Imaging Features and Techniques in Assessment of Cleft Palate: a Pictorial Essay
PICTORIAL ESSAY
Imaging Features and Techniques in Assessment of Cleft Palate: a Pictorial Essay
AWT Chin, KS Tse, HC Lee, YW Hon, KL Lo
Department of Radiology and Organ Imaging, United Christian Hospital, Hong Kong
Correspondence: Dr AWT Chin, Department of Radiology and Organ Imaging United Christian Hospital, Kwun Tong, Hong Kong. Email: anthonywtchin@gmail.com
Submitted: 20 Feb 2019; Accepted: 11 Apr 2019.
Contributors: All authors contributed to the concept or design, acquisition of data, analysis or interpretation of data, drafting of the manuscript,
and critical revision for important intellectual content. All authors had full access to the data, contributed to the study, approved the final version
for publication, and take responsibility for its accuracy and integrity.
Conflicts of Interest: The authors have no conflicts of interest to disclose. All authors had full access to the data, contributed to the study,
approved the final version for publication, and take responsibility for its accuracy and integrity.
Funding/Support: This pictorial essay received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics Approval: Ethics approval and need for patient consent for this pictorial essay was waived by the ethics committee of the Hospital
Authority, Hong Kong.
INTRODUCTION
Cleft lip and palate deformities occur in around 1
in 600 live births in Hong Kong.[1] Our institution has
been offering a one-stop territory-wide integrated
multidisciplinary service to manage patients with
complicated cleft deformities within Hong Kong.[2] The
normal palate arises in utero from fusion of the primary
and secondary palates and should occur at around
4 to 6 weeks gestation and 8 to 12 weeks gestation,
respectively. Failure of fusion may cause cleft lip and / or cleft palate depending on the severity.[3] Cleft palate
may be one of the manifestations of clinical syndromes
such as Pierre Robin sequence. In such patients, there
will be additional faciocranial manifestations.
The levator veli palatini muscles help retract the velum
(soft palate) to allow separation of the nasopharynx
from the oropharynx by complete coverage of the soft
palate against the posterior pharyngeal wall. Patients
with cleft palate have abnormalities of the levator veli
palatini muscle, resulting in suboptimal velopharyngeal
closure, known as velopharyngeal insufficiency. This
causes hypernasality that impairs speech development.
In the past, nasoendoscopy and videofluoroscopy were used to assess velopharyngeal anatomy. However,
nasoendoscopy is invasive as it involves placement of
an endoscope into the pharyngeal region and may cause
patient anxiety and discomfort, especially in children.[4]
In addition, videofluoroscopy, as with other fluoroscopic
studies, has inherent measurement errors that may vary
with patient positioning.[4] With the advances in cross-sectional
imaging modalities including computed
tomography (CT) and magnetic resonance imaging
(MRI), non-invasive assessment of bony anatomy and
velopharyngeal musculature with easily reproducible
anatomy and measurements is now feasible. Preoperative
imaging assessment assists paediatric and maxillofacial
surgeons in surgical management.
In this pictorial essay, we describe technical
considerations in imaging and highlight the relevant
radiological anatomy and pathological features in CT
and MRI in the assessment of patients with cleft palate.
PATIENT PREPARATION
We aim to perform CT and MRI studies, whenever
possible, without sedation. The images used here have
been obtained from patients without sedation. When performing imaging studies in children, it is crucial to
strike a balance between the risk of motion artefacts
that can occur in the absence of sedation and altered
muscle tone that occurs with sedation. Currently, there
is no available evidence to show how sedation affects
cleft palate measurements. A recent study by Ali et al[5]
revealed that velopharyngeal dimensions obtained from
static MRI correlate with speech data, and it included
children who had been sedated. Uncooperative paediatric
patients are given light sedation with oral chloral hydrate
just before imaging to prevent motion artefacts. It is
clearly stated in radiology reports if sedation has been
given. In most of our cases we obtained CT and MRI
images without patient sedation.
Before examination, patients were clearly instructed to
breathe through their nose and remain at rest without
speech or swallowing. Patients undergoing MRI wore
an MR-compatible headset so radiographers could
communicate with them. Cushions and foams were used
to stabilise the patients in a supine position to minimise
motion during scanning.
