Coronary Computed Tomography Angiography Service in the Accident and Emergency Department: Pilot Study
ORIGIINAL ARTICLE
Coronary Computed Tomography Angiography Service in the Accident and Emergency Department: Pilot Study
HHT Chau1, WH Luk1, JKF Ma1, HHL She2, MC Lam3, YK Li4, CM Chan4, WCL Wong4
1 Department of Radiology, Princess Margaret Hospital, Hong Kong
2 Department of Radiology, Adventist Hospital, Hong Kong
3 Department of Radiology, Integrated Diagnostic Imaging Centre, Hong Kong
4 Accident and Emergency Department, Princess Margaret Hospital, Hong Kong
Correspondence: Dr HHT Chau, Department of Radiology, Princess Margaret Hospital, Hong Kong. Email: cht546@ha.org.hk
Submitted: 13 Oct 2020; Accepted: 22 Feb 2021.
Contributors: All authors designed the study and acquired the data. HHT Chau analysed the data and drafted the manuscript. All authors critically revised the manuscript for important intellectual content.
Conflicts of Interest: All authors have disclosed no conflicts of interest.
Funding/Support: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data Availability: All data generated or analysed during the present study are available from the corresponding author on reasonable request.
Ethics Approval: This study was carried out with approval from the Kowloon West Cluster Ethics Committee (KWC REC Ref: KW/EX-18-023(119-23)). The requirement for patient consent was waived by the committee.
Acknowledgement: The authors would like to acknowledge physicians at Princess Margaret Hospital Accident and Emergency Department
physicians for their patient care and Research Officer Miss Ellen Yu for providing statistical support.
Abstract
Introduction
Studies in western countries have shown that installation of coronary computed tomography
angiography (CCTA) in the accident and emergency department (AED) facilitates safe triage and early discharge of
low-to-intermediate risk patients with suspected acute coronary syndrome. The aim of this pilot study was to determine
whether the workflow of a CCTA service in a local hospital AED could safely discharge low-to-intermediate risk
patients presenting with acute chest pain.
Methods
Low-to-intermediate risk chest pain patients (stratified using the HEART score), who underwent CCTA
in the AED, were included. Patient health records were followed up for 2 years. Clinical variables, time needed for
diagnosis, CCTA results, and major adverse cardiac events (MACE) were evaluated.
Results
Thirty-four patients (17 men, 17 women) were included in this study from March to August 2017. Nineteen
patients (55.9%) were low-risk and 15 (44.1%) were intermediate-risk. Mean time to CCTA was 39.2 ± 27.9 hours.
Twenty-four patients (70.6%) with negative CCTA results (<50% coronary artery stenosis) were discharged home
from AED and 10 patients (29.4%) with positive result (≥50% stenosis) were admitted to medical wards for further
assessment. In the 2-year follow-up period, no MACE was found in the negative group. For MACE in the positive
group, no cardiac death, one non-fatal myocardial infarction (contraindicated for revascularisation) and five
revascularisations were noted.
Conclusion
CCTA allows safe discharge of low-to-intermediate risk patients presenting with acute chest pain in
the AED. An AED CCTA service is effective in reducing the waiting time and length of stay.
