Radiological Findings of Falciform Ligament Necrosis: A Case Report
CASE REPORT
Radiological Findings of Falciform Ligament Necrosis: A Case Report
C Agirgun1, H Vehbi2, F Agirgun1, H Kocabas3
1 Department of Radiology, Bartin Government Hospital, Bartin, Turkey
2 Department of Radiology, Istanbul Medipol University Hospital, Istanbul, Turkey
3 Department of General Surgery, Bartin Government Hospital, Bartin, Turkey
Correspondence: Asst. Prof. Dr H Vehbi, Department of Radiology, Istanbul Medipol University Hospital, Istanbul, Turkey. Email: wehbihusam@gmail.com
Submitted: 12 Jan 2019; Accepted: 13 Mar 2019.
Contributors: All authors contributed to the design of the study; acquisition and analysis of the data; drafting of the manuscript; and critical
revision of the manuscript for important intellectual content. All authors had full access to the data, contributed to the study, approved the final
version for publication, and take responsibility for its accuracy and integrity.
Conflicts of Interest: The authors have no conflicts of interest to declare.
Funding/Support: This case report received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics Approval: The patient was treated in accordance with the Declaration of Helsinki. The patient provided informed consent for all treatments and procedures.
INTRODUCTION
The falciform ligament is a sickle-shaped peritoneal
ligament between the liver, the diaphragm and the
anterior abdominal wall. Falciform ligament necrosis
is a rare cause of right upper quadrant pain that is
often misdiagnosed.[1] [2] We present a case of right
upper quadrant pain caused by fatty necrosis of the
falciform ligament seen during ultrasound exam and
confirmed by contrast-enhanced computed tomography
(CT) scan. Very few cases have been reported and
correlation between CT and ultrasound findings are
rarely discussed.
CASE PRESENTATION
A 35-year-old man was admitted to the emergency
department of our hospital with right upper quadrant
pain, epigastric tenderness, and fever. He was referred to
our radiology department with suspected cholecystitis.
The patient and family history were non-specific.
Physical examination revealed right quadrant tenderness
and positive Murphy’s sign. There was no history of drug
use. Blood tests showed increased white blood cell count
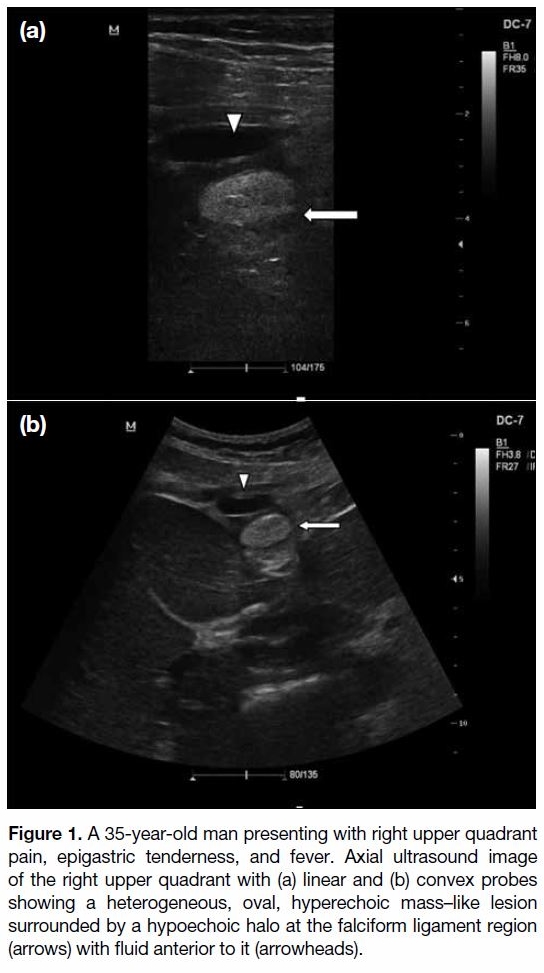
and C-reactive protein levels with normal liver function parameters. Abdominal ultrasound examination showed
an echogenic non-compressible lesion located between
the two lobes of the liver in the falciform ligament region
surrounded by fluid. The gallbladder, liver parenchyma,
and other components were normal (Figure 1) as were
the intrahepatic and common bile ducts.
Figure 1. A 35-year-old man presenting with right upper quadrant
pain, epigastric tenderness, and fever. Axial ultrasound image
of the right upper quadrant with (a) linear and (b) convex probes
showing a heterogeneous, oval, hyperechoic mass–like lesion
surrounded by a hypoechoic halo at the falciform ligament region
(arrows) with fluid anterior to it (arrowheads).