COMPUTED TOMOGRAPHY
Plain CT is usually performed for patients with
complicated or syndromic cleft palate such as Pierre
Robin sequence to better assess bony detail and facilitate
three-dimensional (3D) printing for preoperative
planning. Our centre uses a 64-detector single-source
CT scanner (LightSpeed VCT; GE Healthcare, Chicago
[IL], United States). Plain CT from the skull base to
the entire mandible is performed. Helical mode is used
during scanning. Depending on the patient’s body
habitus, CT studies in older children adopt 120 kVp,
164 mAs and pitch of 0.984. These images are obtained
in axial acquisition at 5-mm thickness, and reformatted
to 0.62-mm slices. For young children and infants, CT
studies adopt 80 kVp, 125 mAs and pitch of 0.968.
These images are obtained in axial acquisition at 2.5-mm slice thickness. Multiplanar reformatted images are
used to better demonstrate bone anatomy and perform
measurements. Patients are imaged in a supine position.
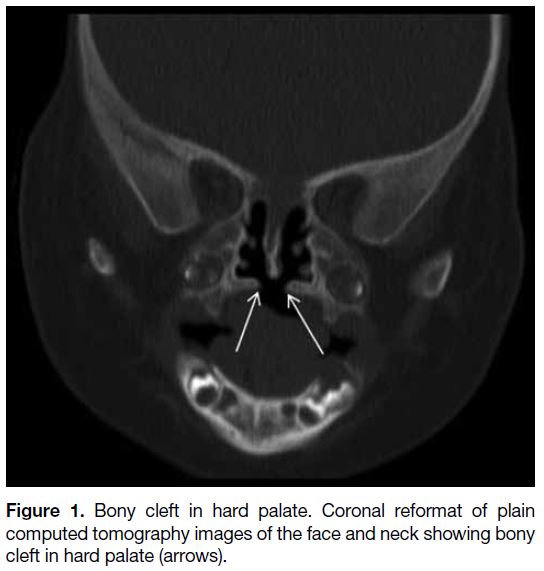
Normally the hard palate should be intact without any
defect. In the case of cleft palate, there will be bony defect
within the hard palate (Figure 1). In cases of Pierre Robin
sequence, cleft palate is associated with micrognathia
and glossoptosis and requires additional correction
procedures such as mandibular distraction osteogenesis.[6]
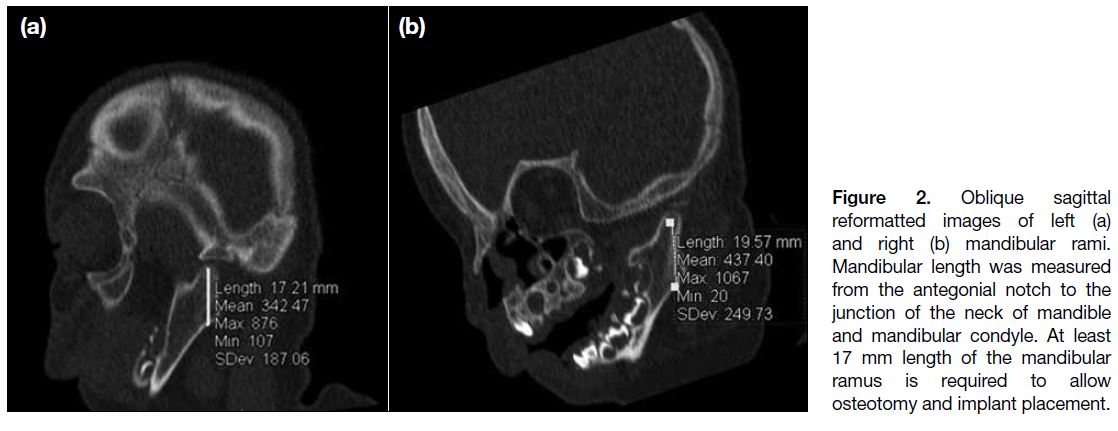
Size, shape, and symmetry of the mandible can be
well assessed. Length of the mandibular ramus can be measured using sagittal oblique reformatted images
(Figure 2). At least 17 mm length of the mandibular
ramus is required to allow osteotomy and implant
placement.[6] Identification of the inferior alveolar nerve
foramina is important to avoid nerve damage during
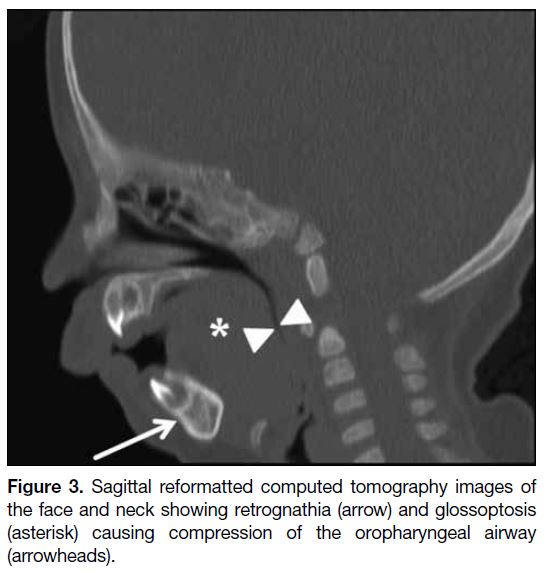
osteotomy or pin insertion.[6] The degree of airway
obstruction can also be assessed (Figure 3).
