Diagnostic Accuracy of Lateral Abdominal Radiographs among Paediatric Patients in Detecting Hirschsprung Disease
ORIGINAL ARTICLE
Diagnostic Accuracy of Lateral Abdominal Radiographs among Paediatric Patients in Detecting Hirschsprung Disease
NDP Concepcion, AEMN Jusi
Institute of Radiology, St. Luke’s Medical Center, Quezon City, Philippines
Correspondence: Dr NDP Concepcion, Institute of Radiology, St. Luke’s Medical Center, Quezon City, Philippines. Email: npconcepcion@stlukes.com.ph
Submitted: 29 Dec 2020; Accepted: 23 Mar 2021.
Contributors: All authors designed the study, acquired the data, analysed the data, drafted the manuscript, and critically revised the manuscript
for important intellectual content. All authors had full access to the data, contributed to the study, approved the final version for publication, and
take responsibility for its accuracy and integrity.
Conflicts of Interest: All authors have disclosed no conflicts of interest.
Funding/Support: This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data Availability: All data generated or analysed during the present study are available from the corresponding author on reasonable request.
Ethics Approval: This study protocol was approved by the Institutional Scientific and Ethics Review Committees of the Research and Biotechnology Division of the hospital (#CT-18104). The need for informed consent was waived owing to the retrospective nature of the study.
Abstract
Purpose
The aim of this study was to determine the diagnostic accuracy of lateral abdominal radiographs in the
detection of Hirschsprung disease (HSCR) in paediatric patients compared with rectal biopsy as the standard.
Methods
This retrospective study was performed in cases with clinical suspicion of HSCR that had undergone lateral
or cross-table prone lateral abdominal radiographs and subsequent rectal biopsies at a tertiary hospital in Metro
Manila, Philippines. Reversal of the rectosigmoid index (RSI) on a lateral abdominal radiograph without or with a
transition zone was interpreted as positive for HSCR. The radiographic findings were correlated with histopathology.
Results
A total of 72 cases were included. Age ranged from 4 days to 12 years with a mean of 16 months. In all,
62 cases (86%) were positive for HSCR on biopsy, 39 of which had reversed RSI. Ten patients (14%) were negative
for HSCR on biopsy, seven of which showed no reversal of the RSI. Overall, the diagnostic accuracy of the lateral
abdominal radiograph was 64%. Sensitivity, specificity, positive predictive value, and negative predictive value were
63%, 70%, 93%, and 23%, respectively.
Conclusion
The presence of a reversed RSI on a lateral or cross-table prone lateral abdominal radiograph had
a high positive predictive value, indicating a high likelihood of HSCR. Therefore, such views are reliable tools in
predicting HSCR in infants and young children. Rectal biopsy should be done for confirmation but patients may no
longer need to undergo contrast enema.
Key Words: Constipation; Enema; Hirschsprung disease; Radiology, abdominal
中文摘要
兒科患者腹側位X線片診斷先天性巨結腸的診斷準確性
NDP Concepcion、AEMN Jusi
目的
與作為標準的直腸活檢相比,本研究確定側位腹部X線片在兒科患者先天性巨結腸的診斷準確性。
方法
這項回顧性研究於菲律賓馬尼拉大都會一家三級醫院進行,對臨床懷疑巨結腸的病例接受側位或橫台俯臥側腹位X線片和隨後的直腸活檢。側位腹部X光片上沒有或有過渡帶的直腸乙狀結腸指數(rectosigmoid index;RSI)的反轉解釋為巨結腸陽性。進行放射學檢查結果與組織病理學相關性的分析。
結果
共納入72例。年齡從4天到12歲不等,平均16個月。總共有62例(86%)活檢巨結腸陽性,其中39例見RSI反轉。10名患者(14%)活檢巨結腸為陰性,其中7名患者的RSI沒有反轉。總體而言,側位腹部X線片的診斷準確率為64%。敏感性、特異性、陽性預測值和陰性預測值分別為63%、70%、93%和23%。
結論
側位或橫台俯臥側腹位X線片顯示RSI反轉具有很高的陽性預測值,表明巨結腸的可能性很高。因此,這些表現是預測嬰幼兒巨結腸的可靠工具。應進行直腸活檢以確認,但患者可能不再需要接受造影劑灌腸。
INTRODUCTION
Hirschsprung disease (HSCR) is the most common
cause of paediatric intestinal obstruction.[1] It results
from failure of normal bowel innervation due to the
arrest of proximal-to-distal migration of vagal neural
crest cells, with a variable length of distal bowel lacking
parasympathetic Auerbach (intermuscular) and Meissner
(submucosal) plexuses.[2] There is resultant colonic
aganglionosis leading to symptoms such as abdominal
distension, irregular bowel movements, or chronic
constipation.
