Normal Tibial Tubercle to Trochlear Groove Distance in an Adult Chinese Population
ORIGINAL ARTICLE
Normal Tibial Tubercle to Trochlear Groove Distance in an Adult Chinese Population
KY Man, KY Au, KY Cho
Department of Radiology, Pamela Youde Nethersole Eastern Hospital, Hong Kong
Correspondence: Dr KY Man, Department of Radiology, Pamela Youde Nethersole Eastern Hospital, Hong Kong. Email: dsgundam@hotmail.com
Submitted: 19 Apr 2018; Accepted: 8 Jun 2018.
Contributors: KYM designed the study. KYM and KYA acquired the data. KYM analysed the data and drafted the manuscript. All authors
critically revised the manuscript for important intellectual content. All authors had full access to the data, contributed to the study, approved the
final version for publication, and take responsibility for its accuracy and integrity.
Acknowledgement: The principal author would like to thank his family who provided insight and spiritual support.
Conflicts of Interest: All authors have disclosed no conflicts of interest.
Funding/Support: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data Availability: All data generated or analysed during the present study are available from the corresponding author on reasonable request.
Ethics Approval: This study was approved by the Hong Kong East Cluster Research Ethics Committee (Ref HKECREC-2017-064).
Abstract
Objective
To define the normal tibial tubercle to trochlear groove (TT-TG) distance in an adult Chinese population
and to confirm that magnetic resonance imaging (MRI) measurements of TT-TG distance are reliable and reproducible.
Methods
We conducted a retrospective review of MRI scans of 100 skeletally mature knees in an adult Chinese cohort
from January 2015 to January 2016. Patients with MRI or clinical evidence of previous lateral patellar dislocation
were excluded. TT-TG distance in MRI scans of normal knees was measured. Intraobserver and interobserver
agreement was evaluated.
Results
In our study, the mean normal value of the TT-TG distance in an adult Chinese cohort was found to be 10.36 ± 2.52 mm (men 10.92 ± 2.59 mm and women 9.67 ± 2.28 mm). Intraobserver and interobserver agreement regarding TT-TG distance measurement with MRI was excellent.
Conclusion
This study can form the basis for future studies on the relationship between TT-TG distance and patellar
instability in the adult Chinese population.
Key Words: Asian continental ancestry group; Magnetic resonance imaging; Patellar dislocation; Tibia
中文摘要
華人成年人脛骨結節到滑車溝距離的正常值
文家潤、區嘉殷、曹君彥
目的
確定華人成年人的正常脛骨結節─滑車溝(TT-TG)距離,並確認磁共振成像(MRI)測量TT-TG 距離的可靠性和可重複性。
方法
我們對2015年1月至2016年1月的華人成人隊列中100例骨骼成熟膝關節的 MRI 掃描進行回顧研究。排除具有MRI或臨床證據提示曾經有髕骨外側脫位的患者。測量正常膝關節MRI掃描中的TT-TG距離。評估同一觀察者及不同觀察者間測量的一致性。
結果
研究結果顯示華人成人TT-TG距離的平均正常值為10.36 ± 2.52毫米(男性10.92 ± 2.59毫米,女性9.67 ± 2.28毫米)。同一觀察者及不同觀察者以MRI測量TT-TG距離均有優異的一致性。
結論
本研究可為未來華人成年人群中 TT-TG距離與髕骨不穩關係的研究奠定基礎。
INTRODUCTION
The amount of lateralisation of the tibial tubercle relative
to the trochlear groove has been termed the tibial tubercle
to trochlear groove (TT-TG) distance and has become a
useful tool in guiding surgical management of patients
with recurrent patellar instability. There are multiple
studies describing the measurement of TT-TG distance
using various modalities such as X-ray, computed
tomography (CT), and magnetic resonance imaging
(MRI).[1] [2] [3] [4] [5] [6] [7] [8] [9] However, to the best of our knowledge, the
TT-TG distance is not well documented in the adult
Chinese population. A previous study compared the
TT-TG distance in Chinese patients with or without
recurrent patellar dislocation using MRI,[10] but there was
no clear definition of a normal control knee.
The aim of the present study was to report normal values
of the TT-TG distance in normal skeletally mature adult
Chinese knees and to assess the reliability of MRI in
measuring TT-TG distance.
METHODS
Study Population
We retrospectively reviewed 125 MRI scans of
skeletally mature knees, which were retrieved using the
dedicated Radiology Information System, from January
2015 to January 2016. Cases recruited in this study had
undergone MRI due to knee pain or suspected internal
knee derangement.