Key Words: Cardiology; Computed tomography angiography; Coronary artery disease; Emergency medicine;
Radiology
中文摘要
急診科冠狀動脈計算機斷層掃描血管造影服務:初步研究
周凱婷、陸永恆、馬嘉輝、佘凱琳、林茂珠、李儒君、陳子明、黃祥麟
引言
西方國家的研究表明,在急診科中使用冠狀動脈計算機斷層掃描血管造影(CCTA)有助於進行分流和疑似急性冠狀動脈綜合徵的中低風險患者早期出院。本初步研究旨在確定本地醫院急診科CCTA服務流程是否可以使急性胸痛的中低風險患者安全地出院。
方法
納入在急診科接受CCTA的中低風險胸痛患者(使用HEART評分分層)。隨訪患者健康記錄2年,評估臨床變量、診斷所需時間、CCTA結果和主要心臟不良事件(MACE)。
結果
本研究於 2017年 3月至 8月共納入 34名患者(17名男性,17名女性)。 19名患者(55.9%)為低危患者,15名(44.1%)為中危患者。到接受CCTA的平均時間為39.2 ± 27.9小時。24名患者(70.6%)CCTA結果陰性(<50%冠狀動脈狹窄)從急診科出院,10名患者(29%)陽性結果(≥50%冠狀動脈狹窄)被送往內科病房作進進一步評估。隨訪2年,CCTA陰性組未發現MACE。 CCTA陽性組MACE結果:無心源性死亡、1 例非致死性心肌梗死(血管重建禁忌)和 5例血管重建。
結論
急診科CCTA允許急性胸痛的中低風險患者安全出院。急診科 CCTA 服務可有效減少等待時間和住院時間。
BACKGROUND
Cardiac disease is the third leading cause of death in
Hong Kong. According to the statistics of the Hong
Kong Department of Health, on average 10.6 people
died from coronary artery disease (CAD) per day in
2017.[1] In the same year, this disease accounted for 8.4%
of all registered deaths in Hong Kong.[1]
Acute chest pain is a common presenting complaint in
the accident and emergency department (AED). It is
challenging for AED physicians to distinguish patients
at high risk for CAD that require admission for urgent
treatment and those at low risk that can be safely
discharged home.[2] In traditional practice, the risk of
CAD in chest pain patients is assessed by history taking,
physical examination, serial electrocardiograms (ECG),
and cardiac biomarkers such as troponin, creatinine
kinase, and myoglobin.[3] Referral to cardiac subspecialties
for further investigations and treatment usually takes
time and the risk of cardiac death increases with time.
Early recognition of patients at risk in the AED can allow
the allocation of resources more efficiently.
Recent advances in coronary computed tomography
angiography (CCTA) allow coronary vasculature
to be evaluated rapidly and non-invasively, leading to an increase in its utilisation in the AED setting.[4]
Multiple randomised controlled trials in the western
world demonstrated that CCTA could facilitate safe
triage and early discharge of low-to-intermediate risk
patients with suspected acute coronary syndrome, with
possible reduction of AED length of stay and cost of
care.[5] [6] [7] [8] Therefore, our radiology department installed a
CCTA service in collaboration with the AED in order to
improve clinical safety and to provide a more efficient
way to manage patients with chest pain who were at low-to-intermediate risk for CAD.
The aim of this pilot study was to find out whether the
workflow of a CCTA service in a local hospital AED
could safely discharge low-to-intermediate-risk patients
presenting with acute chest pain.
METHODS
A CCTA service had been set up in our hospital (Princess
Margaret Hospital) AED and a team of dedicated
AED physicians (Emergency Medicine Fellows) were
available for arranging and booking CCTA. The service
was targeted at adult patients (age ≥18 y) presenting
with acute chest pain, who had two sets of normal serum
troponin levels and normal or non-diagnostic ECG
without dynamic changes concerning for ischaemia. All patients who underwent CCTA in our AED from March
to August 2017 were included in this pilot study.
Candidates were risk stratified by AED physicians using
the HEART score and those classified as either low- or
intermediate-risk for CAD were selected. The scoring
system consists of five parameters: history (H), ECG (E),
age (A), risk factors (R), and troponin level (T), which
can be derived after a standard focused history taking
and evaluation. It predicts the risk of a major adverse
cardiac event (MACE) within 6 weeks after presentation:
myocardial infarction (MI), need for percutaneous
coronary intervention or coronary artery bypass graft,
or death. Patients scoring 0 to 3 (low risk) and 4 to 6
(intermediate risk) were offered CCTA examinations in
the AED.