HSCR occurs in approximately 1 per 5000 live births
with a male-to-female ratio of 4:1.[1] It is responsible
for approximately 15% to 20% of cases of neonatal
bowel obstruction, presenting in the newborn period in
approximately 80% of cases.[2]
Initial diagnosis is mainly based on clinical history
and examination,[1] but approaches to diagnoses include
abdominal radiography, contrast enema, anorectal
manometry (which is not always readily available), and
rectal biopsy.[3]
Patients may present with failure to pass meconium within the first 24 to 48 hours of life or may subsequently develop chronic constipation. Intestinal obstruction may ensue,
causing abdominal distention, poor feeding, and poor
weight gain. Plain abdominal radiographs are routinely
taken as the initial imaging study in the assessment of
these patients, oftentimes in anteroposterior upright and
supine views with or without a lateral view.
Contrast enema is a valuable tool in the diagnosis of
HSCR,[3] with an accuracy ranging from 80% to 94%,[4]
sensitivity of 65% to 80% and specificity of 66% to
100%[5] when compared with anorectal manometry and
rectal biopsy. Common findings in contrast enema for
HSCR include reversal of the rectosigmoid index or
the presence of a transitional zone (RSI: the ratio of the
anteroposterior diameter of the rectum at the level of the
2nd sacral vertebral body to the anteroposterior diameter
of the sigmoid colon measured at the level of the 1st
sacral vertebral body on the lateral view. It is considered
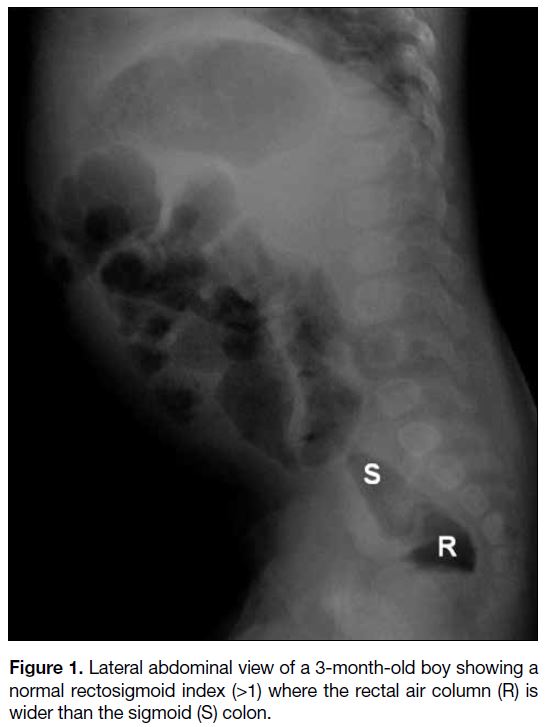
normal if the RSI is ≥1 [Figure 1], meaning the rectal
diameter is wider or at least equal to that of the sigmoid
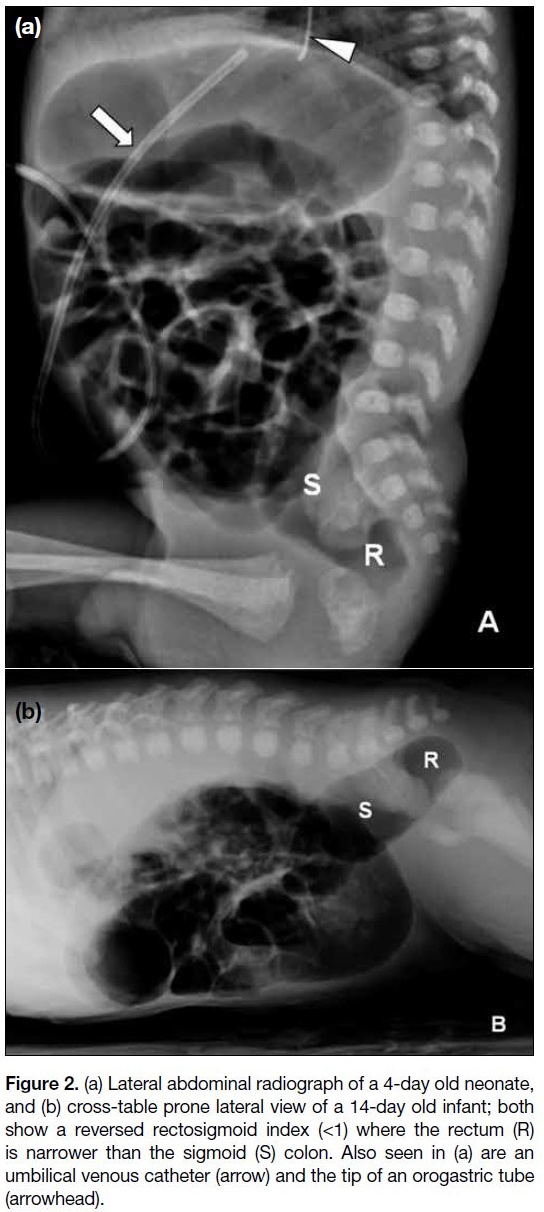
colon. If RSI is <1, it is considered abnormal [Figure 2].
A transitional zone is a severe form of reversed RSI
showing an abrupt change in colonic calibre with
shouldering), delay in barium evacuation >24 hours after
birth, jejunisation of the colon, a cobblestone appearance
of the aganglionic segment, and irregular contraction.[1] Although contrast enema is minimally invasive, it causes
unnecessary stress and discomfort not only for the
patients but also for the parents and/or caretakers.
Figure 1. Lateral abdominal view of a 3-month-old boy showing a
normal rectosigmoid index (>1) where the rectal air column (R) is
wider than the sigmoid (S) colon.
Figure 2. (a) Lateral abdominal radiograph of a 4-day old neonate,
and (b) cross-table prone lateral view of a 14-day old infant; both
