studies contributing to the knowledge of the
anatomy of the internal mammary vessels are cadaveric.
The IMAs are easily demonstrated on CT.
This study aimed to document the shortest distance
between the IMAs and the sternum, and variations in
the number of IMAs, to prevent injury of these vessels
during percutaneous transthoracic procedures.
METHODS
The study was performed in a tertiary care referral
hospital. This study was approved by our Institutional
Review Board (IRB Ref: 12734). The need for consent
was waived in view of the retrospective nature of the
study. We performed a retrospective observational study
of 175 consecutive patients, who underwent contrast-enhanced
CT of the thorax for diverse indications such
as evaluation of lung opacities discovered on chest
radiography, primary or metastatic disease, or suspected
pulmonary infection/inflammatory conditions. Patients
aged <18 years or with conditions that distort the normal
anatomy, such as space-occupying lesions, major trauma,
malunited fractures, or congenital thoracic anomalies
were excluded. Twenty-five patients were excluded from
the study, based on the above criteria.
Technical Information
Computed Tomography Acquisition
Contrast-enhanced axial sections of the thorax in the
arterial phase were obtained on a 64-slice (GE Discovery
CT 750 HD scanner; GE Healthcare, Milwaukee [WI],
United States) or on a 32-slice CT scanner (Philips
Incisive CT; Philips Healthcare, Best, the Netherlands)
with a section thickness of 2.5 mm and an interslice gap
of 2.5 mm.
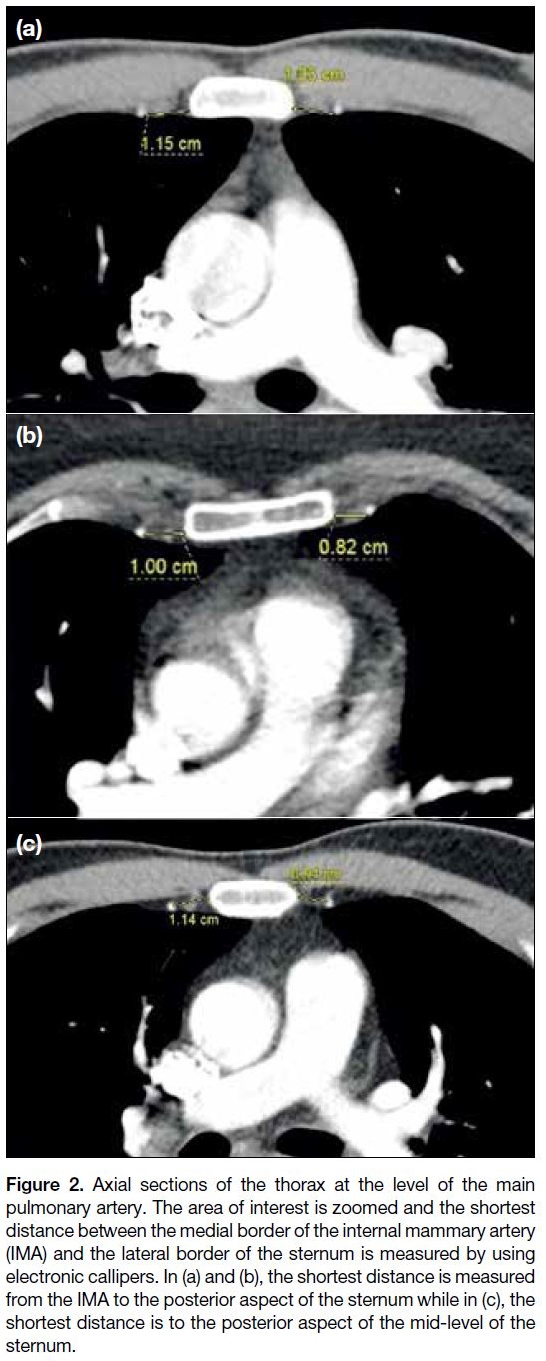
Measurement Methodology
The number of arteries visualised on either side of the
sternum was noted. The shortest distance between the
most medial IMA and the lateral border of the sternum
was measured at a level between the aortic arch and
the main pulmonary artery, which approximately
corresponds to the level of the tracheal bifurcation.