Figure 1. Bony cleft in hard palate. Coronal reformat of plain
computed tomography images of the face and neck showing bony
cleft in hard palate (arrows).
Figure 2. Oblique sagittal
reformatted images of left (a) and right (b) mandibular rami. Mandibular length was measured from the antegonial notch to the junction of the neck of mandible and mandibular condyle. At least 17 mm length of the mandibular ramus is required to allow osteotomy and implant placement.
Figure 3. Sagittal reformatted computed tomography images of
the face and neck showing retrognathia (arrow) and glossoptosis
(asterisk) causing compression of the oropharyngeal airway
(arrowheads).
MAGNETIC RESONANCE IMAGING
Our institution performs static MRI of the face and neck
for patients with complicated cleft palate and those
with primary correction failure. Our institution uses a
1.5-tesla MRI scanner (MAGNETOM Aera; Siemens,
Erlangen, Germany) for all scans. A 20-channel
cable-less Siemens head and neck coil are used during
scanning. At the commencement of MRI study, we first
acquire localiser images with fast gradient echo sequence
within a few seconds. We then acquire T2-weighted
images using turbo spin echo (TSE) technique. The
sequences acquired include T2 3D SPACE (sampling
perfection with application optimised contrasts using
different flip angle evolutions) coronal, T2 TSE sagittal,
T2 TSE coronal, and T2 TSE oblique coronal images.
The T2 3D SPACE coronal sequence is performed first
including the vertex of the skull and the entire mandible.
With the help of this sequence, we select a plane parallel
to the long axis of the levator veli palatini muscles,
to obtain the T2 TSE oblique coronal images. This specific oblique coronal plane allows better anatomical
depiction of the levator veli palatini muscles. The T2
3D SPACE coronal sequence is also used to generate
multiplanar reformatted images in the axial plane for
anatomical correlation of velopharyngeal structures.
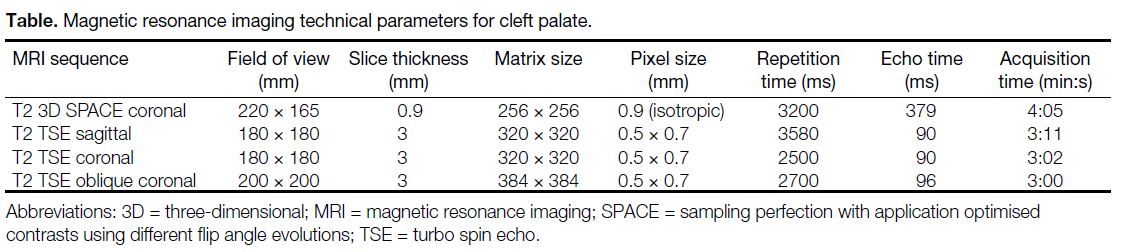
The Table illustrates the detailed technical parameters.
Only T2-weighted sequences without fat suppression are
obtained as the presence of fat allows better depiction of
various anatomical structures.
Table. Magnetic resonance imaging technical parameters for cleft palate.