Patients were excluded from CCTA if their first two
sets of troponin were elevated, dynamic ECG changes
concerning for ischaemia, intravenous contrast allergy,
impaired renal function (creatinine level ≥115 μmol/L),
atrial or ventricular arrhythmias with haemodynamic
instability, clinically decompensated heart failure,
or a normal CCTA performed within the preceding
24 months.
Ethics approval for this study was obtained from the
institutional review board. Written informed consent was
obtained from the patients before the procedure. Patients
were prepared for the CCTA examination according
to local departmental protocol, including refraining
from caffeine-containing substances for 12 hours and
withholding metformin for 48 hours. Steroid coverage
(either oral or intravenous) was administered to those
with a history of non-contrast drug allergy. Patients
were fasted for 4 hours before the computed tomography
examination. A large-bore intravenous access (18 G)
cannula was set up in the right arm (preferably right
antecubital fossa). Patients’ heart rates were optimised
to <65 beats per minute by rate-lowering agents such
as beta blockers or calcium channel blockers in order to
reduce motion artefact during the examination. After the
CCTA examination, patients were transferred back to
the AED for removal of the intravenous access catheter
and further management.
Patient health records were reviewed for clinical variables
including age, sex, risk factors for CAD (obesity,
hypertension, dyslipidaemia, diabetes mellitus and
current smoking) and the HEART score was calculated.
The time from first evaluation by an AED physician to diagnosis by CCTA was recorded. Their CCTA results
were collected and analysed. For those with CCTA-positive
results, the time from first evaluation by an
AED physician to angiography and intervention was
calculated. Patient health records were followed up until
2 years after the presentation at the AED to assess for
any major clinical outcomes, including MACE.
Excel (version 2019; Microsoft, Redmond [WA], United
States) and SPSS (Windows version 22; IBM Corp.,
Armonk [NY], United States) were used for data analysis.
All categorical variables were examined using the Mann-Whitney U test, Fisher’s exact test, or Pearson’s Chi-square
test where appropriate. All continuous variables
are shown as mean ± standard deviation and median
(interquartile range [IQR]).
RESULTS
The HEART score[9] was proven to be a quick and reliable
tool to triage chest pain patients in the AED setting,
particularly in identifying low-risk patients with chest
pain.[10] [11] A total of 34 patients (17 men, 17 women)
were recruited for this pilot study, with mean age 63.3 ± 9.0 years (range, 34-78 years). The median HEART score
was 3 (IQR: 3-5). Nineteen patients were classified as
low-risk (HEART score = 0-3) and 15 were intermediate
risk (HEART score = 4-6). The Table shows the number
of patients with each risk factor for CAD. Ten of
26 patients (38.5%) were obese (body mass index
≥ 25 kg/m2), 19 (55.9%) were hypertensive, 18 (52.9%)
had dyslipidaemia and six (17.6%) were diabetic. Only
four (11.8%) were smokers. Those risk factors were
taken into account when calculating the HEART score.