Electronic callipers were used to measure the shortest
distance between the sternum and the medial margin
of each IMA on either side on relevant magnified
axial sections. Measurement at the level of the costal
cartilages was avoided (Figure 2).
Figure 2. Caption
Statistical Analysis
Descriptive statistics were used such as mean ±
standard deviation for continuous variables. Number and proportion were used for categorical variables.
An independent Student’s t test was used to identify
significant differences in the IMA distance to the sternum
between sides and between sexes. p value < 0.05 was
considered significant. The analysis was carried out
using SPSS (version 21.0; IBM Corp, Armonk [NY],
United States).
RESULTS
There were 150 patients (300 sides) included for
evaluation of which 87 (58%) were men and 63 (42%)
were women. The patients were age 18 to 83 years (mean
age 48.4 ± 15.7; men: 49.7 ± 17.1; women: 46.6 ± 13.4).
A single IMA was noted on each side in all patients. The
mean distance between the IMA from the lateral border
of the sternum was 11.3 ± 2.49) mm. There was no
significant difference between the mean IMA distance of
men and that of women (p = 0.232).
The mean distance from the RIMA to the sternum was
11.7 ± 2.51 mm (range, 2.8-18.0) and from the LIMA
to the sternum was 10.88 ± 2.41 mm (range, 5.2-16.9)
[p = 0.003]. There was a significant difference among
men (p = 0.009) but not among women (p = 0.125) in
IMA distance to sternum between the two sides.
The mean distances between the IMA and sternum were
11.09 ± 2.79 mm in men and 11.45 ± 2.25 mm in women.
The mean distance from the RIMA to the sternum was
11.89 ± 2.24 mm (range, 5.9-17.1) for men and 11.47 ±
2.85 mm (range, 3.8-18.0) for women (p = 0.309). The
mean distance from the LIMA to the sternum was 11 ±
2.18 mm (range, 5.9-16.9) for men and 10.7 ± 2.69 mm
(range, 5.2-16.2) for women (p = 0.472).
We did not encounter any anatomical variants of the
IMA in our study.
DISCUSSION
Knowledge of the location of the IMAs helps to guide the
planning of the procedure, ensuring the trajectory of the
needle is such that the IMA is not along the needle path.
Inadvertent puncture of the IMA can occasionally result
in substantial extrapleural and pleural haemorrhage and
is potentially fatal.[8] The need to preserve the IMA also
lies in the fact that it is the most preferred vessel for
coronary artery bypass grafting.[11]
Although there are cadaveric studies that describe the
distance between the IMA and the lateral margin of the sternum, there are few imaging-based studies available.
Glassberg et al[14] in their study recommended that in
order to avoid IMA injury while performing parasternal
percutaneous transthoracic procedures, a more lateral
approach (2.5 cm from the sternal border) should be
adopted. They described the existence of a safe window
between the sternal border and the internal mammary
vessels and advocated its use only for procedures
performed under image guidance. However, the authors
did not specify the measurement technique, whether it
is measured from the anterior or posterior margin of
the sternum. Also, the study included patients between
5 years and 96 years, which could skew the results as the
younger population have smaller measurements given
their smaller chests. Dursun et al[1] measured the distances
between the IMA and the sternum at three different
levels (manubrium, midsternal corpus, and distal sternal
corpus) and found that the distance increased caudally.[1] [14]
However, these were done on coronal reformatted
images.
Karaman et al,[15] in their study on 164 patients with
CT angiography, measured the mean distance between
the lateral margin of the sternum and midpoint of the
RIMA and LIMA (13.0 mm and 12.4 mm, respectively).
However, we need the shortest distance between the
sternum and the medial margin of the IMA to facilitate
needle insertion without injury to the IMA. Iguchi et al[16]
reported a mean distance of 7.3 ± 2.4 mm between
the IMA and the lateral edge of the sternum, based on
their experience with biopsy of 42 anterior mediastinal
lesions.