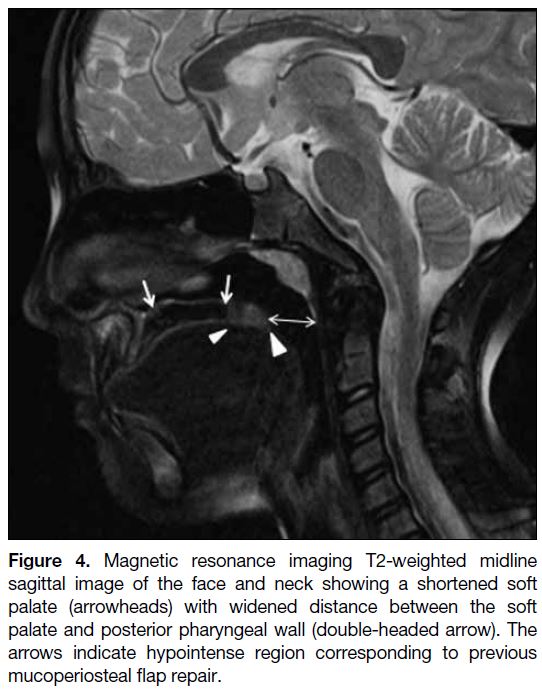
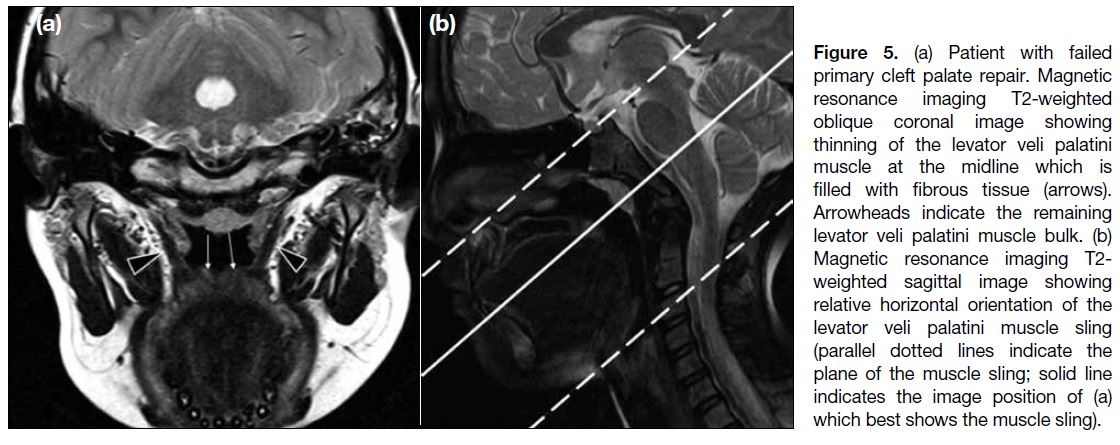
In patients with primary cleft palate and those with
failed primary repair, the soft palate appears shortened
with a widened distance between the soft palate and
posterior pharyngeal wall (Figure 4). The levator veli
palatini muscle sling appears thinned with loss of normal muscle signal in the midline, which is filled with fibrous
tissue. The levator veli palatini muscle also lies along a
relatively horizontal plane, leading to ineffective muscle
contraction and velopharyngeal insufficiency (Figures 5
and 6).
Figure 4. Magnetic resonance imaging T2-weighted midline
sagittal image of the face and neck showing a shortened soft
palate (arrowheads) with widened distance between the soft
palate and posterior pharyngeal wall (double-headed arrow). The
arrows indicate hypointense region corresponding to previous
mucoperiosteal flap repair.
Figure 5. a) Patient with failed
primary cleft palate repair. Magnetic resonance imaging T2-weighted oblique coronal image showing thinning of the levator veli palatini muscle at the midline which is filled with fibrous tissue (arrows). Arrowheads indicate the remaining levator veli palatini muscle bulk. (b) Magnetic resonance imaging T2-weighted sagittal image showing relative horizontal orientation of the levator veli palatini muscle sling (parallel dotted lines indicate the plane of the muscle sling; solid line indicates the image position of (a) which best shows the muscle sling).