Inclusion criterion was an intact patellofemoral joint
on arthroscopy. Exclusion criteria were ≥3 of the
following: MRI or clinical evidence of previous lateral
patellar dislocation, characterised by joint effusion,
contusion of the lateral femoral condyle/medial patellar
facet, osteochondral fragments; or injury to the medial
ligamentous stabilisers, the medial retinaculum, and the
medial patellofemoral ligament.[8] We also excluded MRI
scans showing any ligamentous injury or any internal
derangement of the knee, other than meniscal injury. For
clinical criteria, cases of documented patellar dislocation requiring reduction by a physician, or a convincing
history of giving way along with clinical findings of joint
effusion and tenderness along the medial patella facet,
along the medial retinaculum, and/or the medial femoral
condyle were excluded.[8] We also excluded MRI scans of
those individuals who, on clinical examination, showed
signs and symptoms of patellofemoral instability,
ligamentous laxity, malalignment, or osteoarthritis, as this
may give abnormal measurement of the TT-TG distance.[7] [11]
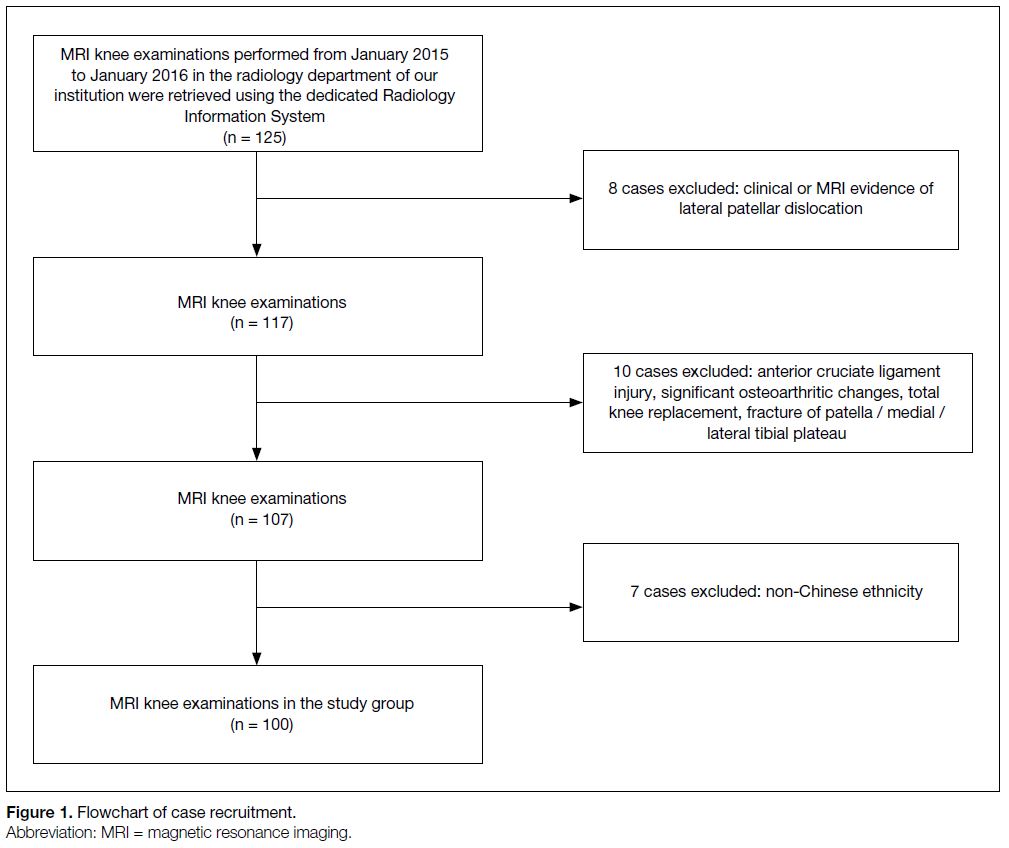
Eight cases showed clinical or MRI evidence of lateral
patellar dislocation. Ten cases were excluded due to
presence of anterior cruciate ligament injury, significant
osteoarthritic changes, total knee replacement, or fracture
of the patella or of the medial or lateral tibial plateau.
Seven patients were excluded due to non-Chinese
ethnicity (Figure 1).
Figure 1. Flowchart of case recruitment.
These criteria were used to identify 100 cases, which
formed the study group. The institutional research ethics
committee approved this investigation. Written consent
was waived as it was retrospective.
Magnetic Resonance Imaging Technique
The MRI examinations were performed on a 1.5-T
imager (MAGNETOM Avanto 1.5T; Siemens, Erlangen,
Germany). The patients underwent imaging in the supine
position with the knee in full extension. A proton-density
weighted turbo spin-echo with fat suppression imaging
sequence (TR/TE, 3500/20 ms; flip angle, 150°; field of
view, 256 × 256 mm; section thickness, 4.0 mm) was
routinely acquired and used for this study.