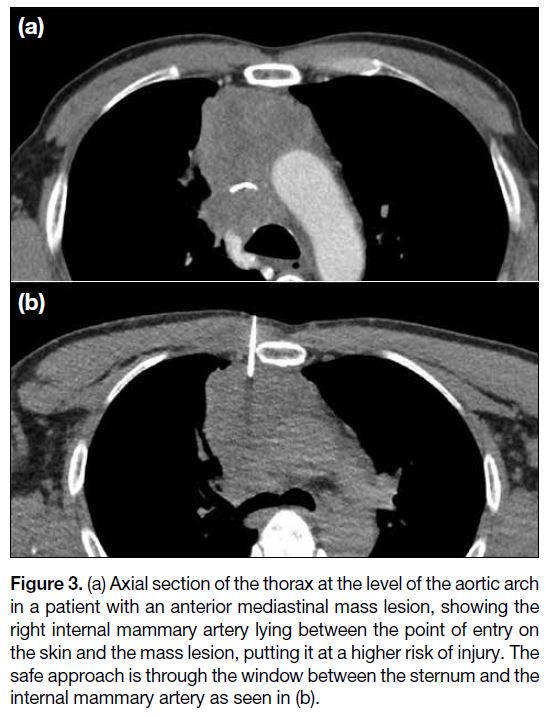
Our study revealed a mean distance of 11.3 ± 2.49 mm
between the lateralmost margin of the sternum and
the medial margin of the IMA. There exists a safe
window of 11.3 mm between them, which would be
sufficient to accommodate a coaxial needle under CT
guidance (Figure 3). The needle, when advanced close
to the sternum, allows the use of the sternum as a pivot
guiding further advancement, and also avoids the pleural
reflection, which lies more laterally, thereby preventing
complications such as pneumothorax and pleural
haemorrhage.
Figure 3. Caption
The knowledge of the relationship between the IMAs
and the lateral margin of sternum helps to plan safe
access to anterior mediastinal pathologies without injury
to the adjacent IMA and the pleural reflection, thereby
avoiding potentially life-threatening mediastinal and/or
pleural haemorrhage as well as pneumothorax.
Although the IMA can be identified on the non-contrast
planning CT, it may not always be possible to do so,
particularly in case of a large anterior mediastinal mass
reaching up to the chest wall, wherein the IMA may
not be visually separated from the mass. This study
establishes the position of the IMAs in relation to the
sternum’s lateral border and assures us that there will,
most often be adequate space available to pass a biopsy
needle.
There are no major limitations in this study. The distance between the IMAs and the sternum was measured
at one specific level. One needs to be aware that the
location of needle insertion for biopsy of a mediastinal
lesion depends on several factors, including the size of
the mediastinal mass, its location, intervening costal
cartilage, and any lung tissue in between. These factors
may limit a fixed location of entry of the biopsy needle.
This distance may vary slightly at different levels. We
did not encounter any anatomical variants in the number
of IMAs and hence the data are not applicable to patients
with anatomical variants. It is important to be aware
that the IMV lies medial to the IMA. To the extent possible, injury to the IMV is preferably avoided, though
it is not known to cause significant or life-threatening
haemorrhage.
In conclusion, this study establishes that there exists
a safe window of 11.3 mm between the IMA and the
lateral margin of the sternum for planning percutaneous
anterior mediastinal biopsies. With this background of
knowledge, the recommended route while planning an
image-guided biopsy for an anterior mediastinal lesion is
therefore medial to the IMA, which will avoid inadvertent
injury to the artery and prevent entry of the pleural
space, avoiding pleural haemorrhage and pneumothorax.
Although the safe window is established as 11.3 mm, the
least distance we encountered in our study was 5.9 mm
in men and 3.8 mm in women. Nevertheless, this study
emphasises the existence of a window between the
IMA and the sternum, wide enough to let a needle pass
through. One will look at the IMAs and IMVs anyway
before biopsy. However, the information obtained by
this study provides confidence regarding the potential
available space between the sternal border and the IMA.
