Painless Asymptomatic Ascending Aortic Dissection with Four-Dimensional Flow Magnetic Resonance Imaging: a Case Report
CASE REPORT
Painless Asymptomatic Ascending Aortic Dissection with Four-Dimensional Flow Magnetic Resonance Imaging: a Case Report
JCY Chan1, SY Fung2, OH Ching2, KC Lee3, CW Cheung1, MY Ng4
1 Department of Radiology, Queen Mary Hospital, Hong Kong
2 Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong
3 Department of Medicine, Ruttonjee Hospital, Hong Kong
4 Department of Diagnostic Radiology, The University of Hong Kong, Hong Kong
Correspondence: Dr JCY Chan, Department of Radiology, Queen Mary Hospital, Hong Kong. Email: johnchancy93@gmail.com
Submitted: 29 Mar 2020; Accepted: 18 May 2020.
Contributors: JCYC and MYN designed the study. JCYC, SYF, OHC and MYN acquired the data. All authors analysed the data. JCYC, KCL
and MYN drafted the manuscript. JCYC, CWC and MYN critically revised the manuscript for important intellectual content. All authors had full
access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of Interest: All authors have disclosed no conflicts of interest.
Funding/Support: This work was generously supported by the Health and Medical Research Fund (05162736).
Ethics Approval: The patient was treated in accordance with the tenets of the Declaration of Helsinki. The patient provided written informed
consent for all treatments and procedures.
INTRODUCTION
Aortic dissection is an uncommon condition with a high
mortality.[1] [2] Over 90% of cases present with severe chest
or back pain.[1] [2] [3] Other presenting symptoms include
syncope, focal neurological deficits, paraplegia, or
symptoms of congestive heart failure.[1] [3] [4] We present an
extremely rare case of asymptomatic ascending aortic
dissection discovered incidentally during scheduled
cardiac magnetic resonance imaging (MRI) for research
purposes.
CASE REPORT
A 57-year-old man, non-smoker, with hyperlipidaemia
and hypertension on 5 mg amlodipine orally once daily,
participated in a cardiac MRI research programme at