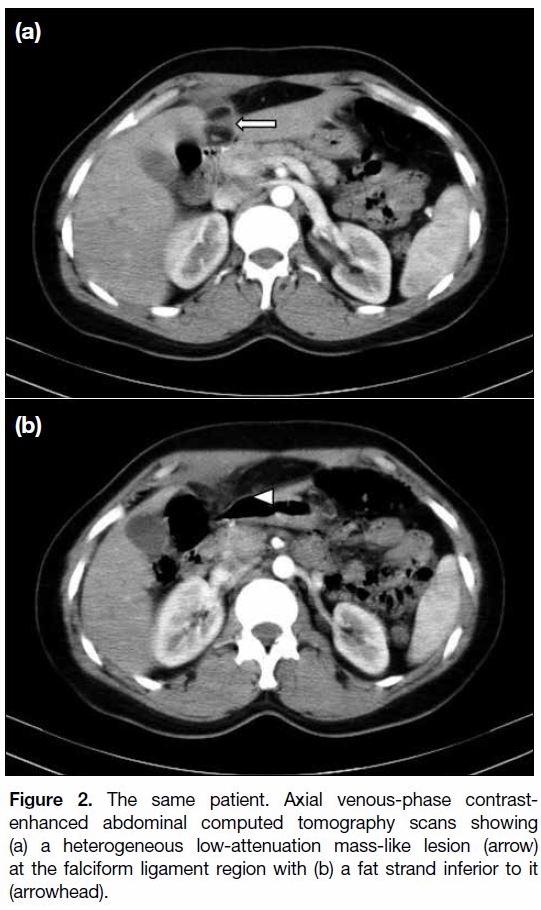
Abdominal CT scan demonstrated a low-density ovalshaped
heterogeneous mass at the falciform ligament
surrounded by inflammatory changes, fat stranding and
minimal free fluid consistent with falciform ligament
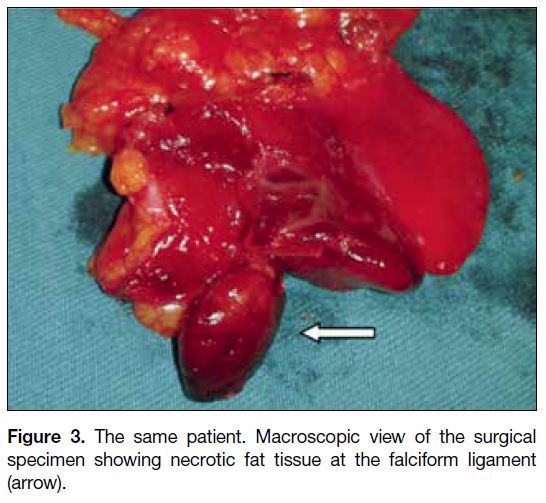
necrosis (Figure 2). Surgical intervention and excision
of the falciform ligament was performed and confirmed
the radiological diagnosis (Figure 3). The patient
experienced no complications and was discharged
after 3 days. Histopathological examination revealed
haemorrhagic areas and fatty necrosis of the falciform
ligament.
Figure 2. The same patient. Axial venous-phase contrast-enhanced
abdominal computed tomography scans showing
(a) a heterogeneous low-attenuation mass-like lesion (arrow)
at the falciform ligament region with (b) a fat strand inferior to it
(arrowhead).
Figure 3. The same patient. Macroscopic view of the surgical specimen showing necrotic fat tissue at the falciform ligament (arrow).