REFERENCES
1. Dursun M, Yekeler E, Yilmaz S, Genchellac H, Tunaci M.
Mapping of internal mammary vessels by multidetector computed
tomography for parasternal transthoracic intervention guidance. J
Comput Assist Tomogr. 2005;29:617-20. Crossref
2. Rubens DJ, Strang JG, Fultz PJ, Gottlieb RH. Sonographic guidance
of mediastinal biopsy: an effective alternative to CT guidance. AJR
Am J Roentgenol. 1997;169:1605-10. Crossref
3. Petranovic M, Gilman MD, Muniappan A, Hasserjian RP,
Digumarthy SR, Muse VV, et al. Diagnostic yield of CT-guided
percutaneous transthoracic needle biopsy for diagnosis of anterior
mediastinal masses. AJR Am J Roentgenol. 2015;205:774-9. Crossref
4. Bressler EL, Kirkham JA. Mediastinal masses: alternative
approaches to CT-guided needle biopsy. Radiology. 1994;191:391-6. Crossref
5. Priola AM, Priola SM, Cataldi A, Ferrero B, Garofalo G, Errico L,
et al. CT-guided percutaneous transthoracic biopsy in the diagnosis
of mediastinal masses: evaluation of 73 procedures [in English,
Italian]. Radiol Med. 2008;113:3-15. Crossref
6. de Margerie-Mellon C, de Bazelaire C, Amorim S, Brice P,
Tazi A, Brière J, et al. Diagnostic yield and safety of computed
tomography–guided mediastinal core needle biopsies. J Thorac
Imaging. 2015;30:319-27.Crossref
7. Sklair-Levy M, Polliack A, Shaham D, Applbaum YH, Gillis S,
Ben-Yehuda D, et al. CT-guided core-needle biopsy in the diagnosis
of mediastinal lymphoma. Eur Radiol. 2000;10:714-8. Crossref
8. Glassberg RM, Sussman SK. Life-threatening hemorrhage due to
percutaneous transthoracic intervention: importance of the internal
mammary artery. AJR Am J Roentgenol. 1990;154:47-9. Crossref
9. Paliouras D, Rallis T, Gogakos A, Asteriou C, Chatzinikolaou F,
Georgios T, et al. Surgical anatomy of the internal thoracic arteries
and their branching pattern: a cadaveric study. Ann Transl Med.
2015;3:212.
10. Hefel L, Schwabegger A, Ninković M, Wechselberger G, Moriggl B, Waldenberger P, et al. Internal mammary vessels: anatomical and clinical considerations. Br J Plast Surg. 1995;48:527-32. Crossref
11. Jelicić N, Djordjević L, Stosić T. The internal thoracic blood vessels
(internal thoracic arteries and veins) and their practical significance
[in Serbian]. Srp Arh Celok Lek. 1996;124:58-61.
12. Brennan P, Standring S, Wiseman S, editors. Gray’s Surgical Anatomy. Amsterdam, Netherlands: Elsevier Health Sciences; 2019. p 891.
13. Gupta S, Seaberg K, Wallace MJ, Madoff DC, Morello FA Jr,
Ahrar K, et al. Imaging-guided percutaneous biopsy of mediastinal
lesions: different approaches and anatomic considerations. Radiographics. 2005;25:763-86. Crossref
14. Glassberg RM, Sussman SK, Glickstein MF. CT anatomy of the
internal mammary vessels: importance in planning percutaneous
transthoracic procedures. AJR Am J Roentgenol. 1990;155:397-400. Crossref
15. Karaman B, Battal B, Bozkurt Y, Bozlar U, Demirkol S, Şahin MA,
et al. The anatomic evaluation of the internal mammary artery using
multidetector CT angiography. Diagn Interv Radiol. 2012;18:215-20. Crossref
16. Iguchi T, Hiraki T, Matsui Y, Fujiwara H, Sakurai J, Masaoka Y, et al. CT fluoroscopy-guided core needle biopsy of anterior mediastinal masses. Diagn Interv Imaging. 2018;99:91-7. Crossref