The University of Hong Kong. He had no history of
connective tissue disorders such as Marfan or Ehlers–Danlos syndrome. Initial cardiac MRI in July 2017
revealed a dilated ascending thoracic aorta measuring
4.4 cm in diameter, moderate aortic regurgitation and
normal left ventricular systolic function. No intimal
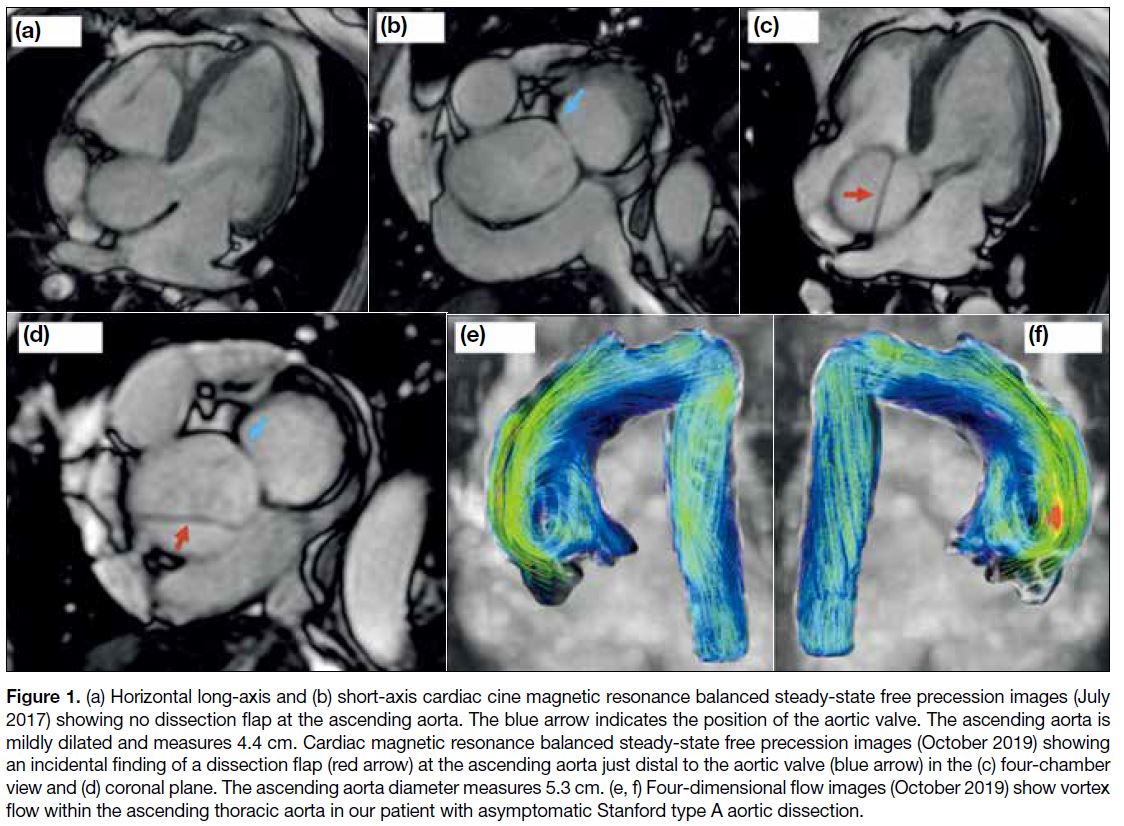
flap was seen in this initial study (Figure 1a and b). A further research cardiac MRI in October 2019 revealed
a new incidental finding of a focal dissection flap in
the ascending thoracic aorta consistent with a Stanford
type A aortic dissection (Figure 1c and d). There was
an increase in the diameter of the ascending thoracic
aorta to 5.3 cm and moderate/severe aortic regurgitation
with normal left ventricular systolic function. There
was no haemopericardium or para-aortic haematoma.
Four-dimensional (4D) flow imaging demonstrated
vortex formation within the ascending aorta indicative
of altered flow dynamics unlike the typical laminar flow
seen in normal aortas (Figure 1e and f).
Figure 1. (a) Horizontal long-axis and (b) short-axis cardiac cine magnetic resonance balanced steady-state free precession images (July
2017) showing no dissection flap at the ascending aorta. The blue arrow indicates the position of the aortic valve. The ascending aorta is
mildly dilated and measures 4.4 cm. Cardiac magnetic resonance balanced steady-state free precession images (October 2019) showing
an incidental finding of a dissection flap (red arrow) at the ascending aorta just distal to the aortic valve (blue arrow) in the (c) four-chamber
view and (d) coronal plane. The ascending aorta diameter measures 5.3 cm. (e, f) Four-dimensional flow images (October 2019) show vortex
flow within the ascending thoracic aorta in our patient with asymptomatic Stanford type A aortic dissection.
The patient was immediately contacted and advised to
attend the emergency department. On admission, he
was asymptomatic. His latest exercise tolerance was
excellent, and he had just competed in a 10-km run.
