Post-lobectomy Lung Torsion: a Report of Two Cases
CASE REPORT
Post-lobectomy Lung Torsion: a Report of Two Cases
SH Liu, FY Wan, JB Chiang
Department of Radiology and Imaging, Queen Elizabeth Hospital, Hong Kong
Correspondence: Dr SH Liu, Department of Radiology and Imaging, Queen Elizabeth Hospital, Hong Kong. Email: calebliu@gmail.com
Submitted: 25 Nov 2019; Accepted: 2 Jan 2020.
Contributors: All authors designed the study, acquired the data, analysed the data, drafted the manuscript, and critically revised the manuscript
for important intellectual content. All authors had full access to the data, contributed to the study, approved the final version for publication, and
take responsibility for its accuracy and integrity.
Conflicts of Interest: All authors have disclosed no conflicts of interest.
Funding/Support: This case report received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics Approval: The patients were treated in accordance with the tenets of the Declaration of Helsinki. The patients provided written informed
consent for all treatments and procedures.
INTRODUCTION
Lung or lobar torsion can occur secondary to trauma
(eg, traumatic pneumothorax) spontaneously, or more
commonly after pulmonary surgery.[1] Lobar torsion
following pulmonary lobectomy is considered a rare
complication with an incidence of 0.09 to 0.4%.[2] Early
recognition is important because rapid deterioration
and death may result if the condition is not promptly
managed. In this report, we describe two cases of
postoperative lobar torsion that presented with non-specific
symptoms, subsequently diagnosed on contrast
computed tomography (CT).
CASE 1
A 49-year-old man underwent video-assisted
thoracoscopic right upper lobectomy and systemic
exploration of mediastinal lymph nodes for biopsy-proven
right upper lobe adenocarcinoma with right hilar and
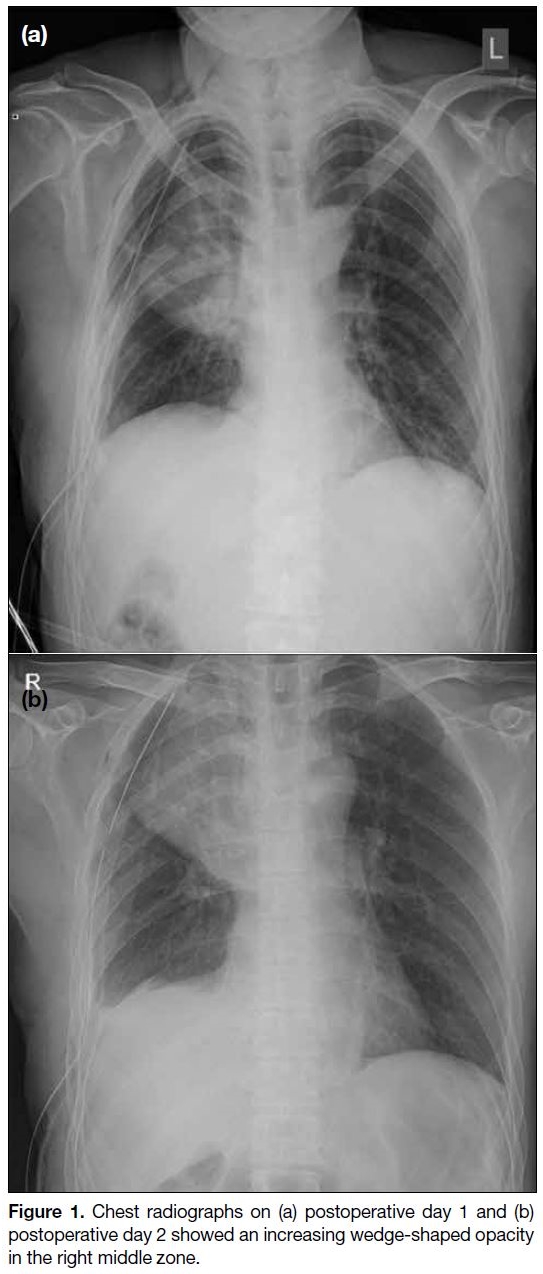
paratracheal lymph node involvement. Chest radiographs
on postoperative days 1 and 2 revealed increasing wedge-shaped
opacity in the right middle zone (Figure 1).