show a reversed rectosigmoid index (<1) where the rectum (R)
is narrower than the sigmoid (S) colon. Also seen in (a) are an
umbilical venous catheter (arrow) and the tip of an orogastric tube
(arrowhead).
The gold standard of diagnosis for HSCR remains rectal
biopsy, which will demonstrate absence of ganglion
cells in the submucosal layer distal to the transitional
zone as well as presence of acetylcholinesterase-positive
hypertrophic nerve fibres.[3]
Our primary objective was to assess the diagnostic
accuracy of plain lateral abdominal radiography in
the diagnosis of HSCR, with the results of the rectal
biopsy used as the reference standard. To the best of our
knowledge, published studies on plain lateral abdominal
radiography in the diagnosis of HSCR as correlated with
rectal biopsy are scarce.
METHODS
The study was a retrospective study of paediatric
patients, aged ≤5 years, suspected of having HSCR,
who underwent abdominal radiographs with lateral or
cross-table prone lateral views, as a stand-alone study or as scout views prior to a barium or water-soluble
contrast enema, and subsequent rectal biopsy at St.
Luke’s Medical Center–Quezon City from January 2011
to December 2020 and at St. Luke’s Medical Center–Global City from January 2010 to December 2020.
Clinical data and histopathological results were retrieved from the hospital’s HealthCare System. Demographic information such as age and gender were recorded.
Clinical suspicion of HSCR was due to the presence of
abdominal distention, delayed passage of meconium,
and/or constipation.
The digital radiographs were reviewed via the Picture
Archiving and Communication System. The lateral
views or cross-table prone lateral views were used for
evaluation. The presence of an abnormal RSI (<1) with
or without a transitional zone was considered a positive
reading. Evaluation of the digital images was done by
a single paediatric radiologist of more than 12 years’
experience, who was blinded on case information and
rectal biopsy findings.
Patients who had undergone prior gastrointestinal
surgery for any reason and those who had a cross-table
supine lateral view were excluded from this study.
The rectal biopsy results were interpreted as positive if the
histopathological report mentioned any of the following
findings: absence of ganglion cells/aganglionosis,
immature ganglion cells, or hypoganglionosis. Absence
of these findings or an inconclusive report was considered
negative.