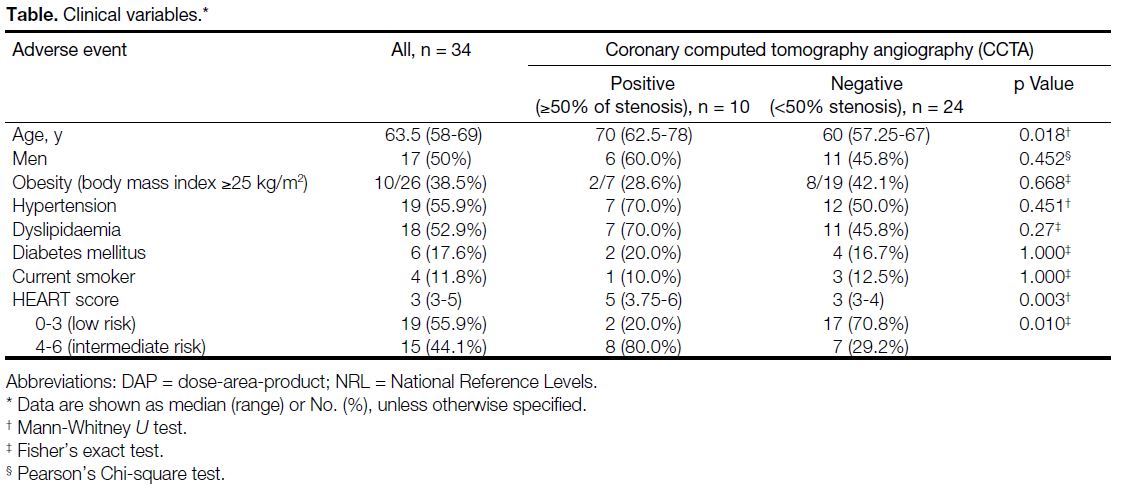
Table. Clinical variables
No patients who underwent CCTA experienced
complications from the procedure. Mean time to CCTA
was 39.2 ± 27.9 hours. Twenty-four patients (70.6%)
with a negative CCTA result (<50% stenosis of any
major coronary artery) were discharged home from the
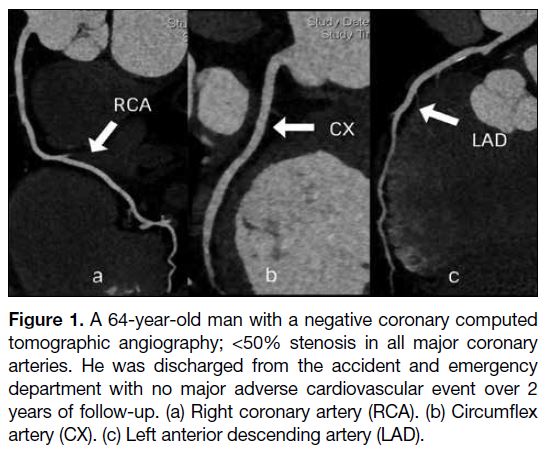
AED (Figure 1). Seventeen of the 24 patients (70.8%)
were in the low-risk group and seven (29.2%) were in the
intermediate-risk group.
Figure 1. A 64-year-old man with a negative coronary computed
tomographic angiography; <50% stenosis in all major coronary
arteries. He was discharged from the accident and emergency
department with no major adverse cardiovascular event over 2
years of follow-up. (a) Right coronary artery (RCA). (b) Circumflex
artery (CX). (c) Left anterior descending artery (LAD).
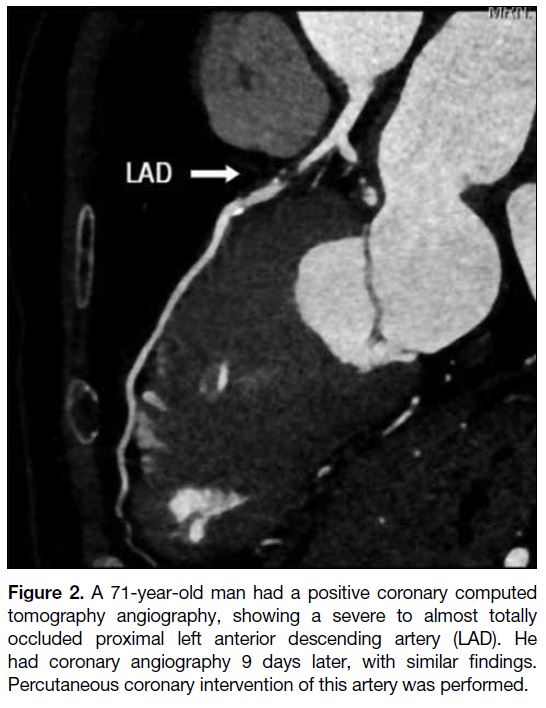
Ten patients (29.4%) with a positive CCTA result (≥50%
of stenosis on CCTA) were admitted to medical wards for
further assessment by cardiologists (Figure 2). They had
their symptoms, ECG and blood troponin level monitored.