His blood pressure measured at home was stable at
<140 mmHg/<85 mmHg. On examination, his vital signs
were normal with blood pressure 130 mmHg/80 mmHg,
heart rate 80 bpm, respiratory rate 16/minute, and SpO2
95%. Heart sounds were normal with an early diastolic murmur. There was no radio-radial delay on either arm
or blood pressure discrepancy between arms. Blood tests
(including complete blood count, liver and renal function
profile, clotting profile, troponin, and creatinine kinase)
were unremarkable. Echocardiogram demonstrated
sinus rhythm with no acute ischaemic changes. A
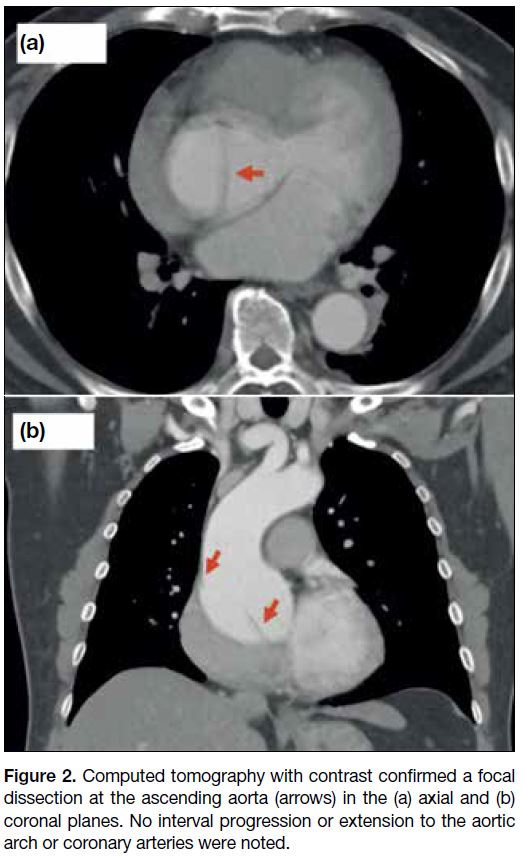
computed tomography aortogram was performed 5 days
after the incidental finding to confirm and evaluate the
extent of the dissection. A static focal dissection flap in
the ascending thoracic aorta without extension to the
aortic arch or coronary arteries was confirmed (Figure 2a
and b). There was no aortic intramural haematoma or
penetrating atherosclerotic ulcer. Echocardiography
confirmed moderate aortic regurgitation but no aortic
stenosis. The patient underwent an open-heart aortic
root replacement and aortic valve valvuloplasty 20 days
after the incidental MRI finding of Stanford type A
aortic dissection. Postoperative recovery was uneventful
and the patient was discharged home. Postoperative
echocardiogram showed no valvular stenosis or regurgitation. The patient was well and asymptomatic at
the last outpatient follow-up, 78 days after surgery.
Figure 2. Computed tomography with contrast confirmed a focal
dissection at the ascending aorta (arrows) in the (a) axial and (b)
coronal planes. No interval progression or extension to the aortic
arch or coronary arteries were noted.
DISCUSSION
Aortic dissection is an uncommon but often fatal
condition with an annual incidence of 2.9 per 100,000
population.[1] [2] [4] Although approximately 6.4% of
patients present with painless aortic dissection,[4] there
is no recognised literature describing the incidence of
asymptomatic presentation.
There are multiple proposed mechanisms of painless
aortic dissection, including: less wall stretching
due to slow dissection; sparing of the adventitial
dissection; damaged aortic wall sensation due to prior
cardiovascular surgery or known aortic aneurysm;
degeneration or denervation of periaortic pain receptors
in the elderly patients or patients with diabetes mellitus;
and cerebral insult (ischaemic stroke or syncope) leading
to attenuation of pain perception.[4]
Painless aortic dissections typically present with other
symptoms and include syncope, symptoms of congestive
heart failure, focal neurological deficit, or paraplegia.[1] [3] [4]
These symptoms are usually due to extension of the
dissection into other structures or vessels, e.g., aortic
valve, coronary arteries, common carotid arteries, and
intercostal arteries.
Painless aortic dissection has an older mean age (67 vs.
61 years) at presentation and is more common in the
presence of diabetes (10.2% vs. 4.0%), aortic aneurysm
(29.5% vs. 13.1%), and prior cardiovascular surgery
(48.1% vs. 19.7%).[4] Our patient was unusual in that he
was younger and generally of good health with no history
of diabetes or connective tissue disorders. However,
he did have a mildly dilated ascending aorta of 4.4 cm
although his hypertension was well controlled. He had
no neurological symptoms or deficit. Aortic stenosis was not evident on echocardiogram. After reviewing the first
MRI scan, we confirmed that the incidental finding of
focal type A aortic dissection was a novel development
between the first and second MRI rather than being
missed. We propose that the unusual presentation and
outcome in our case was due to early discovery of a focal
aortic dissection before progression or any complication
with subsequent prompt management.