Bedside bronchoscopy on postoperative day 3 showed
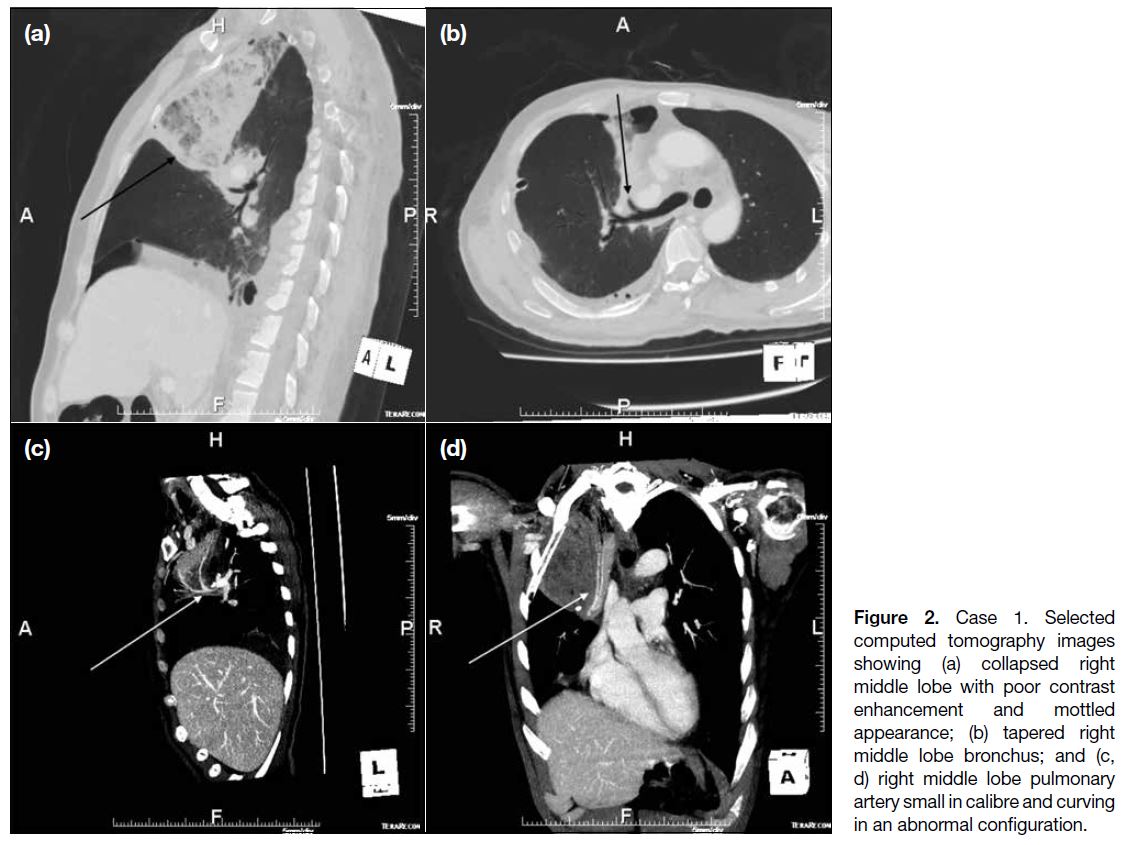
a tight orifice of the right middle lobe. Urgent CT scan
showed collapse consolidation of the right middle lobe
with poor contrast enhancement and mottled appearance
(Figure 2a). The right middle lobe bronchus appeared tapered with abrupt termination (Figure 2b). The right
middle lobe pulmonary artery also appeared small in
calibre and curved in an abnormal configuration (Figure 2c and d). With the suspicion of lung torsion, explorative
thoracotomy was performed. The right middle lobe was
found to be oedematous with a 90-degree clockwise
torsion along the pedicle axis. Emergency lobectomy
was performed with subsequent pathologic examination
showing marked haemorrhage in the alveolar spaces.
The patient was discharged 14 days after operation.
Figure 1. Chest radiographs on (a) postoperative day 1 and (b)
postoperative day 2 showed an increasing wedge-shaped opacity
in the right middle zone.
Figure 2. Case 1. Selected
computed tomography images showing (a) collapsed right middle lobe with poor contrast enhancement and mottled appearance; (b) tapered right middle lobe bronchus; and (c, d) right middle lobe pulmonary artery small in calibre and curving in an abnormal configuration.
