Congenital Absence of Left Circumflex Coronary Artery: Role of Computed Tomography Coronary Angiography
PR Kapur, R Jain, GP Vashist
Hong Kong J Radiol 2014;17:e1-4
DOI: 10.12809/hkjr1412126
ABSTRACT
Congenital coronary artery anomalies are infrequently seen during coronary angiography, and are usually diagnosed incidentally. Among such anomalies, absence of the left circumflex artery is extremely rare. We report on a 49-year-old man who presented with a 2-month history of increasing exertional breathlessness and was found to have poor left ventricular function on echocardiography. Routine coronary angiography showed a normal left anterior descending, no left circumflex artery and a dominant right coronary artery. Neither aortography nor pulmonary angiography showed a separate ostium for the left circumflex artery. Multi-detector computed tomographic coronary angiography was performed to confirm the diagnosis of congenital absence of the left circumflex artery.
中文摘要
左冠狀動脈迴旋支先天缺如:CT冠狀動脈造影的作用
PR Kapur、R Jain、GP Vashist
先天性冠狀動脈異常於冠狀動脈造影中很少見,通常為偶然發現。在冠狀動脈異常的病例中,左迴旋支先天缺如極為罕見。本文報告一名49歲男子,病發時出現勞力性呼吸困難已達兩個月,超聲心動圖顯示左心室功能差。常規冠狀動脈造影顯示正常左前降支,無左迴旋支和優勢右冠狀動脈。無論是主動脈造影或肺動脈造影都未能顯示左迴旋支獨立開口。後進行多切面電腦斷層造影以確診病人的左迴旋支先天缺如。
INTRODUCTION
Congenital absence of the left circumflex artery (LCX) is very rare; only a few case reports exist in the literature. In most patients, this is discovered incidentally during imaging studies like coronary angiography, and most are asymptomatic.1 However, association with vasospastic angina, infarction, and systolic click syndrome have been described, which may be life-threatening.2 3 4 We report the case of a 49-year-old male who presented with recent worsening of dyspnoea on exertion and was found to have poor left ventricular function on echocardiography. Routine coronary angiography showed a normal left anterior descending (LAD) artery, no LCX, and a dominant right coronary artery (RCA). Neither aortography nor pulmonary angiography showed a separate ostium for the LCX. A dilated left atrium and left ventricle with left ventricular ejection fraction of 36% were noted.
Multi-detector computed tomography (MDCT) was performed to confirm the diagnosis. To the best of our knowledge this is a second report of its kind, in which this anomaly was associated with myopathy. In such cases, precise morphological and functional evaluation is warranted to guide treatment and gauge the prognosis.
CASE REPORT
A 49-year-old man with known chronic obstructive pulmonary disease presented with a 2-month history of increasing breathlessness on exertion in May 2011. He did not have diabetes or hypertension. Physical exam-ination revealed a well-nourished male with a pulse rate of 72 beats/min, blood pressure of 100/80 mm Hg, and peripheral arterial oxygen saturation of 98%. Peripheral pulses were normal. Routine investigations yield no significant lipid profile abnormality. Cardiac auscultation revealed regular heart sounds and a left ventricular third sound (S3). His chest X-ray showed no abnormality. His 12-lead electrocardiogram showed left axis deviation and two-dimensional echocardiography revealed global hypokinesia with a dilated left atrium and left ventricle, and a left ventricular ejection fraction of 36%.
Selective coronary angiography via the radial artery approach revealed the left main and LAD coronary arteries that appeared normal, and their small-sized diagonal vessels showed 50% and 70% mid and ostial stenoses, respectively. The RCA was a large super dominant vessel which crossed the left atrioventricular (AV) groove and supplied the inferior and posterolateral walls of the left ventricle, but showed no discrete stenosis. The LCX was not visualised. Aortic root and pulmonary angiography did not reveal any anomalous coronary artery. A nuclear-medicine myocardial perfusion scan with Thallium-201 was normal. However, angiography using a 64-slice MDCT performed on the following day confirmed absence of the LCX. The posterior descending artery and posterior left ventricle (PLV) were prominent; the PLV supplied the posterolateral wall of the left ventricle (Figures 1, 2, 3).