Despite being described in a previous case report,[5]
asymptomatic ascending aortic dissection is extremely
rare, likely because patients with completely
asymptomatic ascending aortic dissection do not present
to medical services until complications arise.
In this case, the diagnosis was based on identifying the
dissection flap on the cine images. The 4D flow images
did not alter the diagnosis or patient management per se.
The patient’s 4D flow images demonstrated turbulent
flow in the aortic aneurysm and dissection that has
been commonly described.[6] [7] The clinical application of
4D flow MRI is becoming increasingly clear. In cases
of aortic stenosis, studies have demonstrated that 4D
flow is better in measuring the peak velocity compared
with traditional two-dimensional flow which is operator
dependent. It provides better understanding of altered
aortic blood flow and regional wall shear stress in the
expression of an aortopathy phenotype.[8] [9] [10] Moreover,
4D flow is particularly useful in patients with congenital
heart disease before and after operation where multiple
two-dimensional flow measurements are routinely
required in highly complex and abnormal anatomy
that is challenging, even in the most experienced
hands.[9] 4D flow can potentially save time by acquiring
a whole volume dataset and allowing the experienced
cardiothoracic radiologist to perform post-processing
in exchange for longer scanning time. Lastly, 4D flow
provides information about intracardiac blood flow
that was previously not possible (e.g., amount of flow
travelling directly from the atrium to the ventricle and
out into the aorta in a single cardiac cycle) and is an area
under investigation.[9]
REFERENCES
1. Golledge J, Eagle KA. Acute aortic dissection. Lancet. 2008;372:55-66. Crossref
2. Mészáros I, Mórocz J, Szlávi J, Schmidt J, Tornóci L, Nagy L, et al. Epidemiology and clinicopathology of aortic dissection. Chest.
2000;117:1271-8. Crossref
3. Pape LA, Awais M, Woznicki EM, Suzuki T, Trimarchi S,
Evangelista A, et al. Presentation, diagnosis, and outcomes of acute
aortic dissection: 17-Year trends from the International Registry of Acute Aortic Dissection. J Am Coll Cardiol. 2015;66:350-8. Crossref
4. Park SW, Hutchison S, Mehta RH, Isselbacher E, Cooper JV, Fang J, et al., Association of painless acute aortic dissection with
increased mortality. Mayo Clin Proc. 2004;79:1252-7. Crossref
5. Cohen R, Mena D, Carbajal-Mendoza R, Arole O, Mejia JO. A case report on asymptomatic ascending aortic dissection. Int J Angiol
2008;17:155-61. Crossref
6. François CJ, Markl M, Schiebler ML, Niespodzany E, Landgraf BR, Schlensak C, et al. Four-dimensional, flow-sensitive
magnetic resonance imaging of blood flow patterns in thoracic
aortic dissections. J Thorac Cardiovasc Surg. 2013;145:1359-66. Crossref
7. Weigang E, Kari FA, Beyersdorf F, Luehr M, Etz CD, Frydrychowicz A, et al. Flow-sensitive four-dimensional magnetic resonance imaging: flow patterns in ascending aortic aneurysms.
Eur J Cardiothorac Surg. 2008;34:11-6. Crossref
8. Garcia, J, Barker AJ, Markl M. The role of imaging of flow patterns by 4D flow MRI in aortic stenosis. JACC Cardiovasc Imaging.
2019;12:252-66. Crossref
9. Azarine A, Garçon P, Stansal A, Canepa N, Angelopoulos G,
Silvera S, et al. Four-dimensional flow MRI: principles and
cardiovascular applications. Radiographics. 2019;39:632-48. Crossref
10. Rodríguez-Palomares JF, Dux-Santoy L, Guala A, Kale R, Maldonado G, Teixidó-Turà G, et al. Aortic flow patterns and wall
shear stress maps by 4D-flow cardiovascular magnetic resonance in
the assessment of aortic dilatation in bicuspid aortic valve disease.
J Cardiovasc Magn Reason. 2018;20:28. Crossref