CASE 2
A 64-year-old man underwent video-assisted
thoracoscopic right upper lobectomy for right upper lobe
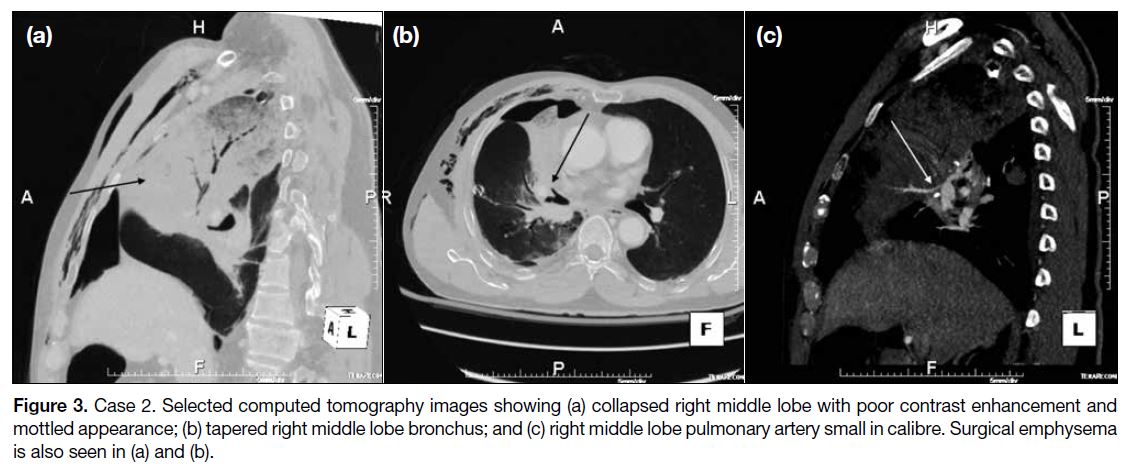
adenocarcinoma. Chest radiographs on postoperative
days 0 to 2 showed increasing opacity over the right mid
zone. Urgent CT scan revealed collapse consolidation
of the right middle lobe associated with poor contrast
enhancement and a mottled appearance (Figure 3a). The
right middle lobe bronchus appeared tapered (Figure 3b)
and the right middle lobe pulmonary artery appeared
small in calibre (Figure 3c). Surgical emphysema was also
noted (Figure 3a and b). Right middle lobe torsion was
suspected, and endoscopy confirmed the suspicion with
distortion of the right middle lobe distal bronchial tree.
Explorative thoracotomy revealed a markedly congested dusky right middle lobe with 180° clockwise rotation,
confirming a right middle lobe torsion. Emergency
lobectomy was performed and pathological examination
confirmed a haemorrhagic infarct. The patient was
discharged 12 days after the second operation.
Figure 3. Case 2. Selected computed tomography images showing (a) collapsed right middle lobe with poor contrast enhancement and
mottled appearance; (b) tapered right middle lobe bronchus; and (c) right middle lobe pulmonary artery small in calibre. Surgical emphysema
is also seen in (a) and (b).
DISCUSSION
CT has been increasingly used to aid diagnosis of lung or
lobar torsion. In postoperative lung torsion, patients may
initially be stable with non-specific symptoms and signs.
Twisting of the bronchovascular pedicle may lead to
pulmonary or lobar ischaemia, and consequent infarction
or gangrene if left untreated. If the condition is not
promptly recognised, it may lead to rapid deterioration
(eg, shock and sepsis) and death.[3] [4] The most common
predisposing factor for lobar torsion is recent right upper
lobectomy. This accounted for three-quarters of cases in
a literature review[5] and was the preceding event in both
patients illustrated in this case report.
Several radiographic signs have been described for
pulmonary torsion, including rapid opacification of an
ipsilateral lobe after lobectomy; unusual position or
change in position of an opacity representing a collapsed
or consolidated lobe; displacement of the hilum in an
inappropriate direction for that collapsed lobe; and
abnormal position and direction of pulmonary vascular
markings.[3] In right middle lobe torsion, a wedge-shaped
opacity at the right side of the mediastinum is seen,
with a sharp oblique demarcation as a result of inverted
horizontal fissure.[1] These findings may raise a suspicion
of lobar torsion. However, most patients do not present
with these classic findings. Further evaluation with
contrast CT is helpful to confirm the diagnosis.