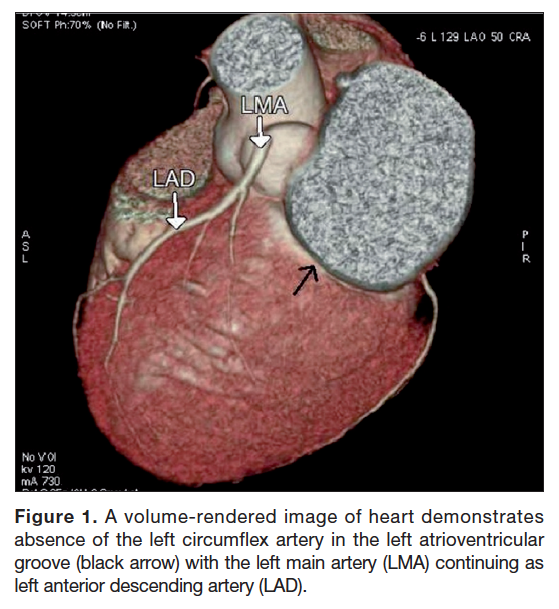
Figure 1. A volume-rendered image of heart demonstrates absence of the left circumflex artery in the left atrioventricular groove (black arrow) with the left main artery (LMA) continuing as left anterior descending artery (LAD).
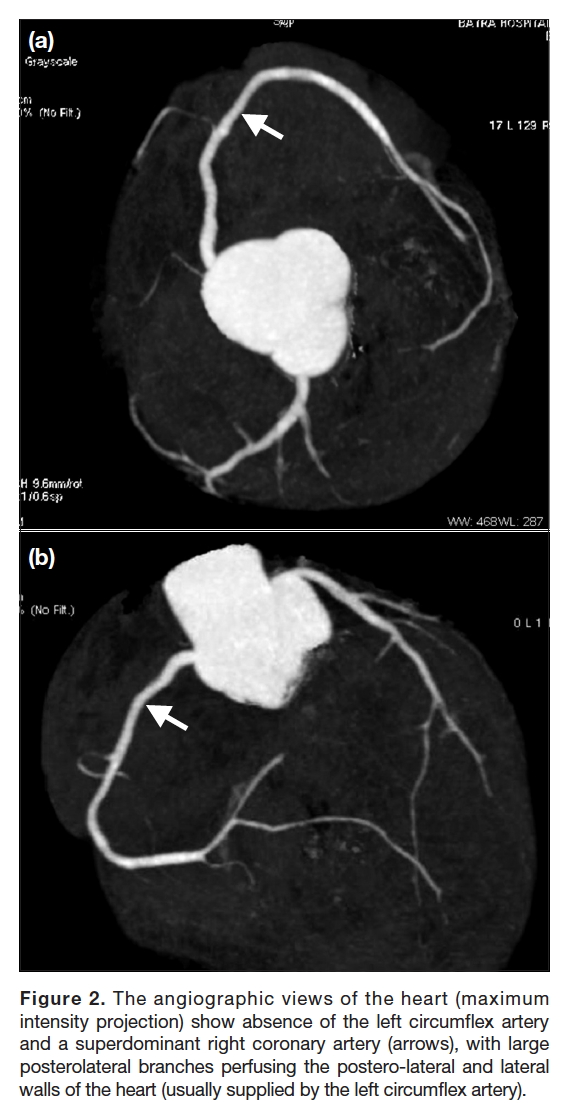
Figure 2. The angiographic views of the heart (maximum intensity projection) show absence of the left circumflex artery and a superdominant right coronary artery (arrows), with large posterolateral branches perfusing the postero-lateral and lateral walls of the heart (usually supplied by the left circumflex artery).