They also had an echocardiogram assessment. None of
the patients with positive CCTA results had subsequent
ECG changes during their hospital stay. Two of 10
patients with positive CCTA results had raised serum troponin level upon further testing, while one of them
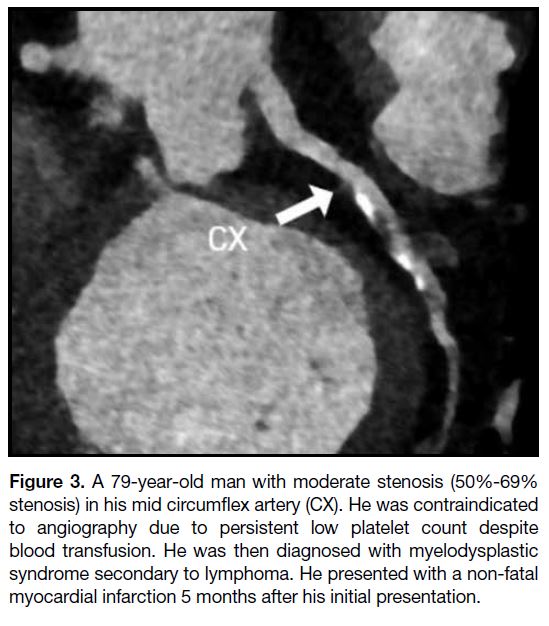
had a non-fatal MI 5 months later; the patient was not a
candidate for percutaneous coronary intervention due to a persistently low platelet count (Figure 3). He was later
diagnosed with myelodysplastic syndrome secondary
to lymphoma. Two of 10 patients with positive CCTA results were classified as low-risk by HEART. Both of
them showed 50% to 69% coronary artery stenosis and
were managed conservatively.
Figure 2. A 71-year-old man had a positive coronary computed
tomography angiography, showing a severe to almost totally
occluded proximal left anterior descending artery (LAD). He
had coronary angiography 9 days later, with similar findings.
Percutaneous coronary intervention of this artery was performed.
Figure 3. A 79-year-old man with moderate stenosis (50%-69%
stenosis) in his mid circumflex artery (CX). He was contraindicated
to angiography due to persistent low platelet count despite
blood transfusion. He was then diagnosed with myelodysplastic
syndrome secondary to lymphoma. He presented with a non-fatal
myocardial infarction 5 months after his initial presentation.
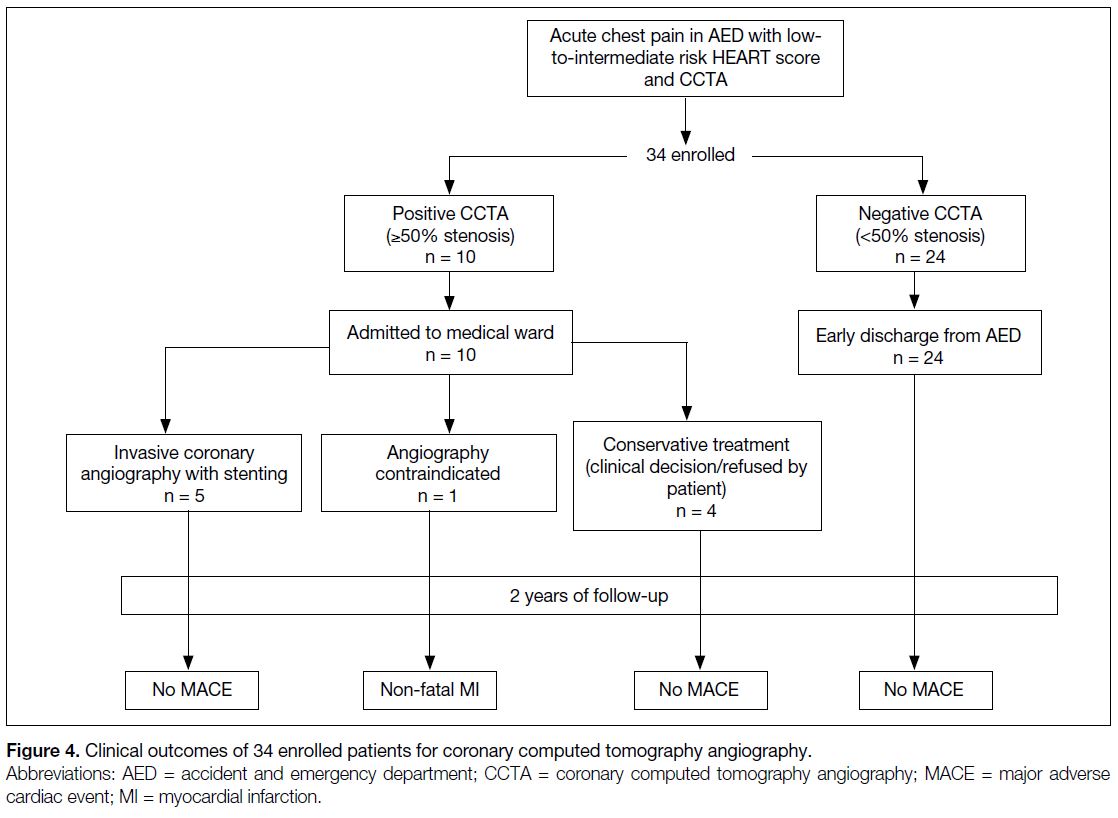
In the 2-year follow-up period, none of those patients with a negative CCTA result had MACE, including cardiac death, MI, or the need for coronary revascularisation
(Figure 4). In the negative CCTA group, none of the
patients had died. Five of 10 patients with a positive
CCTA result (50%) underwent a revascularisation
procedure with no adverse events in the follow-up
period. The time taken to angiography varied from 9 to
154 days, depending on the patient’s symptoms and the
clinician’s decision. The other half who did not undergo
revascularisation had contraindications to the procedure,
preferred conservative treatment, or were subject to the
clinician’s judgement.
Figure 4. Clinical outcomes of 34 enrolled patients for coronary computed tomography angiography.
Two clinical variables showed significant differences