DISCUSSION
The falciform ligament is a sickle-shaped area of the
peritoneum that divides the right and the left subphrenic
compartments. It is a remnant of the ventral fetal mesentery that contains the paraumbilical veins, ligament
teres, fatty tissue, and muscular fibres. Its arterial blood
supply derives from the middle or left hepatic artery and
drains into the portal or paraumbilical veins.[1] [2] [3]
Falciform ligament pathologies are rare. Inflammation
or necrosis of this ligament can be seen in infants
secondary to omphalitis. Other rare pathologies such
as lipoma, cysts, leiomyosarcoma, lymphangioma,
and paraganglioma have also been recorded.[4] [5] Rarely
falciform ligament inflammation and abscess formation
are seen as a complication of cholecystitis, or following
instrumentation during laparoscopic surgery.[6]
Falciform ligament necrosis is a very rare cause of acute abdominal pain that is often misdiagnosed. To the best of our knowledge, very few cases have been reported
in the literature and most had no accurate preoperative
diagnosis.[7] Clinical presentation is similar to that of
acute cholecystitis, perforated duodenal ulcer, and
pancreatitis. Infection, torsion of the ligament, venous
thrombosis and arterial embolisation are the main causes
of this condition, as is septic thromboembolism.[8]
In recent years, there has been an increase in diagnosis
of intraperitoneal fat tissue and falciform ligament
pathologies due to the increased availability and use
of advanced imaging modalities. Ultrasound and CT
play a vital role in the diagnosis of falciform ligament
pathologies. Ultrasound examination accurately reveals
fatty necrosis of the falciform ligament. Use of a linear
probe after convex probe in suspicious cases enables
a clearer view of the ligament and may reveal an oval
hyperechoic mass with a hypoechoic halo in the falciform
ligament region. (Figure 1). However, solitary fibrous
tumours, lipoma and ligament haemorrhage should be
considered as differential diagnoses.
CT scan is a very specific imaging tool for diagnosing
abdominal pathologies and their complications.[5] [9]
Technical advances with multidetector CT allow
multiplanar reformats and volume rendering. These
reformats allow us to detect the falciform ligament in
coronal sagittal planes and in the traditional transverse
plane. Thin slices and multiple acquisitions allow more
high-resolution images per tube rotation that be can
be combined to create three-dimensional images and
reformats, greatly increasing the diagnostic capability of
CT scan. During CT scan, fatty necrosis of the falciform
ligament presents as an oval fatty mass without contrast
enhancement, with fluid and inflammatory changes
around it.
Magnetic resonance imaging may provide an alternative
imaging modality to diagnose falciform ligament
pathologies. Using different sequences including the
fat suppression ones enable differentiation between
fat tissue, bleeding, and effusion.[7] Nonetheless its
susceptibility to artefacts of motion and organ pulsation may limit its use in abdominal imaging.
Treatment is generally surgical excision although
conservative treatment has been reported in some
cases.[10] Our patient underwent surgical excision with no
complications and was discharged 3 days later.
CONCLUSION
Fatty necrosis of the falciform ligament is a very rare
cause of acute abdominal pain. Although it is easily
diagnosed by ultrasound and CT scan, many clinicians
and radiologists are unfamiliar with the condition. The
falciform ligament region should be carefully examined
in patients with right upper quadrant pain. Surgical
excision is the treatment of choice although conservative
treatment is successful in some cases.
REFERENCES
1. Standring S, editor. Gray’s Anatomy, 39th edition. Emerg Med J. 2006;23:492. Crossref
2. Ozkececı ZT, Ozsoy M, Celep B, Bal A, Polat C. A rare cause of
acute abdomen: an isolated falciform ligament necrosis. Case Rep
Emerg Med. 2014;2014:570751. Crossref
3. Webber CE Jr, Glanges E, Crenshaw CA. Falciform ligament. A
possible twist? Arch Surg. 1977;112:1264. Crossref
4. Koca YS, Okur N, Barut İ. Isolated falciparum ligament
necrosis causing right upper quadrant pain. Turk J Gastroenterol.
2017;28:531-2. Crossref
5. Lloyd T. Primary torsion of the falciform ligament: computed
tomography and ultrasound findings. Australas Radiol 2006;50:252-
4. Crossref
6. Lim ZS, Tan JY, Fanning S, Mitchell B. Education and imaging.
Hepatobiliary and pancreatic: falciform ligament necrosis. J
Gastroenterol Hepatol. 2012;27:1409. Crossref
7. Maccallum C, Eaton S, Chubb D, Franzi S. Torsion of fatty
appendage of falciform ligament: acute abdomen in a child. Case
Rep Radiol. 2015;2015:293491. Crossref
8. Czymek R, Bouchard R, Hollmann S, Kagel C, Frank A,
Bruch HP, et al. First complete laparoscopic resection of a
gangrenous falciform ligament. Eur J Gastroenterol Hepatol.
2010;22:109-11. Crossref
9. Coulier B, Cloots V, Ramboux A. US and CT diagnosis of a twisted
lipomatous appendage of the falciform ligament. Eur Radiol.
2001;11:213-5. Crossref
10. Nam JG, Choi SH, Kang BS, Kim JY, Kwon WJ. Serial ultrasound
and computed tomography findings of torsion of lipomatous
appendage of the falciform ligament in a child treated by
conservative management. J Korean Soc Radiology. 2015;72:368-
71. Crossref