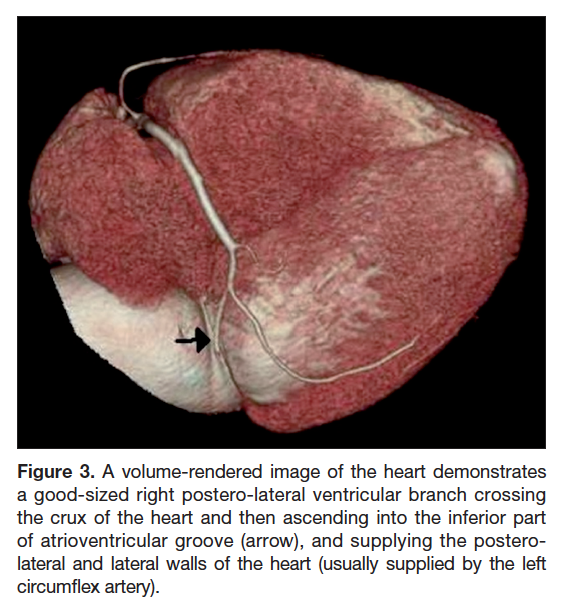
Figure 3. A volume-rendered image of the heart demonstrates a good-sized right postero-lateral ventricular branch crossing the crux of the heart and then ascending into the inferior part of atrioventricular groove (arrow), and supplying the postero-lateral and lateral walls of the heart (usually supplied by the left circumflex artery).
DISCUSSION
Congenital coronary artery anomalies are seen rarely, and have been reported to occur in 0.64% to 1.3% of patients undergoing angiography.1 5
Congenital absence of the LCX is a vascular anomaly in which the artery fails to develop in the AV groove.6 7 8 Yamanaka and Hobbs1 found it in only four of 126,595 patients who underwent coronary angiography between 1960 and 1988, yielding a frequency of only 0.003% in all the patients, and 0.24% in those with other coronary artery anomalies. Separate origins of the LAD and LCX from the left sinus of valsalva were the most common anomalies, and occurred in about 0.41% of the patients studied. Anomalous origin of the LCX from the right sinus of Valsalva or the RCA was reported by Ueyama et al6 and Page et al9 with a frequency of 0.39% and 0.67%, respectively. Ott et al10 reported a rare patient with an ectopic LCX originating from the right pulmonary artery.
In 1984, Bestetti et al11 described the first autopsied case of congenital absence of the LCX in a 12-year-old girl clinically diagnosed as having idiopathic cardiomyopathy. The coexistence of the two conditions was postulated to be incidental. To the best of our knowledge, ours is the second report of an absent LCX and dilated cardiomyopathy in the world literature.
There could be an association between the two conditions in patients with coronary artery hypoplasia (which could occur with an absent LCX and poorly developed RCA) that may give rise to myocardial fibrosis due to chronic ischaemia in the area of myocardial hypoperfusion and lead to a dilated cardiomyopathy.12 However, in the case reported by Bestetti et al,11 the pathological findings did not support any such association. In our patient too, cardiomyopathy also appears to be incidental, as myocardial perfusion imaging showed nil normal. The degree of stenosis in the minor vessels of our patient cannot account for the global hypokinesia and poor left ventricular function.
Conventional cardiac catheterization is a well-known modality for the detection of coronary anomalies. However, MDCT is emerging as an essential imaging tool for this purpose, as many congenital coronary anomalies are more easily assessed using this modality.13 Notably, MDCT is well suited to detect and define the anatomical course of coronary artery anomalies and their relationship to other cardiac and non-cardiac structures, because of the three-dimensional nature of the images it provides. This makes CT angiography an imaging modality of choice for the investigation of known or suspected coronary artery anomalies.14
With CT arteriography, the frequency of this anomaly can be more accurately assessed but might not yield a particularly high frequency. Komatsu et al15 reported only two cases of this type of anomaly in their 3910 consecutive cases undergoing MDCT, yielding a frequency of 0.05%. This suggests the anomaly remains very rare, even in the era of refined investigations.