between the positive CCTA group and negative CCTA
group. There was a significant difference in their
HEART score: low risk (0-3) with positive CCTA (20%)
and negative CCTA (70.8%); intermediate risk (4-6)
with positive CCTA (80%) and negative CCTA (29.2%)
[p = 0.01]. The other clinical variable that was
significantly different between the two groups was a
higher median age in the positive CCTA group (70 y
[IQR: 62.5-78 y] vs. negative CCTA: 60 y [IQR: 57.25-67 y]; p = 0.018). There was no significant difference
in other clinical variables between the two groups,
including gender, obesity (body mass index ≥25 kg/m2),
hypertension, dyslipidaemia, diabetes mellitus and
current smoker.
DISCUSSION
Previous studies have revealed that CCTA had a relatively
high negative predictive value of >95%, which was
helpful to rule out significant CAD and safely discharge
low-risk patients.[12] [13] [14] [15] [16] This pilot study demonstrated
consistent findings: no major cardiac events in 2 years
of follow-up for those patients who had negative
CCTA results. It suggests that CCTA would be a reliable
and safe tool in identifying low-to-intermediate risk
patients presenting with acute chest pain in our AED,
provided that they had negative cardiac enzyme results
and ECG findings. If more patients with negative CCTA
findings can be discharged immediately from the AED in
the future, further extensive diagnostic tests and hospital
admission can be avoided, saving hospital costs.
Meta-analysis showed that CCTA was highly sensitive
(98%) and moderately specific 84%) in detecting
clinically significant coronary artery stenosis.[17] Using
CCTA and clinical diagnosis of the MI after 2 years
of follow-up as the gold standard of diagnosis of symptomatic
CAD, the sensitivity and specificity of the low- and
intermediate-risk HEART scores for detection of
symptomatic CAD in this study were 80.0% (8/10)
and 70.8% (17/24), respectively. The false-negative
rate of a low-risk HEART score was 10.5% (2/19). A
previous study revealed that the predictability of MACE
in 6 weeks in low- and intermediate-risk HEART score
patients were 2.5% and 20.3%, respectively.[9] Therefore,
addition of CCTA service is beneficial to patient care.