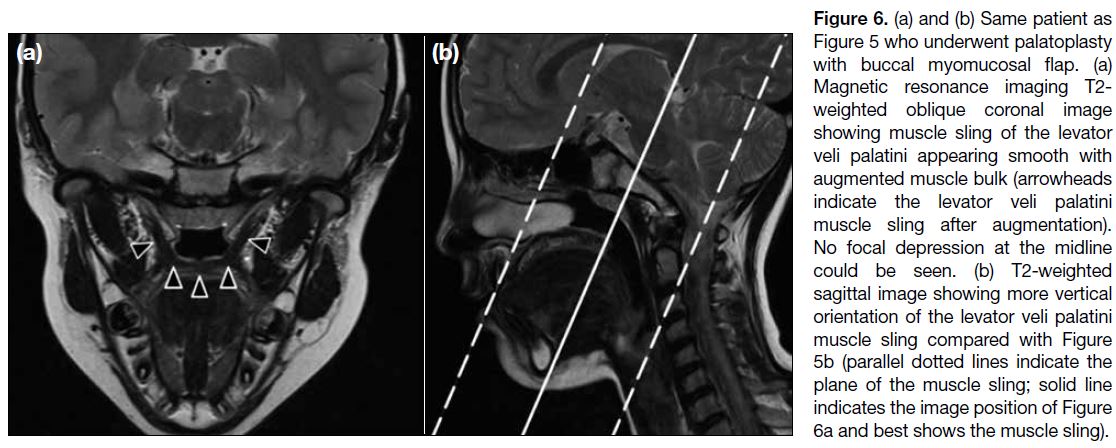
Figure 6. (a) and (b) Same patient as
Figure 5 who underwent palatoplasty with buccal myomucosal flap. (a) Magnetic resonance imaging T2-weighted oblique coronal image showing muscle sling of the levator veli palatini appearing smooth with augmented muscle bulk (arrowheads indicate the levator veli palatini muscle sling after augmentation). No focal depression at the midline could be seen. (b) T2-weighted sagittal image showing more vertical orientation of the levator veli palatini muscle sling compared with Figure 5b (parallel dotted lines indicate the plane of the muscle sling; solid line indicates the image position of Figure 6a and best shows the muscle sling).
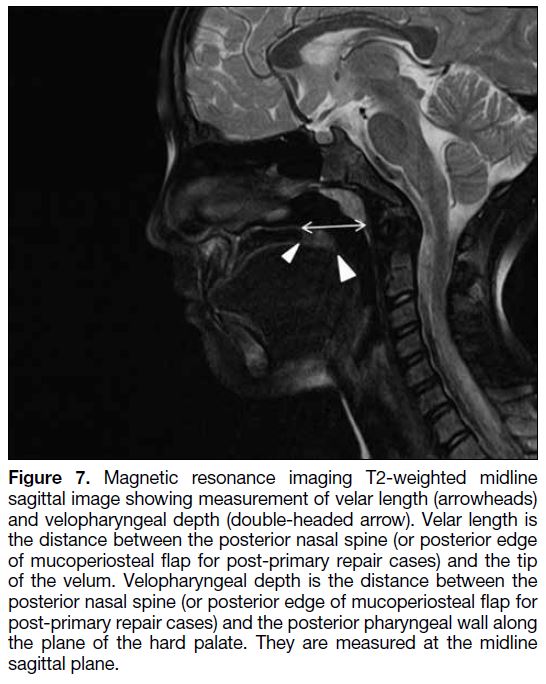
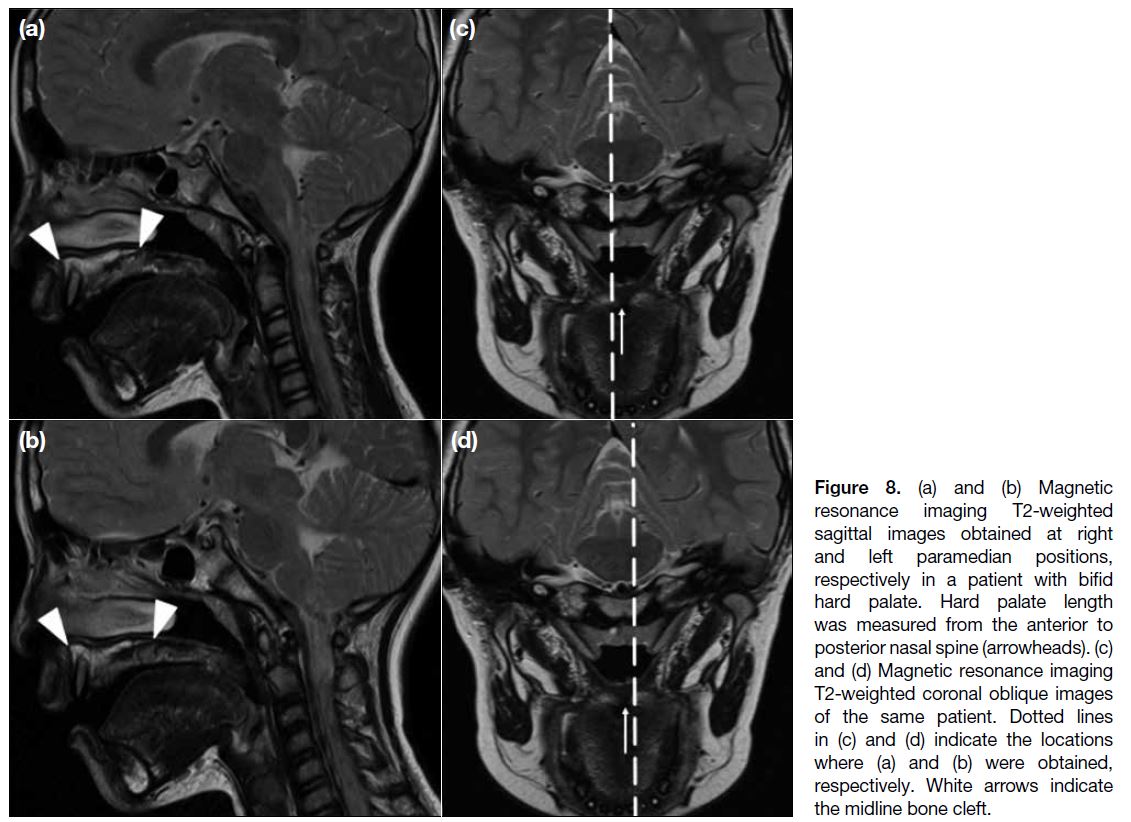
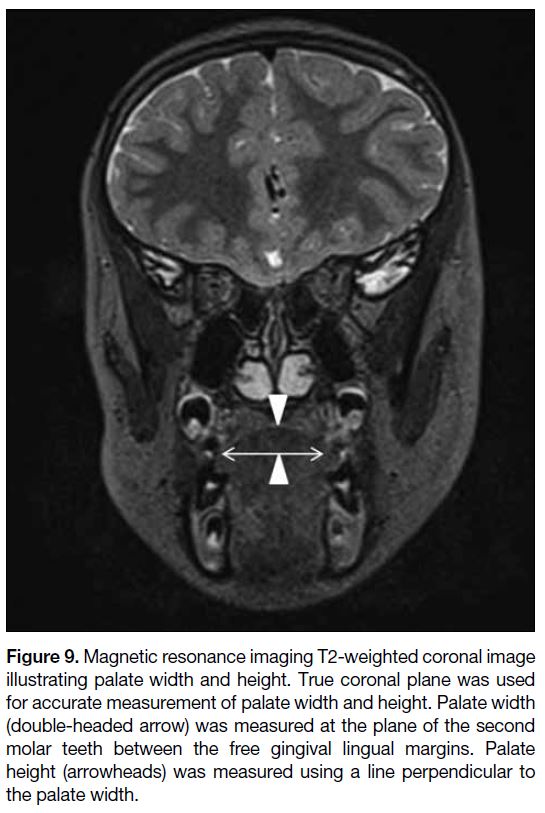
Various measurements of velopharyngeal structures may
be obtained, including hard palate length, velar length,
velopharyngeal depth, palate width, and palate height
(Figures 7 8 and 9). Previous studies have evaluated the
range of values of velopharyngeal structures in normal
subjects.[4] Nonetheless, methods used to measure these
parameters vary among studies, as do reference values
and most include only a small number of patients.[4] We
believe that providing the various measurements as a guide for surgeons is sufficient without the need to
determine whether the different parameters follow a
particular reference range. Surgical approaches include
Furlow double-opposing Z-plasty, augmentation
pharyngoplasty, pharyngeal flap surgery, and sphincter
palatoplasty.[7] According to Ruda et al,[7] choice of
treatment for velopharyngeal insufficiency depends on
numerous factors. These include symmetry and degree
of separation between the velum and pharynx, length of
the palate and configuration of velopharyngeal muscles
that can be assessed by MRI. A recent study by Ali et al[5]
demonstrated that static velopharyngeal measures on
MRI in patients with cleft palate correlated with their
speech performance. Velar length has been shown to
have a strong positive linear correlation with degree
of velar movement.[5] Velar thickness has a significant
moderate positive linear correlation with degree of
velar movement and overall intelligibility of speech.[5]
The measurements provided in this pictorial essay help
surgeons to select the most appropriate approach to
optimise velar coverage in separating the nasopharynx
and oropharynx during speech.