Recognition of this anomaly is important, as it may mimic atherosclerotic coronary artery disease, whereby oxygen demand in myocardium normally supplied by it are taken over by RCA and such supply may not be sufficient during increased physical activity.
CONCLUSION
Although the absence of a LCX is considered benign, its clinical relevance cannot be overlooked, as it has been associated with symptoms, myocardial infarction,3 and systolic click syndrome.4
REFERENCES
1. Yamanaka O, Hobbs RE. Coronary artery anomalies in 126,595 patients undergoing coronary arteriography. Cathet Cardiovasc Diagn. 1990;21:28-30. CrossRef
2. Yoon YK, Rha SW, Na JO, Suh SY, Choi CU, Kim JW, et al. Congenital absence of left circumflex coronary artery presented with vasospastic angina and myocardial bridge in single left coronary artery. Int J Cardiol. 2009;131:e108-11. CrossRef
3. Mievis E, Bopp P, Righetti A. Congenital absence of the circumflex artery. Association with an infarction without coronary disease [in French]. Arch Mal Coeur Vaiss. 1979;72:1155-9.
4. Gentzler RD 2nd, Gault JH, Liedtke AJ, McCann WD, Mann RH, Hunter AS. Congenital absence of the left circumflex coronary artery in the systolic click syndrome. Circulation. 1975;52:490-6. CrossRef
5. Roberts WC. Major anomalies of coronary artery origin seen in adulthood. Am Heart J. 1986;111:941-63. CrossRef
6. Ueyama K, Ramchandani M, Beall AC Jr, Jones JW. Diagnosis and operation for anomalous circumflex coronary artery. Ann Thorac Surg. 1997;63:377-81. CrossRef
7. Ilia R, Jafari J, Weinstein JM, Battler A. Absent left circumflex coronary artery. Cathet Cardiovasc Diagn. 1994;32:349-50. CrossRef
8. Baruah DK, Babu PR, Prasad S. Absent left circumflex coronary artery. Indian Heart J. 1998;50:335-6.
9. Page HL Jr, Engel HJ, Campbell WB, Thomas CS Jr. Anomalous origin of the left circumflex coronary artery. Circulation. 1974;50:768-73. CrossRef
10. Ott DA, Cooley DA, Pinsky WW, Mullins CE. Anomalous origin of circumflex coronary artery from right pulmonary artery. Report of a rare anomaly. J Thorac Carddiovasc Surg. 1978;76:190-4.
11. Bestetti RB, Costa RB, Oliviera JS, Rossi MA, Corrêa de Araujo R. Congenital absence of the circumflex coronary associated with dilated cardiomyopathy. Int J Cardiol. 1985;8:331-5. CrossRef
12. Li LX, Nohara R, Okuda K, Hosokawa R, Hata T, Tanaka M, et al. Comparative study of 201Tl-scintigraphic image and myocardial pathologic findings in patients with dilated cardiomyopathy. Ann Nucl Med. 1996;10:307-14. CrossRef
13. Kim SY, Seo JB, Do KH, Heo JN, Lee JS, Song JW, et al. Coronary artery anomalies: classification and ECG-gated multi-detector row CT findings with angiographic correlation. Radiographics. 2006;26:317-33. CrossRef
14. Schroeder S, Achenbach S, Bengel F, Burgstahler C, Cademartiri F, de Feyter P, et al. Cardiac computed tomography: indications, applications, limitations, and training requirements: report of a Writing Group deployed by the Working Group Nuclear Cardiology and Cardiac CT of the European Society of Cardiology and the European Council of Nuclear Cardiology. Eur Heart J. 2008;29:531-56. CrossRef
15. Komatsu S, Sato Y, Ichikawa M, Kunimasa T, Ito S, Takagi T, et al. Anomalous coronary arteries in adults detected by multislice computed tomography: presentation of cases from multicenter registry and review of the literature. Heart Vessels. 2008;23:26-34. CrossRef