One patient had an adverse cardiac event in the 2-year
follow-up period. Although his CCTA result was positive
(Figure 3), he was not a candidate for angiography due
to persistent low platelet count due to lymphoma. His
platelet count remained low despite chemotherapy and
blood transfusions. Without definitive treatment, he had
a non-fatal MI 5 months after his initial presentation
with chest pain. In this trial, 10 of 34 patients (29.4%)
had a positive CCTA while two of them had subsequent
elevation of serum troponin levels signifying an acute
MI. Since those two patients were not in the low-risk
group, it further supports that CCTA allows quicker
identification of patients who requires intervention to
avoid future cardiac events.
When comparing the positive and negative CCTA
groups, there was no statistically significant difference
in most clinical variables. Patients in the positive CCTA
group were comparatively older and had a higher HEART score, which were valid as age and the HEART
score correlate with the risk of CAD.
There was a prolonged CCTA waiting time in this study;
mean time to CCTA was 39.2 hours. This was mainly
related to limited CCTA service provision with inadequate
cardiovascular imaging specialists and resources for the
pilot study. The service was only available on alternate
days over weekdays, so selected patients could have
waited for more than 2 days (in addition of weekends
and/or public holidays) for the examination. Increasing
manpower and daily CCTA slot provision is necessary to
reduce the waiting time and length of hospital stay. This
can potentially increase throughput in AED.
This is a pilot study, and therefore, did not have adequate
power to demonstrate the effectiveness and cost-efficiency
of CCTA service in AED. However, it was
adequate to reflect the feasibility of our current workflow
and to guide future study. A more comprehensive study
with a larger sample size and longer period is expected
to give a better reflection on long-term costs and benefits
of CCTA service in AED. As stated above, provision of
CCTA service was limited by resources and manpower.
More imaging slots should be provided in AED so that
the waiting time can be shortened, and patients can
be discharged earlier. In this retrospective study, the
information collected from the electronic patient record
might not be comprehensive as some records were not
well-documented. A prospective study is preferred in the
future. Future study can also include a control group for
comparison.
CONCLUSION
This pilot study demonstrated that CCTA could be used
as a negative predictor of cardiovascular events. It is
a reliable tool to identify and allows safe discharge of
low-to-intermediate risk patients presenting with acute
chest pain in the AED. Increasing manpower and daily
CCTA slot provision are necessary to reduce the waiting
time and length of hospital stay. A more comprehensive
study in the future can give a better evaluation of the cost
and the long-term benefits of application of CCTA in the
emergency department.
REFERENCES
1. HealthyHK, Department of Health, Hong Kong SAR Government. Public health information and statistics of Hong Kong. Available
from: https://www.healthyhk.gov.hk/phisweb/en/chart_detail/24/.
Accessed 14 Jun 2020.
2. Amsterdam EA, Kirk JD, Bluemke DA, Diercks D, Farkouh ME, Garvey JL, et al. Testing of low-risk patients presenting to the emergency department with chest pain: a scientific statement from the American Heart Association. Circulation. 2010;122:1756-76. Crossref
3. Amsterdam EA, Wenger NK, Brindis RG, Casey DE Jr,
Ganiats TG, Holmes DR Jr, et al. 2014 AHA/ACC Guideline for the
Management of Patients with Non-ST-Elevation Acute Coronary
Syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J
Am Coll Cardiol. 2014;64:e139-228. Crossref
4. Yang FB, Guo WL, Sheng M, Sun L, Ding YY, Xu QQ, et al.
Diagnostic accuracy of coronary angiography using 64-slice
computed tomography in coronary artery disease. Saudi Med J.