Tibial Tubercle to Trochlear Groove
Distance Measurement
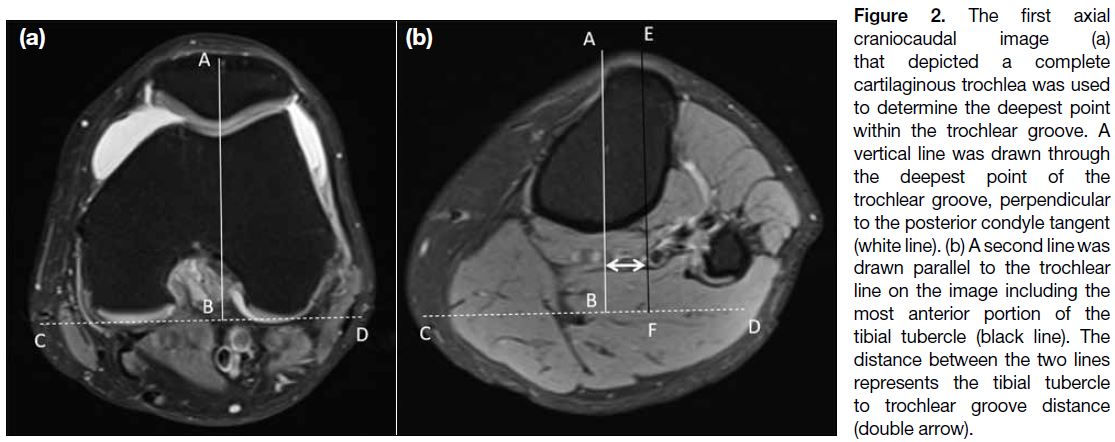
Axial images were used to measure the TT-TG
distance in all individuals. The TT-TG distance was
measured in accordance with the technique described by
Schoettle et al[5] (Figure 2). All readings were done using
OsiriX software, which runs on Macintosh system
(Apple Inc. Cupertino [CA], United States).
Figure 2. The first axial
craniocaudal image (a) that depicted a complete cartilaginous trochlea was used to determine the deepest point within the trochlear groove. A vertical line was drawn through the deepest point of the trochlear groove, perpendicular to the posterior condyle tangent (white line). (b) A second line was drawn parallel to the trochlear line on the image including the most anterior portion of the tibial tubercle (black line). The distance between the two lines represents the tibial tubercle to trochlear groove distance (double arrow).
The measurement of TT-TG distance was done by
two independent radiologists with special interest in
musculoskeletal radiology. Each TT-TG distance was
measured twice by each radiologist (raters A and B) on
two different occasions and in randomised order. The
radiologists were blinded to patient age, sex, diagnosis,
their previous measurement, and the measurements of
the other reader.
Statistical Analysis
All analyses were undertaken using commercial software
SPSS (Windows version 22.0; IBM Corp, Armonk
[NY], United States). We were interested in estimating
the mean TT-TG distance in this adult group at a 95%
confidence interval (95% CI) with a maximum error
of 1 mm. The standard deviation based on a study was
3.1 mm.[7] An estimated sample size of at least 37 would be
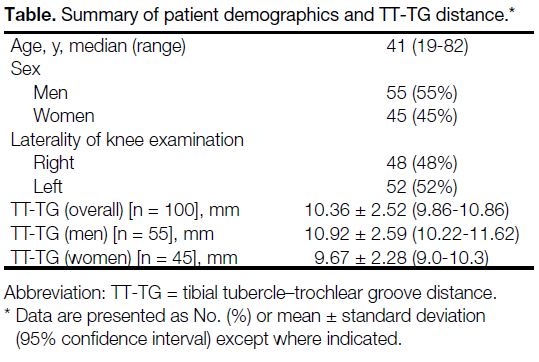
needed. Descriptive statistics for TT-TG distance of men
and women were calculated (Table); an independent t test
was used to detect any significant differences between
the two values. An intraclass correlation coefficient
was used to evaluate intraobserver and interobserver
reliability of the MRI measurements. A p value of < 0.05
was considered statistically significant.
Table. Summary of patient demographics and TT-TG distance.
RESULTS
Total 100 cases were included. The median age of the
cohort was 41 years (range, 19-82 years). Preliminary
analysis confirmed that the TT-TG measurements
had a normal distribution. Mean TT-TG distance
for this adult Chinese cohort was 10.36 ± 2.52 mm,
95% CI = 9.86-10.86 mm). The mean TT-TG distance
was 10.92 ± 2.59 mm for men and 9.67 ± 2.28 mm for
women (p = 0.013).