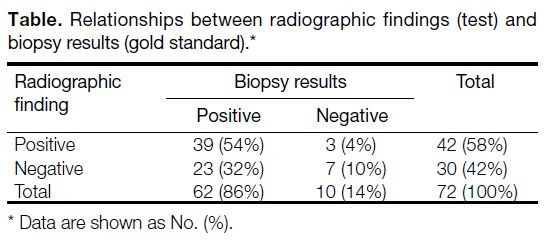
The findings from the lateral radiographs were then
correlated with the rectal biopsy results using the four-fold
table technique (Table) to compute for the accuracy,
sensitivity, specificity, positive predictive value, and
negative predictive value. To determine the relationship
between patient age and gender with radiographic
findings and biopsy results, independent sample t tests
and Fisher’s exact test (with a Chi-square test for small
samples) at a 5% level of significance, were utilised.
Table. Relationships between radiographic findings (test) and biopsy results (gold standard).
RESULTS
A total of 72 paediatric cases clinically suspected of
having HSCR were included in the study. In all, 46 were
male and 26 were female, with a male-to-female ratio
of 1.8:1, with age ranging from 4 days to 12 years old
(mean age 16.09 ± 32.16 mo). Those with positive lateral
radiographs had a mean age of 12.17 ± 32.05 months;
negative lateral radiographs being 21.59 ± 32.02 months;
positive rectal biopsy being 11.20 ± 23.68 months; and
negative rectal biopsy being 32.88 ± 48.47 months.
The differences in age and gender in relation to the
radiographic findings and biopsy results were not
statistically significant.
In total, 62 patients (86%) were confirmed positive for HSCR on rectal biopsy, 39 of which were also positive
on the lateral abdominal radiographs. Ten patients (14%)
were negative for HSCR on biopsy, seven of which were
likewise negative on the radiographs (Table).
In using lateral abdominal radiography to detect HSCR,
its sensitivity and specificity were computed to be 63%
and 70%, respectively. The positive predictive value was
high at 93%, while the negative predictive value was
only 23%. Overall accuracy was 64%.
DISCUSSION
A plain (non-contrast) abdominal radiograph is the
initial study for patients manifesting with abdominal
distention, failure to pass meconium in 24 to 48 hours
after birth, and/or constipation. This is routinely taken
in anteroposterior supine and upright views, along with
a lateral view. Additional cross-table prone or supine
lateral views may also be included in patients with
possible intestinal obstruction and to better visualise the
rectosigmoid air column.[6] [7] [8] [9] These are easily done, taking
less than 5 minutes, with minimal radiation exposure,
and are also relatively cheap and ubiquitous.
A contrast enema using either barium solution or
water-soluble iodinated contrast material has 80% to
94% accuracy[4] in detecting HSCR, more accurate than
a lateral plain abdominal study (56%). Most common
findings appreciated were presence of a transitional zone
and a reversed RSI.[1] [4] [5] [10] [11] However, this procedure is
more invasive because it necessitates insertion of a rectal
tube.[12] It is likewise more expensive, takes more time,
and involves some ionising radiation exposure.
A study by Pratap et al in 2007[4] compared the plain
abdominal radiograph transitional zone (PARTZ)
with the contrast enema transitional zone (CETZ) in
diagnosing HSCR. Their study concluded that PARTZ
and CETZ matched with the level of the transitional
zone in 22 (92%) and 13 (72%) patients, respectively.[4] PARTZ was said to be better than CETZ in predicting
the level of the transitional zone in cases of inconclusive
contrast enema.[4]
This study obtained an overall diagnostic accuracy
of 64% with sensitivity of 63%, specificity of 70%
and negative predictive value of 23% in predicting
HSCR using the lateral abdominal radiograph, which
is comparably low relative to contrast enema and rectal
biopsy. This is actually not unusual because decreased
or non-visualisation of the rectosigmoid air column is
common in patients without bowel preparation, due to
presence of stool and/or fluid within the distal colonic
segments. It may even be empty and thus physiologically
collapsed. The positive predictive value, however, was
very high at 93%, indicating that detection of a reversed
RSI (<1) without or with a transitional zone on a plain
lateral or cross-table prone lateral radiograph correlates
with high likelihood that the patient has HSCR. Age and
gender were non-contributing factors.