2015;36:1156-62. Crossref
5. Litt HI, Gatsonis C, Snyder B, Singh H, Miller CD, Entrikin DW,
et al. CT angiography for safe discharge of patients with possible
acute coronary syndromes. N Engl J Med. 2012;366:1393-403. Crossref
6. Hoffmann U, Truong QA, Schoenfeld DA, Chou ET, Woodard PK, Nagurney JT, et al. Coronary CT angiography versus standard evaluation in acute chest pain. N Engl J Med. 2012;367:299-308. Crossref
7. Goldstein JA, Chinnaiyan KM, Abidov A, Achenbach S, Berman DS, Hayes SW, et al. The CT-STAT (Coronary Computed
Tomographic Angiography for Systematic Triage of Acute Chest
Pain Patients to Treatment) trial. J Am Coll Cardiol. 2011;58:1414-22. Crossref
8. Hoffmann U, Bamberg F, Chae CU, Nichols JH, Rogers IS,
Seneviratne SK, et al. Coronary computed tomography angiography
for early triage of patients with acute chest pain: the ROMICAT
(Rule Out Myocardial Infarction using Computer Assisted
Tomography) trial. J Am Coll Cardiol. 2009;53:1642-50. Crossref
9. Six AJ, Backus BE, Kelder JC. Chest pain in the emergency room:
value of the HEART score. Neth Heart J. 2008;16:191-6. Crossref
10. Backus BE, Six AJ, Kelder JC, Bosschaert MA, Mast EG,
Mosterd A, et al. A prospective validation of the HEART score
for chest pain patients at the emergency department. Int J Cardiol.
2013;168:2153-8. Crossref
11. Six AJ, Cullen L, Backus BE, Greenslade J, Parsonage W,
Aldous S, et al. The HEART score for the assessment of patients
with chest pain in the emergency department: a multinational
validation study. Crit Pathw Cardiol. 2013;12:121-6. Crossref
12. Meijboom WB, Meijs MF, Schuijf JD, Cramer MJ, Mollet NR,
van Mieghem CA, et al. Diagnostic accuracy of 64-slice computed
tomography coronary angiography: a prospective, multicenter,
multivendor study. J Am Coll Cardiol. 2008;52:2135-44. Crossref
13. Meijboom WB, Mollet NR, Van Mieghem CA, Weustink AC,
Pugliese F, van Pelt N, et al. 64-Slice CT coronary angiography in
patients with non-ST elevation acute coronary syndrome. Heart.
2007;93:1386-92. Crossref
14. Budoff MJ, Dowe D, Jollis JG, Gitter M, Sutherland J,
Halamert E, et al. Diagnostic performance of 64-multidetector
row coronary computed tomographic angiography for evaluation
of coronary artery stenosis in individuals without known
coronary artery disease: results from the prospective multicenter
ACCURACY (Assessment by Coronary Computed Tomographic
Angiography of Individuals Undergoing Invasive Coronary
Angiography) trial. J Am Coll Cardiol. 2008;52:1724-32. Crossref
15. Mowatt G, Cummins E, Waugh N, Walker S, Cook J, Jia X,
et al. Systematic review of the clinical effectiveness and costeffectiveness
of 64-slice or higher computed tomography
angiography as an alternative to invasive coronary angiography in
the investigation of coronary artery disease. Health Technol Assess.
2008;12:iii-iv, ix-143. Crossref
16. Ladapo JA, Hoffmann U, Bamberg F, Nagurney JT, Cutler DM,
Weinstein MC, et al. Cost-effectiveness of coronary MDCT in the
triage of patients with acute chest pain. AJR Am J Roentgenol.
2008;191:455-63. Crossref
17. Yin X, Wang J, Zheng W, Ma J, Hao P, Chen Y. Diagnostic
performance of coronary computed tomography angiography
versus exercise electrocardiography for coronary artery disease: a
systematic review and meta-analysis. J Thorac Dis. 2016;8:1688-96. Crossref