Intraclass correlation coefficients for intraobserver and
interobserver reliability were excellent. Intraobserver reliability for raters A and B at two different time
points was 0.993 (95% CI = 0.990-0.995) and 0.983
(95% CI = 0.975-0.989), respectively, p < 0.001.
Respective interobserver reliability was 0.961 (95% CI = 0.943-0.974) and 0.967 (95% CI = 0.952-0.978),
p < 0.001.
DISCUSSION
Both CT and MRI can accurately measure TT-TG
distance; however, MRI study has several advantages
over CT scan study as it is free of radiation hazards and
can also evaluate cartilage damage as a result of recurrent
patellar dislocations.[5] [7]
Different studies reported wide range of normal TT-TG
values. For instance, Wittstein et al[3] found it as
9.4 ± 0.6 mm, Pandit et al[4] found it as 9.91 mm in
men and 10.04 mm in women, Kulkarni et al[7] found it
as 13.19 ± 3.14 mm in men and 14.07 ± 3.03 mm in
women in an Indian population. Tse et al[10] found it as
12.7 ± 3.4 mm. In our study, the mean normal value of
the TT-TG distance in an adult Chinese population was
found to be 10.36 ± 2.52 mm (10.92 ± 2.59 mm for men
and 9.67 ± 2.28 mm for women).
In Caucasian populations, the cut-off value of TT-TG
distance for tibial tuberosity transfer is 20 mm.[1] It is not
certain if an absolute value is applicable to all patients,
with different sex and ethnicity. The threshold for tibial
tuberosity transfer may be lower in Chinese patients.[10]
Further study is required to better define the cut-off
value, and its relationship with patellar instability and
body size metrics in the Chinese population.
Our study also confirmed that MRI measurements
of TT-TG distances in the adult Chinese population
were reliable and reproducible. There was excellent
intraobserver and interobserver reliability in our study.
CONCLUSION
Our study defined normal MRI measurements of the TT-TG
distance in an adult Chinese population. We believe
that this study could form the basis for further research
to study the association between TT-TG distance and
patellar instability in the adult Chinese population.
REFERENCES
1. Goutallier D, Bernageau J, Lecudonnec B. The measurement of the
tibial tuberosity. Patella groove distanced technique and results [in
French]. Rev Chir Orthop Reparatrice Appar Mot. 1978;64:423-8.
2. Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar
instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2:19-26. Crossref
3. Wittstein J, Bartlett E, Easterbrook J, Byrd JC. Magnetic resonance imaging evaluation of patellofemoral malalignment. Arthroscopy.
2006;22:643-9. Crossref
4. Pandit S, Frampton C, Stoddart J, Lynskey T. Magnetic resonance imaging assessment of tibial tuberosity–trochlear groove distance: normal values for males and females. Int Orthop. 2011;35:1799-
803. Crossref
5. Schoettle PB, Zanetti M, Seifert B, Pfirrmann C, Fucentese S, Romero J. The tibial tuberosity–trochlear groove distance;
a comparative study between CT and MRI scanning. Knee.
2006;13:26-31. Crossref
6. Pennock AT, Alam M, Bastrom T. Variation in tibial tubercle–trochlear groove measurement as a function of age, sex, size, and patellar instability. Am J Sports Med. 2014;42:389-93. Crossref
7. Kulkarni S, Shetty AP, Alva KK, Talekar S, Shetty VD. Patellar instability in Indian population: relevance of tibial tuberosity and trochlear groove distance. SICOT J. 2016;2:14. Crossref
8. Balcarek P, Ammon J, Frosch S, Walde TA, Schüttrumpf JP, Ferlemann KG, et al. Magnetic resonance imaging characteristics
of the medial patellofemoral ligament lesion in acute lateral patellar
dislocations considering trochlear dysplasia, patella alta, and tibial
tuberosity–trochlear groove distance. Arthroscopy. 2010;26:926-
35. Crossref
9. Dickens AJ, Morrell NT, Doering A, Tandberg D, Treme G. Tibial tubercle–trochlear groove distance: defining normal in a pediatric population. J Bone Joint Surg Am. 2014;96:318-24. Crossref
10. Tse MS, Lie CW, Pan NY, Chan CH, Chow HL, Chan WL. Tibial tuberosity–trochlear groove distance in Chinese patients with or
without recurrent patellar dislocation. J Orthop Surg (Hong Kong).
2015;23:180-1. Crossref
11. Balcarek P, Jung K, Frosch KH, Stürmer KM. Value of the tibial
tuberosity–trochlear groove distance in patellar instability in the
young athlete. Am J Sports Med. 2011;39:1756-61. Crossref