Previously described CT findings include bronchial
obstruction, hilar displacement, and unusual fissure
configuration.[6] Bronchial obstruction is not specific
since it may occur from mucus impaction or a blood
clot. Evaluation of fissure orientation and hilar position
is challenging due to altered anatomy after surgery.
More specific findings include poor enhancement of the
involved lung parenchyma and abnormal configuration
with twisting of hilar structures.
In CT pulmonary angiograms, the configuration of the
pulmonary artery and branches can be evaluated. Cases
of right middle lobe torsion can demonstrate vascular
swirling on axial images. A specific imaging sign,
the antler sign, was described in a recent study where
pulmonary arteries were abnormally curved with all
branches arising on the same side of the artery. However,
it is only demonstrated in non-right middle lobe torsion.[7]
For better evaluation of pulmonary vasculature, three-dimensional
reconstructions can be potentially useful to
demonstrate twisting.[8]
In our two cases, diagnosis of lobar torsion was made
on the basis of both imaging and bronchoscopy findings.
Conventionally, patients with suspected lobar torsion will undergo optical bronchoscopy, as in our two
cases. On optical bronchoscopy, a twisted or occluded
bronchus may present with a “fish mouth” appearance.[2]
Niekel et al[1] raised the possibility of CT bronchoscopy
from reformatted images, which can potentially obviate
the need for further bronchoscopy that may delay surgical
management. Gutiérrez Ramírez et al[9] have reported the
use of CT virtual bronchoscopy with good correlation
with optical bronchoscopy in a case of right middle
lobe torsion. If CT virtual bronchoscopy can replace
conventional bronchoscopy, the time to diagnosis and
surgery may be shortened, increasing the chance of lobe
salvage. Nonetheless validation of the accuracy of CT
virtual bronchoscopy in such a setting warrants further
evaluation.
CONCLUSION
Awareness of lung torsion is crucial for prompt
diagnosis and management. Early diagnosis may
lead to salvage of the lobe before infarction occurs,
especially for patients with marginal preoperative
pulmonary function, and thus reduce morbidity and
mortality. Radiologists should be aware of possible
imaging findings, especially the specific radiological
signs such as poor parenchymal enhancement and
abnormal twisting of hilar structures. Additionally,
evaluation of pulmonary vasculature with three-dimensional
reformatted images can offer potential
benefit in diagnosis. Whether CT virtual bronchoscopy is adequate to replace conventional bronchoscopy
requires further research.
REFERENCES
1. Niekel MC, Horsch AD, vd Ven M, Reijnen MM, Joosten FB.
Right middle lobe torsion: evaluation with CT angiography. Emerg
Radiol. 2009;16:387-9. Crossref
2. Apostolakis E, Koletsis EN, Panagopoulos N, Prokakis C, Dougenis
D. Fatal stroke after completion pneumonectomy for torsion of left
upper lobe following left lower lobectomy. J Cardiothorac Surg.
2006;1:25. Crossref
3. Felson B. Lung torsion: radiographic findings in nine cases.
Radiology. 1987;162:631-8. Crossref
4. Ziarnik E, Grogan EL. Postlobectomy early complications. Thorac
Surg Clin. 2015;25:355-64. Crossref
5. Dai J, Xie D, Wang H, He W, Zhou Y, Hernández-Arenas LA, et al.
Predictors of survival in lung torsion: a systematic review and
pooled analysis. J Thorac Cardiovasc Surg. 2016;152:737-45.e3. Crossref
6. Kim EA, Lee KS, Shim YM, Kim J, Kim K, Kim TS, et al.
Radiographic and CT findings in complications following
pulmonary resection. Radiographics. 2002;22:67-86. Crossref
7. Hammer MM, Madan R. Clinical and imaging features in lung torsion and description of a novel imaging sign. Emerg Radiol.
2018;25:121-7. Crossref
8. Chung SH, Nam JE, Choe KO, Choi BW, Hur J, Lee HJ, et al. Radiologic findings of lung lobe torsion in reconstructed
multidetector computed tomography image lead to early detection.
Clin Imaging. 2010;34:400-3. Crossref
9. Gutiérrez Ramírez MC, Rodríguez Sánchez D, Ros Lucas JA. Torsion of middle lobe after lobectomy. Correlation between optical
bronchoscopy-computed tomography virtual bronchoscopy. Arch
Bronconeumol. 2015;51:355. Crossref
| Attachment | Size |
|---|---|
| v24n1_Post.pdf | 288.73 KB |