Figure 7. Magnetic resonance imaging T2-weighted midline
sagittal image showing measurement of velar length (arrowheads)
and velopharyngeal depth (double-headed arrow). Velar length is
the distance between the posterior nasal spine (or posterior edge
of mucoperiosteal flap for post-primary repair cases) and the tip
of the velum. Velopharyngeal depth is the distance between the
posterior nasal spine (or posterior edge of mucoperiosteal flap for
post-primary repair cases) and the posterior pharyngeal wall along
the plane of the hard palate. They are measured at the midline
sagittal plane.
Figure 8. (a) and (b) Magnetic
resonance imaging T2-weighted sagittal images obtained at right and left paramedian positions, respectively in a patient with bifid hard palate. Hard palate length was measured from the anterior to posterior nasal spine (arrowheads). (c) and (d) Magnetic resonance imaging T2-weighted coronal oblique images of the same patient. Dotted lines in (c) and (d) indicate the locations where (a) and (b) were obtained, respectively. White arrows indicate the midline bone cleft.
Figure 9. Magnetic resonance imaging T2-weighted coronal image
illustrating palate width and height. True coronal plane was used
for accurate measurement of palate width and height. Palate width
(double-headed arrow) was measured at the plane of the second
molar teeth between the free gingival lingual margins. Palate
height (arrowheads) was measured using a line perpendicular to
the palate width.
CONCLUSION
Preoperative imaging of the velopharyngeal apparatus
is crucial to facilitate operative management. Crosssectional
imaging allows non-invasive, accurate
assessment of velopharyngeal and bone anatomy
compared with other modalities. A multidisciplinary
team that involves paediatric surgeons, maxillofacial
surgeons, and radiologists is important for successful
treatment of patients with cleft palate deformities.
REFERENCES
1. Choi WK. Primary cleft lip and palate repair. HK Med Diary.
2018;23:7-14.
2. United Christian Hospital, Hospital Authority, Hong Kong SAR
Government. Cleft lip/cleft palate services. Hospital Authority,
Hong Kong. Available from: http://www3.ha.org.hk/uch/internet/show.aspx?p=spCleft. Accessed 31 Jan 2019.
3. Abramson ZR, Peacock ZS, Cohen HL, Choudhri AF. Radiology of
cleft lip and palate: imaging for the prenatal period and throughout
life. Radiographics. 2015;35:2053-63. Crossref
4. Perry JL, Sutton BP, Kuehn DP, Gamage JK. Using MRI for
assessing velopharyngeal structures and function. Cleft Palate
Craniofac J. 2014;51:476-85. Crossref
5. Ali A, El Shamy M, AbdElmonem A, Hamza F, El Banoby T.
Role of MRI in detection of repaired cleft palate muscles and
correlation to speech. Egypt J Hosp Med. 2018;73:7604-9.
6. Meyers AB, Zei, MG, Denny AD. Imaging neonates and children
with Pierre Robin sequence before and after mandibular distraction
osteogenesis: what the craniofacial surgeon wants to know. Pediatr
Radiol. 2015;45:1392-402. Crossref
7. Ruda JM, Krakovitz P, Rose AS. A review of the evaluation
and management of velopharyngeal insufficiency in children.
Otolaryngol Clin North Am. 2012;45:653-69, viii. Crossref
| Attachment | Size |
|---|---|
| v24n1_Imaging.pdf | 382.32 KB |