The authors recognise some limitations in the
methodology. This was a retrospective study and thus
the radiological technique was not fully controlled
resulting in non-uniform image quality. Moreover, both
lateral and cross-table prone lateral views were taken
into consideration, and the latter view is considered more
superior in the visualisation of the rectosigmoid colon.
It is therefore the recommendation of the authors that a
prospective study be done using standardised imaging
parameters in acquiring only the cross-table prone lateral
view. Lastly, the number of true negatives is limited
because it is rare for surgeons to perform a biopsy on
patients not suspected of having HSCR.
In conclusion, the diagnostic accuracy of the lateral
abdominal radiograph in the detection of HSCR among
paediatric patients ≤12 years prior to rectal biopsy for
suspected HSCR is only 64%. However, there was a high
positive predictive value of 93% which means that if a
reversed RSI (<1) is appreciated on the lateral abdominal
radiograph, there is also a high likelihood that the patient
has HSCR disease. Therefore, a lateral or cross-table prone lateral abdominal radiograph that demonstrates a
reversed RSI is a reliable view in the detection of HSCR
in infants and young children. Rectal biopsy may be
done for confirmation but patients may no longer need to
undergo contrast enema.
REFERENCES
1. Peyvasteh M, Askarpour S, Ostadian N, Moghimi MR, Javaherizadeh H. Diagnostic accuracy of barium enema findings
in Hirschsprung’s disease [in English, Portuguese]. Arq Bras Cir
Dig. 2016;29:155-8. Crossref
2. Hernanz-Schulman M. Hirschsprung disease. In: Coley BD, editor. Caffey’s Pediatric Diagnostic Imaging. 12th ed. Philadelphia: Elsevier Saunders; 2013. p 1112-6.
3. Frongia G, Günther P, Schenk JP, Strube K, Kessler M, Mehrabi A, et al. Contrast enema for Hirschsprung disease investigation: diagnostic accuracy and validity for subsequent diagnostic and surgical planning. Eur J Pediatr Surg. 2016;26:207-14. Crossref
4. Pratap A, Gupta DK, Tiwari A, Sinha AK, Bhatta N, Singh SN,
Agrawal CS, Kumar A, Adhikary S. Application of a plain
abdominal radiograph transition zone (PARTZ) in Hirschsprung's
disease. BMC Pediatr. 2007;7:5. Crossref
5. Huang CC, Shih SL, Chen YF, Yang FS. Hirschsprung disease and
contrast enema: diagnostic value of simplified contrast enema and
twenty-four-hour-delayed abdominal radiographs. J Radiol Sci.
2011;36:159-64.
6. Menashe SJ, Iyer RS, Parisi MT, Otto RK, Weinberger E, Stanescu AL. Pediatric abdominal radiographs: common and less common errors. AJR Am J Roentgenol. 2017;209:417-29. Crossref
7. Prasad GR, Aziz A. Abdominal plain radiograph in neonatal intestinal obstruction. J Neonat Surg. 2017;6:6. Crossref
8. Aggarwal SK. Neonatal Intestinal Obstruction. In: Choudhury P, Bagga A, Chugh K, Ramji S, Gupta P, editors. Principles of Pediatric and Neonatal Emergencies. 3rd ed. New Delhi: Jaypee Brothers Medical Publishers; 2011. p 607-19. Crossref
9. Aggarwal SK. Gastrointestinal and Abdominal Malformations. In:
Gupta P, Menon PS, Ramji S, Lodha R, editors. PG Textbook of
Pediatrics: Volume 1: General Pediatrics and Neonatology. 2nd
ed. New Delhi: Jaypee Brothers Medical Publishers; 2015. p 606-15.
10. Alehossein M, Roohi A, Pourgholami M, Mollaeian M, Salamati P.
Diagnostic accuracy of radiologic scoring system for evaluation
of suspicious Hirschsprung disease in children. Iran J Radiol.
2015;12:e12451. Crossref
11. Singh CD, Baruah RR. Role of barium enema in the diagnosis of Hirschsprung disease. J. Evol Med Dent Sci. 2016;5:5245-8. Crossref
12. American College of Radiology. American College of
Radiology–Society for Pediatric Radiology Practice Parameter
for the Performance of Pediatric Fluoroscopic Contrast Enema
Examinations. 2016. Available from: https://www.acr.org/-/media/ACR/Files/Practice-Parameters/FluourConEnema.... Accessed 15 Oct 2020.